#EACTS2021
This is a 🧵all about Transcatheter Mitral Valve Implantation (TMVI). If you don't know a lot about this and want to learn more - read on! This is a summary of a great expert focus session
First talk from Dr Gry Dahle (Oslo), on why TMVI is not the same as TAVI
This is a 🧵all about Transcatheter Mitral Valve Implantation (TMVI). If you don't know a lot about this and want to learn more - read on! This is a summary of a great expert focus session
First talk from Dr Gry Dahle (Oslo), on why TMVI is not the same as TAVI
#EACTS2021
1st TAVI was done 10 years before 1st TMVI
TAVI has revolutionised treatment of aortic stenosis; TMVI is further behind largely due to anaromical complexity of treating the MV compared to the AV - the AV valves are much more complex than the semilunar valves!

1st TAVI was done 10 years before 1st TMVI
TAVI has revolutionised treatment of aortic stenosis; TMVI is further behind largely due to anaromical complexity of treating the MV compared to the AV - the AV valves are much more complex than the semilunar valves!


#EACTS2021
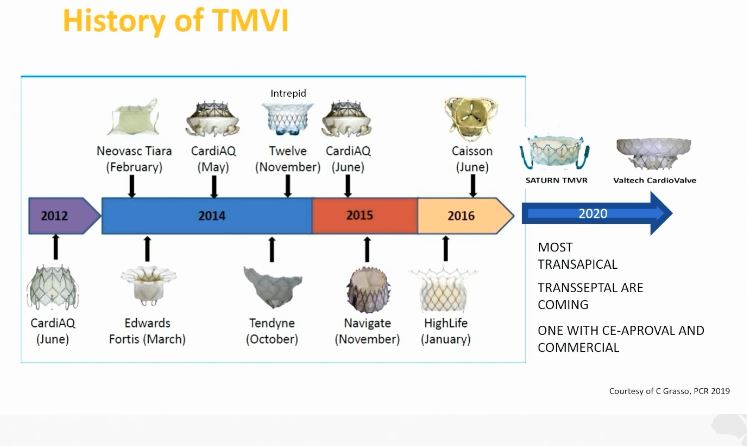
Historical timeline of the TMVI journey (left) and the large number of devices still competing for approval in the transcatheter mitral space (right)
@GilbertTangMD @mrjzacharias @BISMICS @SCTSUK @BrHeartValveSoc

Historical timeline of the TMVI journey (left) and the large number of devices still competing for approval in the transcatheter mitral space (right)
@GilbertTangMD @mrjzacharias @BISMICS @SCTSUK @BrHeartValveSoc

#EACTS2021
Just like TAVI, pre-procedural imaging is vital for TMVI. However, unlike TAVI, much more detail is required around the valve anatomy & subvalvular apparatus, as well as LV size / shape, LVOT size etc
Just like TAVI, pre-procedural imaging is vital for TMVI. However, unlike TAVI, much more detail is required around the valve anatomy & subvalvular apparatus, as well as LV size / shape, LVOT size etc

#EACTS2021
OK, the echo talk was given by Royal Brompton stalwart @AlisonD61630805
A great overview for echo enthusiasts
OK, the echo talk was given by Royal Brompton stalwart @AlisonD61630805
A great overview for echo enthusiasts

#EACTS2021
Lots of things to consider, including whether the patient is suitable initially for transcatheter edge-edge repair (TEER).
Lots of things to consider, including whether the patient is suitable initially for transcatheter edge-edge repair (TEER).

#EACTS2021
Here, Alison explains the inclusion criteria for a Tendyne procedure. LV cannot be too big (<7cm) or too poor in function (EF >30% only) with no or minimal annular calcium
Predominantly for primary MR patients unsuitable for surgery or TEER
Can be used in 2o MR also

Here, Alison explains the inclusion criteria for a Tendyne procedure. LV cannot be too big (<7cm) or too poor in function (EF >30% only) with no or minimal annular calcium
Predominantly for primary MR patients unsuitable for surgery or TEER
Can be used in 2o MR also


#EACTS2021
Initial TTE important to look at anatomy and physiology, paying special attention to RV size and function also


Initial TTE important to look at anatomy and physiology, paying special attention to RV size and function also



#EACTS2021
3D-TOE of course allows for even better assessment of the MV, including checking for presence of clefts and confirming exact scallop pathology
3D-TOE of course allows for even better assessment of the MV, including checking for presence of clefts and confirming exact scallop pathology

#EACTS2021
Need to ensure the MV annulus is neither too large nor too small
Measure using biplane view on TOE in end-systole
Need to ensure the MV annulus is neither too large nor too small
Measure using biplane view on TOE in end-systole

#EACTS2021
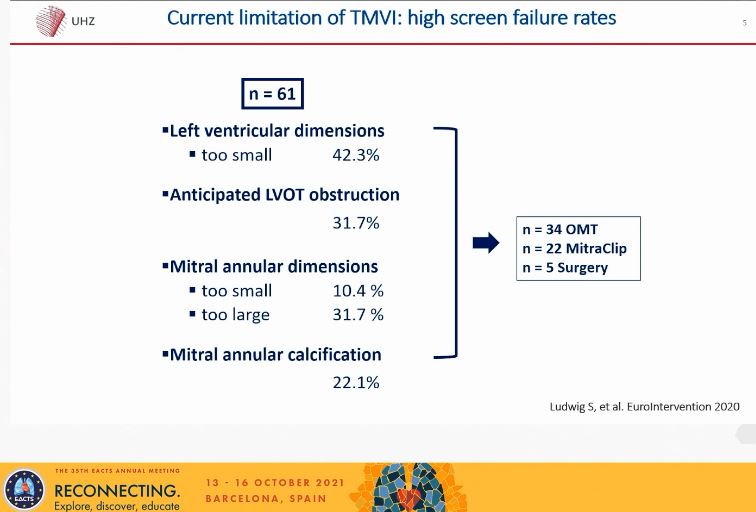
Patients may be deemed unsuitable for TMVI due to imaging considerations, either by echo or CT or both
Some examples of why patients had suffered screen failures in their centre were shared here
Patients may be deemed unsuitable for TMVI due to imaging considerations, either by echo or CT or both
Some examples of why patients had suffered screen failures in their centre were shared here
#EACTS2021
Next, a specific talk on the Tendyne system from Dr David Muller in Australia
Started by explaning what the Tendyne system is: the apical pad helps not just anchor the device and provide stability but also with haemostasis

Next, a specific talk on the Tendyne system from Dr David Muller in Australia
Started by explaning what the Tendyne system is: the apical pad helps not just anchor the device and provide stability but also with haemostasis


#EACTS2021
This is the appearance of the device on echo once deployed on 3D (left) and 2D imaging (right) with laminar flow across the valve
This is the appearance of the device on echo once deployed on 3D (left) and 2D imaging (right) with laminar flow across the valve

#EACTS2021
Next, data from the Tendyne CE mark study. 191 patients
Mean age 74
Mean STS score 7.7%
Mean LVEF 44%
~70% NYHA Class III / IV HF
88% had 2o MR
Lots of co-morbidity
30-day mortality ~8%
90-day mortality ~16%

Next, data from the Tendyne CE mark study. 191 patients
Mean age 74
Mean STS score 7.7%
Mean LVEF 44%
~70% NYHA Class III / IV HF
88% had 2o MR
Lots of co-morbidity
30-day mortality ~8%
90-day mortality ~16%


#EACTS2021
Next talk on the Tiara device, by Prof Anson Cheung from Vancouver
Tiara is a transapical valve that comes in 2 sizes (35mm & 40mm) and has anchors that aim to capture the native AMVL, reducing risk of SAM and LVOTO


Next talk on the Tiara device, by Prof Anson Cheung from Vancouver
Tiara is a transapical valve that comes in 2 sizes (35mm & 40mm) and has anchors that aim to capture the native AMVL, reducing risk of SAM and LVOTO



#EACTS2021
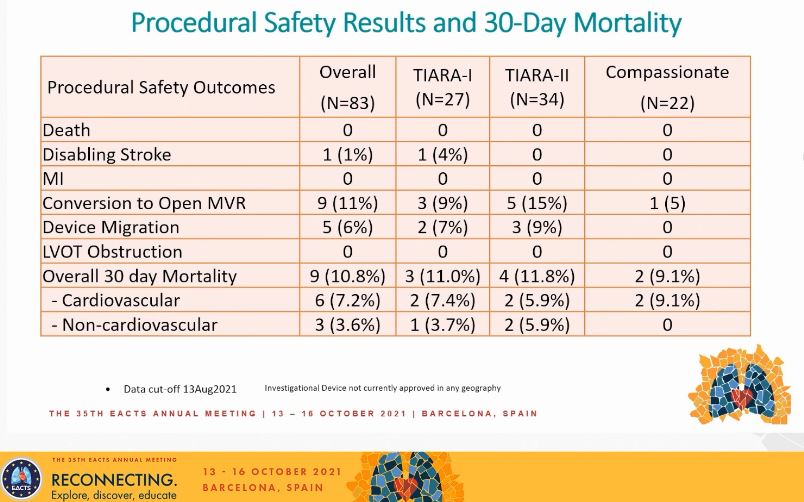
TIARA I was the early feasibility study, now on to TIARA II
Recruitment hampered significantly by COVID-19, hence only 83 implants to date
TIARA I was the early feasibility study, now on to TIARA II
Recruitment hampered significantly by COVID-19, hence only 83 implants to date

#EACTS2021
Tiara outcomes here. No immediate procedural mortality. Successful deployment & correct position in 93% cases. Overall short-term outcomes show promise

Tiara outcomes here. No immediate procedural mortality. Successful deployment & correct position in 93% cases. Overall short-term outcomes show promise

#EACTS2021
Conclusion slide - the longest survivor is already >7 years out from surgery!
Will be interesting to see how this fares in the future against Tendyne, which has 10 times as many implants worldwide so far. Is there room for both systems? Probably...
Conclusion slide - the longest survivor is already >7 years out from surgery!
Will be interesting to see how this fares in the future against Tendyne, which has 10 times as many implants worldwide so far. Is there room for both systems? Probably...

#EACTS2021
Next talk from @m_taramasso on TMVI in 2 special situations:
1. Mitral annular calcification (MAC)
2. Previous SAVR / TAVI procedure
Started by reminding us that valve-in-MAC is not good, not bad but ugly!

Next talk from @m_taramasso on TMVI in 2 special situations:
1. Mitral annular calcification (MAC)
2. Previous SAVR / TAVI procedure
Started by reminding us that valve-in-MAC is not good, not bad but ugly!


#EACTS2021
Valve-in-MAC has a worse outcome than valve-in-ring and valve-in-valve...why?
Up to 40% can develop LVOTO...that will be a major factor

Valve-in-MAC has a worse outcome than valve-in-ring and valve-in-valve...why?
Up to 40% can develop LVOTO...that will be a major factor


I reached the end of a thread!
Final tweet in this thread - data of n=11 from Tendyne system in MAC shows some promise...and prior AVR/TAVI should not be considered a contra-I to TMVI
See you all tomorrow!
#EACTS2021 @EACTS @rafasadaba



Final tweet in this thread - data of n=11 from Tendyne system in MAC shows some promise...and prior AVR/TAVI should not be considered a contra-I to TMVI
See you all tomorrow!
#EACTS2021 @EACTS @rafasadaba




• • •
Missing some Tweet in this thread? You can try to
force a refresh