#EACTS2021
This 🧵is related to Thursday's symposium on Edwards' Inspiris Resilia aortic bioprosthetic valve
The hospital in which I work used this valve for ~2yrs before stopping, so I was intrigued to hear the experts
A thought-provoking session!
@rafasadaba @GilbertTangMD
This 🧵is related to Thursday's symposium on Edwards' Inspiris Resilia aortic bioprosthetic valve
The hospital in which I work used this valve for ~2yrs before stopping, so I was intrigued to hear the experts
A thought-provoking session!
@rafasadaba @GilbertTangMD

#EACTS2021
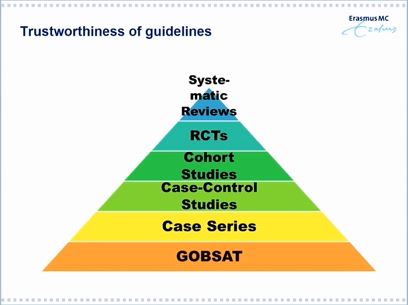
First talk from Prof Takkenberg, who needs no introduction to any of you. A very important talk in which she questioned the primacy of RCTs and spoke up on the importance of 'real world' registry data, often dismissed as poor quality
First talk from Prof Takkenberg, who needs no introduction to any of you. A very important talk in which she questioned the primacy of RCTs and spoke up on the importance of 'real world' registry data, often dismissed as poor quality

#EACTS2021
I learnt a new acronym today - GOBSAT!
Good Old Boys Sat Around the Table!
i.e. expert consensus, LoE - C! Love it!
She emphasised that a lot of our evidence, esp in VHD, is GOBSAT!
@mirvatalasnag @mrjzacharias

I learnt a new acronym today - GOBSAT!
Good Old Boys Sat Around the Table!
i.e. expert consensus, LoE - C! Love it!
She emphasised that a lot of our evidence, esp in VHD, is GOBSAT!
@mirvatalasnag @mrjzacharias

#EACTS2021
Correctly, she highlighted that 1 issue with RCTs is the very selective nature of the patients enrolled - often leading to much better outcomes in trials than we see subsequently in real life - TAVI & SAVR example here
This reduces external validity of the results
Correctly, she highlighted that 1 issue with RCTs is the very selective nature of the patients enrolled - often leading to much better outcomes in trials than we see subsequently in real life - TAVI & SAVR example here
This reduces external validity of the results

#EACTS2021
Other problems highlighted with RCTs were under-representation of women and ethnic minorities - again reducing external validity of results
If data are mostly from Caucasian males in affluent countries...how relevant are the data on a global scale?


Other problems highlighted with RCTs were under-representation of women and ethnic minorities - again reducing external validity of results
If data are mostly from Caucasian males in affluent countries...how relevant are the data on a global scale?



#EACTS2021
Concluded by emphasising that RCTs and observational / real world data should be viewed in combination and as complimentary, not as RCTs are the untouchable gold standard that should never be questioned...
Concluded by emphasising that RCTs and observational / real world data should be viewed in combination and as complimentary, not as RCTs are the untouchable gold standard that should never be questioned...

#EACTS2021
Next talk from Dr Kocher giving an Austrian single-centre experience of the Inspiris Resilia valve
Next talk from Dr Kocher giving an Austrian single-centre experience of the Inspiris Resilia valve

#EACTS2021
Starts off with an explanation of the valve structure.
Based on the highly successful Perimount valve design, with new features to reduce leaflet calcification & for ring to 'expand' to facilitate future V-in-V TAVI when AVR degenerates

Starts off with an explanation of the valve structure.
Based on the highly successful Perimount valve design, with new features to reduce leaflet calcification & for ring to 'expand' to facilitate future V-in-V TAVI when AVR degenerates


#EACTS2021
This slide is a little over-hyped imho...the valves were explanted after just 8 months...we need a longer timeframe, but I understand the premise - these leaflets are hopefully less prone to calcification
This slide is a little over-hyped imho...the valves were explanted after just 8 months...we need a longer timeframe, but I understand the premise - these leaflets are hopefully less prone to calcification

#EACTS2021
Maybe I'm just spoilt by excellent outcomes where I work, but I was worried by these data
30-day mortality 2.6% in a cohort with mean age just 60, and 94pts are <60yrs old? We didn't have STS scores that I saw, but this seemed really high to me
Is that unfair?
Maybe I'm just spoilt by excellent outcomes where I work, but I was worried by these data
30-day mortality 2.6% in a cohort with mean age just 60, and 94pts are <60yrs old? We didn't have STS scores that I saw, but this seemed really high to me
Is that unfair?

#EACTS2021
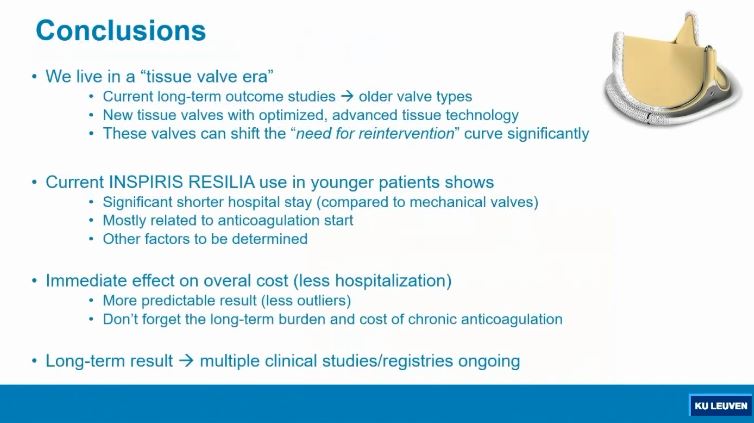
Final talk in this symposium by Professor Bert Meuris from Leuven. Health economic data...hmmm...let's see!
Final talk in this symposium by Professor Bert Meuris from Leuven. Health economic data...hmmm...let's see!

#EACTS2021
Starts by highlighting that implant rates for mechanical valves in ALL age ranges are falling, including the <60s...that was quite striking to see
Starts by highlighting that implant rates for mechanical valves in ALL age ranges are falling, including the <60s...that was quite striking to see

#EACTS2021
However, if you put tissue valves into younger patients, you're going to have problems (well, the patients will...)
However, if you put tissue valves into younger patients, you're going to have problems (well, the patients will...)

#EACTS2021
Again, the data (that Prof Meuris' team conducted) showing significantly less leaflet calcium on the Inspiris compared to Perimount valve after 8 months in an animal model...my thoughts on this later...
Again, the data (that Prof Meuris' team conducted) showing significantly less leaflet calcium on the Inspiris compared to Perimount valve after 8 months in an animal model...my thoughts on this later...

#EACTS2021
Many registries and small studies conducted
The pitch was very much that these valves may be used in patients that would otherwise receive a mechanical valve - mAVR means more bleeding, tAVR means more re-do procedures

Many registries and small studies conducted
The pitch was very much that these valves may be used in patients that would otherwise receive a mechanical valve - mAVR means more bleeding, tAVR means more re-do procedures


#EACTS2021
Retrospective review of patients that had been allocated to mAVR or tAVR with Inspiris - latter group had shorter stays in ICU & overall in hospital


Retrospective review of patients that had been allocated to mAVR or tAVR with Inspiris - latter group had shorter stays in ICU & overall in hospital



#EACTS2021
This slide was...interesting
There was NO mention of the cost of the Inspiris Resilia valve itself and how that compares to a mechanical valve...see end of thread for why that matters...
This slide was...interesting
There was NO mention of the cost of the Inspiris Resilia valve itself and how that compares to a mechanical valve...see end of thread for why that matters...

#EACTS2021
These slides were used to illustrate that anticoagulation comes at a price, soemtimes due to low INR needing admission for correction or bleeding complications causing admission and possibly major harm

These slides were used to illustrate that anticoagulation comes at a price, soemtimes due to low INR needing admission for correction or bleeding complications causing admission and possibly major harm


#EACTS2021
So, my thoughts? Well, this was a cleverly crafted session. The constant theme through the talks was to question the primacy of RCTs & showcase the utility of real world data
Now, as it happens, I *agree* that RCTs have major flaws, especially some done recently...
So, my thoughts? Well, this was a cleverly crafted session. The constant theme through the talks was to question the primacy of RCTs & showcase the utility of real world data
Now, as it happens, I *agree* that RCTs have major flaws, especially some done recently...
#EACTS2021
Cherrypicking patients to maximise likelihood of a significant difference between two arms is not useful, if the outcomes achieved in an RCT - upon which FDA / CE approvals may be based - simply cannot be recreated in our daily practice
Cherrypicking patients to maximise likelihood of a significant difference between two arms is not useful, if the outcomes achieved in an RCT - upon which FDA / CE approvals may be based - simply cannot be recreated in our daily practice
#EACTS2021
However - where I disagreed is what we do about this. The answer is not to embrace retrospective observational studies even more but to improve RCTs! We *have* to demand better of our randomised studies. There's a reason randomised studies are considered best
However - where I disagreed is what we do about this. The answer is not to embrace retrospective observational studies even more but to improve RCTs! We *have* to demand better of our randomised studies. There's a reason randomised studies are considered best
#EACTS2021
Randomisation evenly & randomy distributes all variables - known & unknown - that could influence outcomes
So, must do better to enrol women, to enrol ethnic minorities & to reduce exclusion criteria...of course, *obvious* reasons trial sponsors may not be keen
Randomisation evenly & randomy distributes all variables - known & unknown - that could influence outcomes
So, must do better to enrol women, to enrol ethnic minorities & to reduce exclusion criteria...of course, *obvious* reasons trial sponsors may not be keen
#EACTS2021
In our hospital, we stopped using Inspiris Resilia due to cost. These were valve costs to us:
Mechanical AVR - £1100
Perimount Magna Ease - £1500
Inspiris Resilia - £3000
(Sapien 3 TAVI - £20,500 - just for info)
So, Inspiris was DOUBLE the cost of Perimount
In our hospital, we stopped using Inspiris Resilia due to cost. These were valve costs to us:
Mechanical AVR - £1100
Perimount Magna Ease - £1500
Inspiris Resilia - £3000
(Sapien 3 TAVI - £20,500 - just for info)
So, Inspiris was DOUBLE the cost of Perimount
#EACTS2021
Our surgeons were not very happy. But, on this occasion, I had some sympathy with the managers too. The new valve is DOUBLE the cost of the old valve and there are ZERO data (by definition) *proving* that it lasts longer than the original Perimount Mgane Ease
Our surgeons were not very happy. But, on this occasion, I had some sympathy with the managers too. The new valve is DOUBLE the cost of the old valve and there are ZERO data (by definition) *proving* that it lasts longer than the original Perimount Mgane Ease
#EACTS2021
In theory, the valve should last longer & V-in-V TAVI should have better outcomes-but of course no-one knows for sure, as that hasn't happended yet
So, if you work in a wealthy nation without restrictions, I can understand you may opt to pay more for the new valve
In theory, the valve should last longer & V-in-V TAVI should have better outcomes-but of course no-one knows for sure, as that hasn't happended yet
So, if you work in a wealthy nation without restrictions, I can understand you may opt to pay more for the new valve
#EACTS2021
But, the Perimount Magna Ease is already a very good valve! Most patients get >10 years from it and a decent % get between 13-15 years
Are we saying we think Inspiris Resilia will last significantly longer than that?? I'm not so sure...
But, the Perimount Magna Ease is already a very good valve! Most patients get >10 years from it and a decent % get between 13-15 years
Are we saying we think Inspiris Resilia will last significantly longer than that?? I'm not so sure...
#EACTS2021
I'm sure I'm coming across as too cynical. I don't mean to. I applaud Industry for spending R&D funds on improving bioprostheses & Edwards has been a leader in the field
But, it would be nice to have a well-conduced RCT of Inspiris vs mAVR in 50-60yr olds
End! 😀
I'm sure I'm coming across as too cynical. I don't mean to. I applaud Industry for spending R&D funds on improving bioprostheses & Edwards has been a leader in the field
But, it would be nice to have a well-conduced RCT of Inspiris vs mAVR in 50-60yr olds
End! 😀
• • •
Missing some Tweet in this thread? You can try to
force a refresh