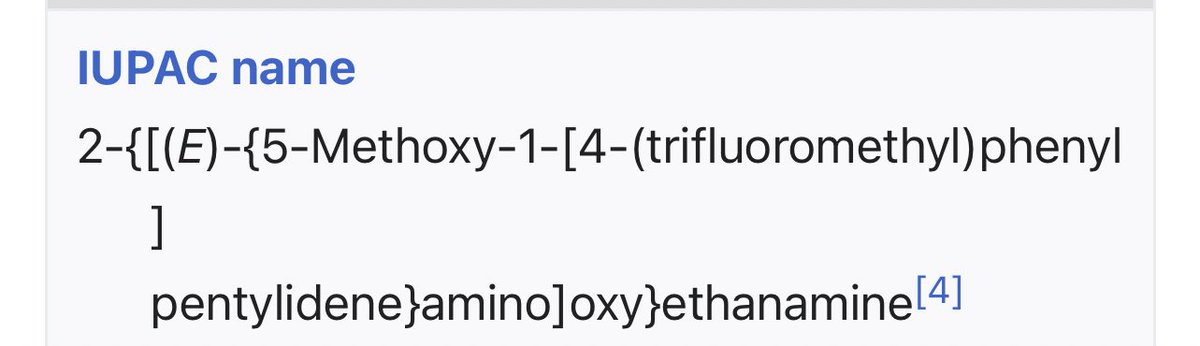
All SSRIs contain fluoride.
Sertraline (Zoloft) is the only exception.
• • •
Missing some Tweet in this thread? You can try to
force a refresh