
Time for Fix The Vent! #CHEST2021
A: Peak pressure alarm is limiting volume delivery.
They changed the alarm, it's delivering the volume and sat comes up.
They changed the alarm, it's delivering the volume and sat comes up.
Now your screen looks like this.
Your plat is high! It's 35! We like it to be below 30.
To help this, you could decrease the tidal volume (can increase the rate to preserve MV).
Your plat is high! It's 35! We like it to be below 30.
To help this, you could decrease the tidal volume (can increase the rate to preserve MV).

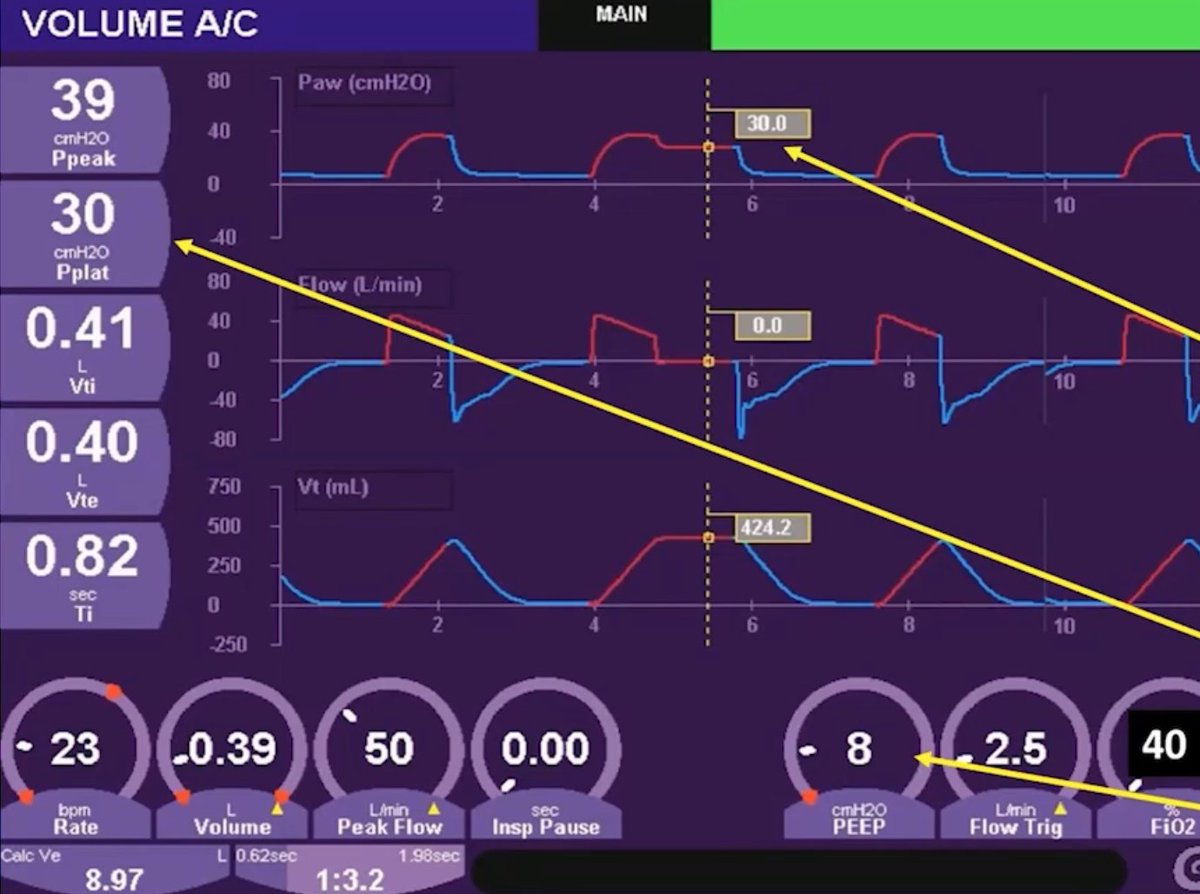
Here's your screen after changing your tidal volume to be closer to 6cc/kg. Things look better, plat is down to 30.
Of note, driving pressure here is 22 (plat 30 - PEEP 8). We like to shoot for 15 or less.
Of note, driving pressure here is 22 (plat 30 - PEEP 8). We like to shoot for 15 or less.
This is a mucus plug!
Two main problems to consider when you get a high pressure alarm
- airway obstruction OR
- resp system stiffening
Look at
- peak/plateau relationship (peak alone = obstruction)
- Exp flow (slow, prolonged = obstruction)
Two main problems to consider when you get a high pressure alarm
- airway obstruction OR
- resp system stiffening
Look at
- peak/plateau relationship (peak alone = obstruction)
- Exp flow (slow, prolonged = obstruction)
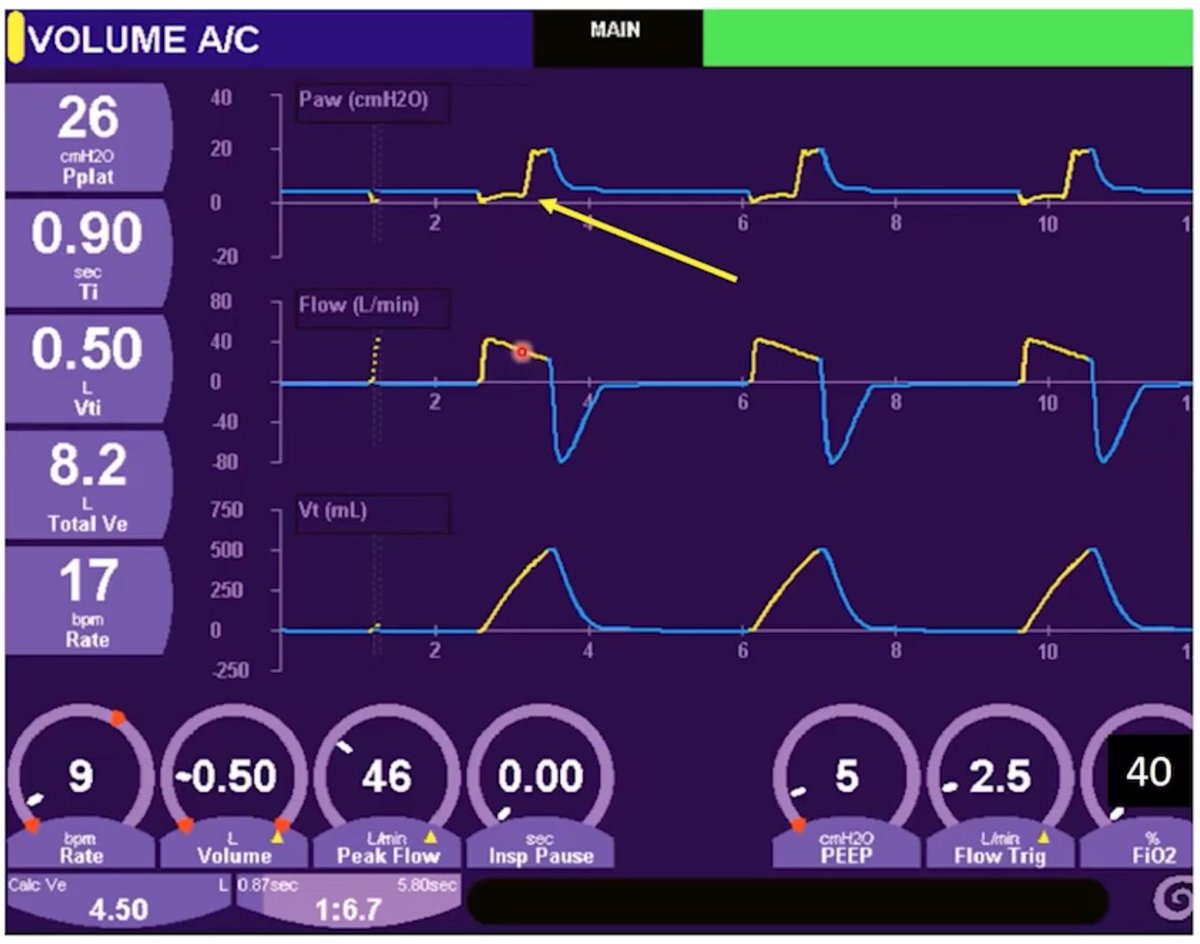
This is AutoPEEP, which is common in patients with airway obstruction.
You see slow expiratory flow here, and it doesn't come back to zero prior to the next breath.
You see slow expiratory flow here, and it doesn't come back to zero prior to the next breath.

You measure AutoPEEP with an expiratory hold maneuver. Measured total PEEP here is 12, when we've set it at 5! 

How can you fix this?
You can
- decrease the rate
- or increase the flow rate
Both allow for a longer expiratory time to get that air out.
You can
- decrease the rate
- or increase the flow rate
Both allow for a longer expiratory time to get that air out.
Even though you reduce the MV, your CO2 may still improve!
Less autopEEP reduces intrathoracic pressure and improves pulmonary blood flow.
Less autopEEP reduces intrathoracic pressure and improves pulmonary blood flow.

This is flow asynchrony. It was set, but now your unparalyzed patient is waking up and trying to take breaths. Patient wants more flow, vent doesn't give it, and patient pulls down the flow tracing. 
How do we fix it?
The flow was increased (in my Maquet vents, this isn't an option--must change I:E instead and come at it indirectly)
What's the consequence of increasing flow?
Your I time decreases.
Is that a problem? Can be...
The flow was increased (in my Maquet vents, this isn't an option--must change I:E instead and come at it indirectly)
What's the consequence of increasing flow?
Your I time decreases.
Is that a problem? Can be...
They could start double triggering--one effort causes two breaths. Vent can't recognize that the patient's long breath is only one breath, so it gives two. 

You could also try switching to pressure control.
What's your unintended consequence here?
Increased volumes. Your patient wants to breathe more than what you're giving them, and they're going to try do it in either mode, just in different ways.
What's your unintended consequence here?
Increased volumes. Your patient wants to breathe more than what you're giving them, and they're going to try do it in either mode, just in different ways.

This is a circuit leak.
All of our volume is not coming back to the vent.
Can happen due to:
- Sensitive flow trigger
- Large air leak
Both can cause auto-triggering.
All of our volume is not coming back to the vent.
Can happen due to:
- Sensitive flow trigger
- Large air leak
Both can cause auto-triggering.

This is what it looks like when an in line neb is hooked up. You're getting way more volume back than what you put in. 

Your plat has increased with your peak, so it's a compliance issue.
Options:
- ptx
- flash edema
- R mainstem intubation
Also note expiratory flow has become much faster.
Options:
- ptx
- flash edema
- R mainstem intubation
Also note expiratory flow has become much faster.
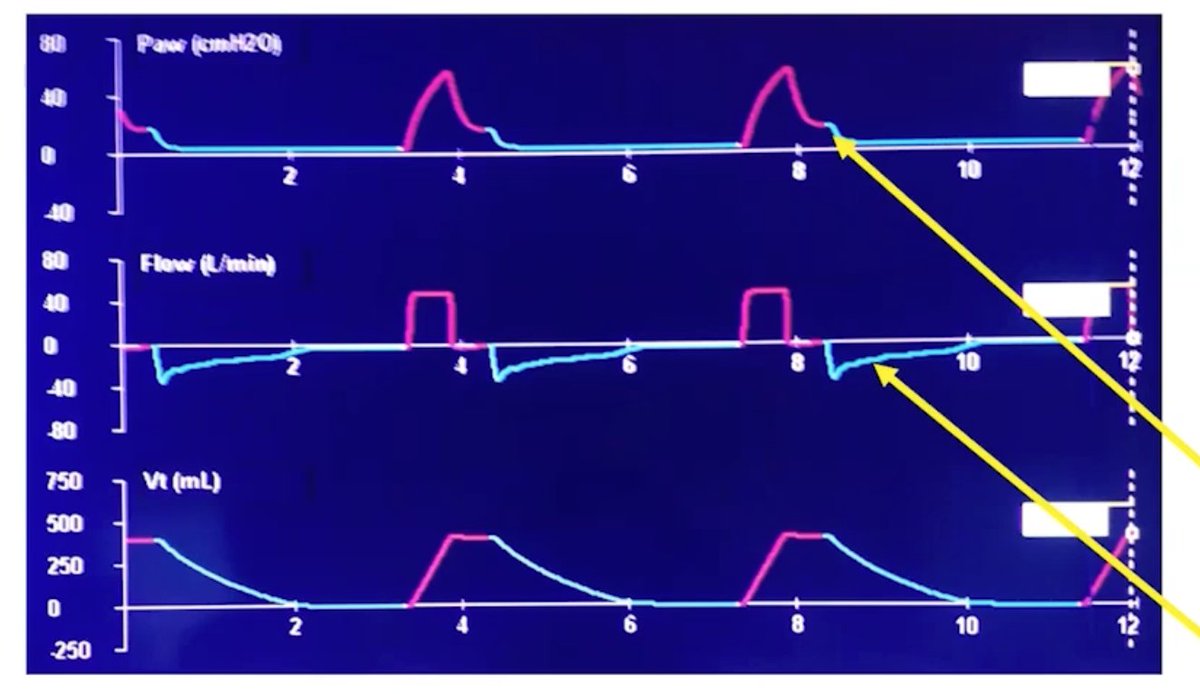
Opposite scenario--peak up, but not plateau. This is a resistance problem. You will also see slow expiratory flow.
- mucus plug
- bronchospasm
- kinked ET tube
- mucus plug
- bronchospasm
- kinked ET tube
In pressure control, VOLUME will change with changes in compliance or resistance.
Look at your expiratory flow to help sort out which pathway is the problem.
Look at your expiratory flow to help sort out which pathway is the problem.

Shew! That required some rapid fire tweeting to keep up but it was SUCH a great overview!
Time for Q&A now.
Time for Q&A now.
Adding PEEP to address intrinsic PEEP--idea is that you can maybe splint the airways open a bit. This may happen in a minority, but is not recommended routinely apparently.
The other use of PEEP here is to help with the triggering process.
The other use of PEEP here is to help with the triggering process.
Adding a little PEEP when a patient is autoPEEPing can keep the patient from having to pull soooo far down to get the breath to trigger. Less delay between patient effort and ventilator response.
Reverse triggering--it does exist.
Double triggering, but patient is deeply sedated so pretty clear they're not double triggering because they want more/faster/bigger breath.
Double triggering, but patient is deeply sedated so pretty clear they're not double triggering because they want more/faster/bigger breath.
With mucus plugging, you can also see what looks like a compliance change because if you've totally obstructed a segment or a whole lung, you're sending the same amount of volume into less lung.
Are air trapping and autoPEEP the same thing?
Yes.
Also, you *can* have air trapping where the flow does reach 0--suspect the small airways totally collapse resulting in no flow.
Yes.
Also, you *can* have air trapping where the flow does reach 0--suspect the small airways totally collapse resulting in no flow.
No clear answer for patients pulling large volumes. We know it's not good, we also know that heavy sedation and NMB can also lead to badness.
If your volumes are reasonable (8-10ml/kg or 12?) maybe let them be as long as compliance/plateaus ok?
If your volumes are reasonable (8-10ml/kg or 12?) maybe let them be as long as compliance/plateaus ok?
Trying to balance two bad things. The sicker the patient, the more likely you may be to quiet things down with sedation/NMB.
No magical mode, unfortunately.
No magical mode, unfortunately.
Balancing driving pressure and plateaus?
Plat >30 in multiple studies adjusted for chest wall --> clearly harmful.
Driving pressure < 15? Growing evidence says probably, but not as strong as evidence re: plateaus.
Plat >30 in multiple studies adjusted for chest wall --> clearly harmful.
Driving pressure < 15? Growing evidence says probably, but not as strong as evidence re: plateaus.
Synchrony issues: look at the vent, look at the patient.
Makes me think of our local vent whisperer, @mossy_rolling.
Makes me think of our local vent whisperer, @mossy_rolling.
@mossy_rolling Explaining driving pressure: plateau - PEEP
The amount of pressure required to drive a given pressure into the lungs.
Depends on compliance.
As does the stress index--another way to look at mechanical changes during breath delivery.
The amount of pressure required to drive a given pressure into the lungs.
Depends on compliance.
As does the stress index--another way to look at mechanical changes during breath delivery.
@mossy_rolling High 6.9 range for permissive hypercapnia as long as hemodynamically stable?! 😱
@mossy_rolling Super inverse ratio ventilation.
Idea is better recruitment during tidal breath, short deflation prevents derecruitment (it also causes air trapping).
It also allows spontaneous breaths.
Hidden untoward consequences. Clinical trials have been disappointing.
Idea is better recruitment during tidal breath, short deflation prevents derecruitment (it also causes air trapping).
It also allows spontaneous breaths.
Hidden untoward consequences. Clinical trials have been disappointing.
@mossy_rolling Little agreement even among experts on how to use it, no evidence of benefit. Argues that APRV should only be studied in clinical trials, not used routinely.
@mossy_rolling SIMV 👻
Imagine if you were doing bicep curls with your eyes closed, and you didn't know if you were going to have a 5lb weight or a 20lb weight.
That's SIMV (and it sounds very uncomfortable).
Imagine if you were doing bicep curls with your eyes closed, and you didn't know if you were going to have a 5lb weight or a 20lb weight.
That's SIMV (and it sounds very uncomfortable).
@mossy_rolling It came to be because assist mechanisms used to not be a thing, and it was the only way to allow any kind of patient activity (I didn't not know this!).
@mossy_rolling PS wean? May prolong time on the vent. Just use a comfortable mode when on the vent, then daily assess for readiness to extubate/go to TC.
@mossy_rolling "We need to be weaned from weaning."
@mossy_rolling Utility of mean airway pressure for vent titration?
Generally correlates with better oxygenation in most cases, but goes with everything else we're already doing/watching. Keep an eye on it.
Impacts hemodynamics. May be useful to assess in that regard.
Generally correlates with better oxygenation in most cases, but goes with everything else we're already doing/watching. Keep an eye on it.
Impacts hemodynamics. May be useful to assess in that regard.
@mossy_rolling What about smaller ICUs?
E-ICU/e-consults can help. Important in the age of COVID where transfers are often limited.
E-ICU/e-consults can help. Important in the age of COVID where transfers are often limited.
@mossy_rolling Awesome, awesome talk from
Neil MacIntyre
John Davies
Natalie Yip
Craig Rackley
and Amanda Dexter
Thank you all for this session...so practical and helpful!!
Neil MacIntyre
John Davies
Natalie Yip
Craig Rackley
and Amanda Dexter
Thank you all for this session...so practical and helpful!!
• • •
Missing some Tweet in this thread? You can try to
force a refresh





















