Yesterday the FDA Advisory committee recommended that the 15 million Americans who have had J&J vaccines, more than 2 months out, get a 2nd shot.
There are some significant issues with this that could have been prevented /1
There are some significant issues with this that could have been prevented /1

By May 1, there were over 8 million people 5.5 months out
By June 1, the number rose to nearly 11 million people 4.5 months out
Yet data have consistently been showing attrition of protection vs infections for this vaccine, this week in 620,000 US Veterans /2
By June 1, the number rose to nearly 11 million people 4.5 months out
Yet data have consistently been showing attrition of protection vs infections for this vaccine, this week in 620,000 US Veterans /2

This is the only Covid vaccine that was positioned as "one and done." J&J is the largest healthcare company in the world, yet research to back that up was undone until recently.
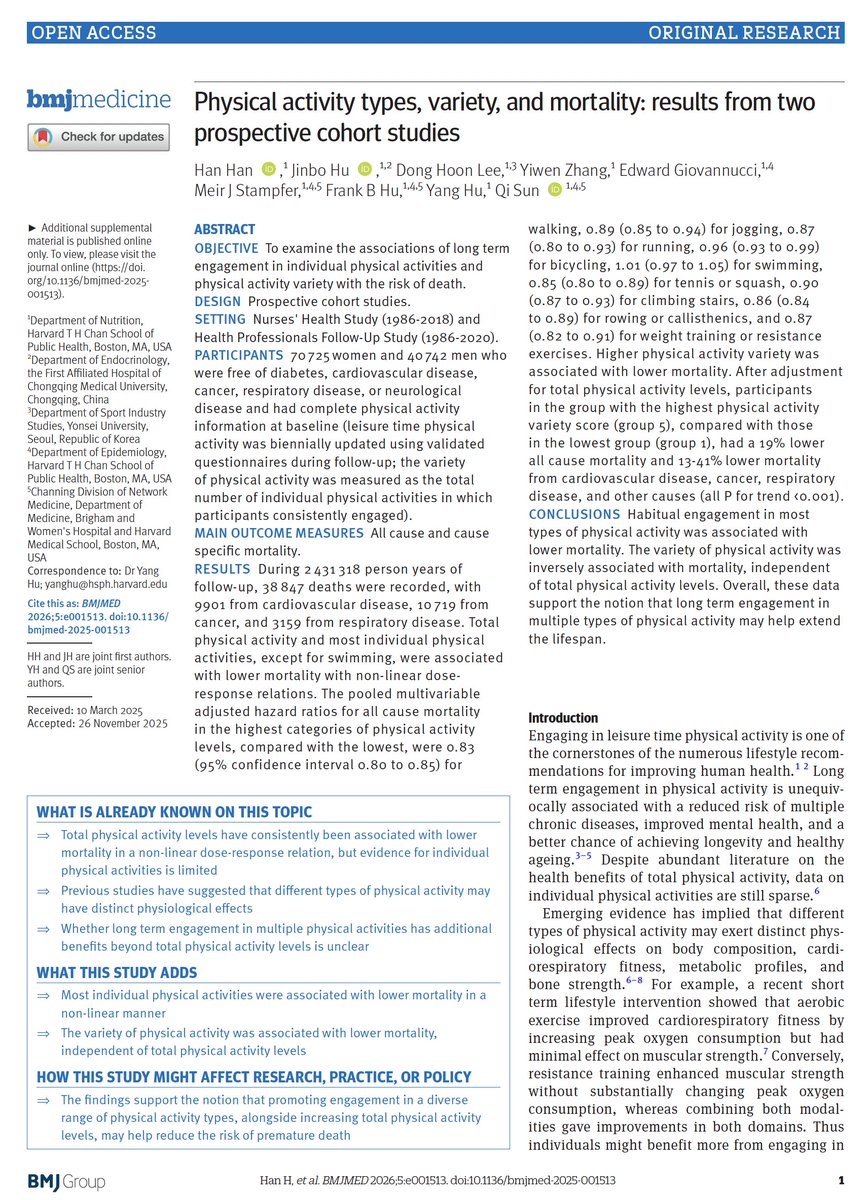
Single dose: 70% protection vs symptomatic infection
2-dose: 94% protection /3
fda.gov/media/153129/d…
Single dose: 70% protection vs symptomatic infection
2-dose: 94% protection /3
fda.gov/media/153129/d…

To start with, the 1-shot 70% efficacy vs. symptomatic infections was considerably lower than the mRNA vaccines (95%), the primary endpoint of all Covid vaccine trials, and a proxy for protection vs hospitalizations and deaths
2-shots brought it to parity in the US at 94% /4
2-shots brought it to parity in the US at 94% /4

A grand total of 17 people were studied for impact on spike protein binding antibody levels (not even neutralization Abs) at 6 months /5 

Parenthetically, the antibody level increase from the 2nd J&J shot at 2 months were small relative to a booster with an mRNA vaccine (50-70 fold, 1 month)/6 



How could this happen? 15 million Americans potentially left vulnerable and still no formal approval for a 2nd shot
1. J&J did insufficient and late in coming research to backup their "one and done" assertion
2. The poor US tracking of data obscured detection of this issue
/7
1. J&J did insufficient and late in coming research to backup their "one and done" assertion
2. The poor US tracking of data obscured detection of this issue
/7
We've known about the lapses in antibody levels and reduced protection vs hospitalization for some time, but left these people (who typically had no choice and were told all vaccines were equivalent) susceptible over a prolonged period 



• • •
Missing some Tweet in this thread? You can try to
force a refresh