Check out our new preprint: SARS-CoV-2 infections elicit higher levels of original antigenic sin antibodies compared to SARS-CoV-2 mRNA vaccinations
1/
medrxiv.org/content/10.110…
1/
medrxiv.org/content/10.110…
We found that both SARS-CoV-2 infections and mRNA vaccinations elicit antibodies that bind to the S1 and S2 regions of the SARS-CoV-2 spike. 2nd doses of vaccine primarily boost antibodies reactive to S1.
2/
2/

Here is where it gets interesting: SARS-CoV-2 infections boost antibodies that react to the S2 region of OC43 (a related seasonal coronavirus). SARS-CoV-2 mRNA vaccines boost OC43-reactive antibodies less than infection.
3/
3/

Even though SARS-CoV-2 infections efficiently boost OC43-reactive antibodies, these antibodies paradoxically do not bind to SARS-CoV-2 antigens in absorption assays. So, the OC43-reactive antibodies boosted by infection have a very low affinity for SARS-CoV-2.
4/
4/

We found that mRNA vaccines elicit antibodies that behave very differently in these absorption assays. The OC43-reactive antibodies boosted by SARS-CoV-2 mRNA vaccines efficiently bind to both OC43 and SARS-CoV-2 antigens. These antibodies are truly cross-reactive.
5/
5/

These studies show that SARS-CoV-2 mRNA vaccines elicit fundamentally different antibody responses compared to SARS-CoV-2 infections. Infections elicit higher levels of OC43 antibodies, but these bind poorly to SARS-CoV-2.
6/
6/

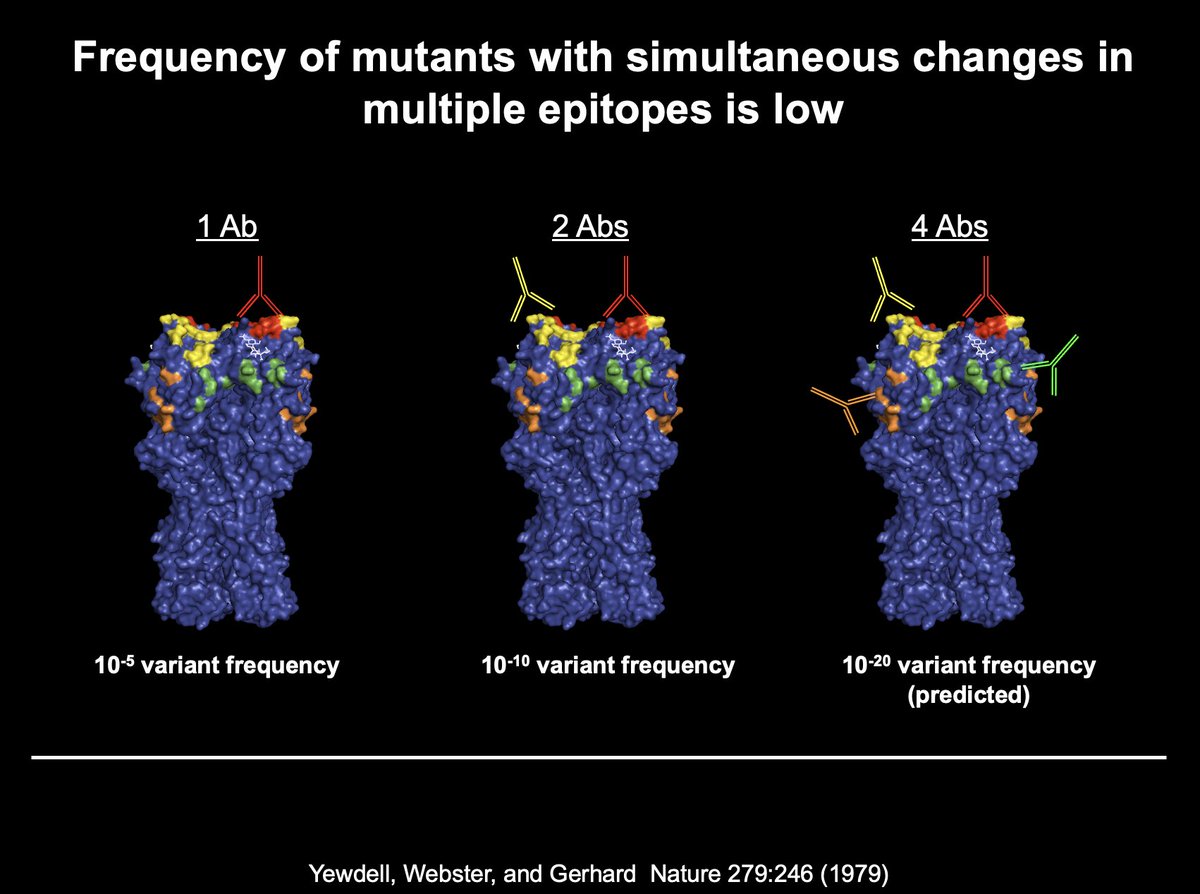
How does this happen? We think that antigenically distinct viruses engage memory B cells elicited by prior infections through multiple low affinity interactions with thousands of B cell receptors on memory B cells.
7/
7/
What is the consequence of SARS-CoV-2 infections boosting low affinity OC43-reactive S2 Abs? The short answer is that we don't know. Could this compromise de novo responses? Or maybe the recall of OC43-reactive B cells is a good thing, because these cells can then adapt.
8/
8/
It is fascinating that mRNA vaccines elicit antibodies that bind efficiently to both OC43 and SARS-CoV-2. We think that long-lived germinal centers elicited by mRNA vaccines create a lush environment where B cells primed by past OC43 exposures can adapt.
9/
9/
At the end of the day, all of these findings are consistent with Thomas Francis' doctrine of original antigen sin. Francis figured out a lot of this over 60 years ago with a lab filled with red blood cells and crude virus isolates.
10/
10/
This is another great collaboration with many labs at @PennMedicine.
@penn really is a special place.
11/11
@penn really is a special place.
11/11
• • •
Missing some Tweet in this thread? You can try to
force a refresh