** Bubbles of Truth **
We can gain a tremendous amount of clinical information by observing the flow of bubbles within our vascular system.
Here are a few illustrative examples!
We can gain a tremendous amount of clinical information by observing the flow of bubbles within our vascular system.
Here are a few illustrative examples!
Exhibit A:
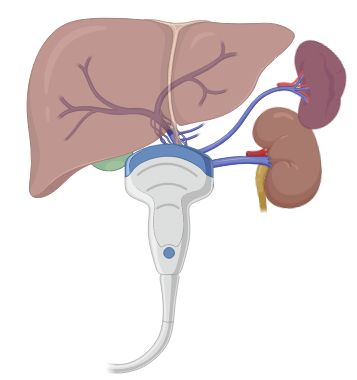
Below is a subxiphoid view highlighting markedly distended hepatic veins and IVC. Note the reflux of bubbles into the HV/IVC consistent with high right sided filling pressures.
Below is a subxiphoid view highlighting markedly distended hepatic veins and IVC. Note the reflux of bubbles into the HV/IVC consistent with high right sided filling pressures.
The bubbles in the above case are arising from rapidly infusing IV fluids through an upper extremity central venous catheter. 

Why the reflux, you say?
Marked dilation of RA/RV with a hyperdynamic LV consistent with RV failure!
Marked dilation of RA/RV with a hyperdynamic LV consistent with RV failure!
Exhibit B:
Utilize your bubbles to help localize (a) venous structures and (b) central catheter tip location.
Utilize your bubbles to help localize (a) venous structures and (b) central catheter tip location.
How? Agitated bubbles can be injected via upper extremity CVCs to localize the catheter tip and observing for chamber quantification! 

*Tip*
When attempting subclavian/axillary vein cannulations use a preexisting ipsilateral peripheral IV to inject agitated saline and localize bubbles within the subclavian vein to make double sure you aren't targeting the artery.
When attempting subclavian/axillary vein cannulations use a preexisting ipsilateral peripheral IV to inject agitated saline and localize bubbles within the subclavian vein to make double sure you aren't targeting the artery.
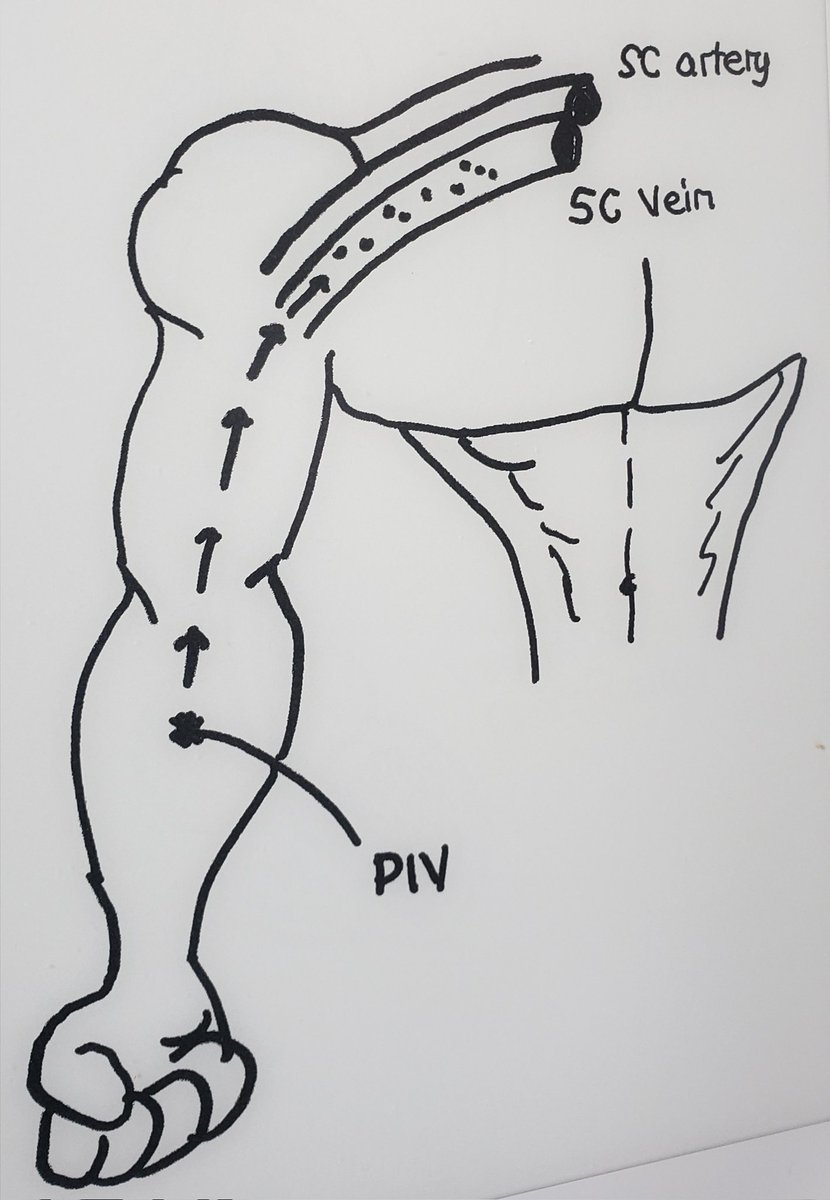
Voila! Longitudinal view of axillary/subclavian vein whilst flushing an ipsilateral peripheral IV. Proceed to cannulate with confidence.
Exhibit C:
Be wary of the patient with shock/resp failure and an abundance of bubbles opacifying the right heart.
Air embolism should be a careful consideration. Although it usually occurs upon removal of the catheter with rapid decompensation..I've seen cases while in situ!
Be wary of the patient with shock/resp failure and an abundance of bubbles opacifying the right heart.
Air embolism should be a careful consideration. Although it usually occurs upon removal of the catheter with rapid decompensation..I've seen cases while in situ!
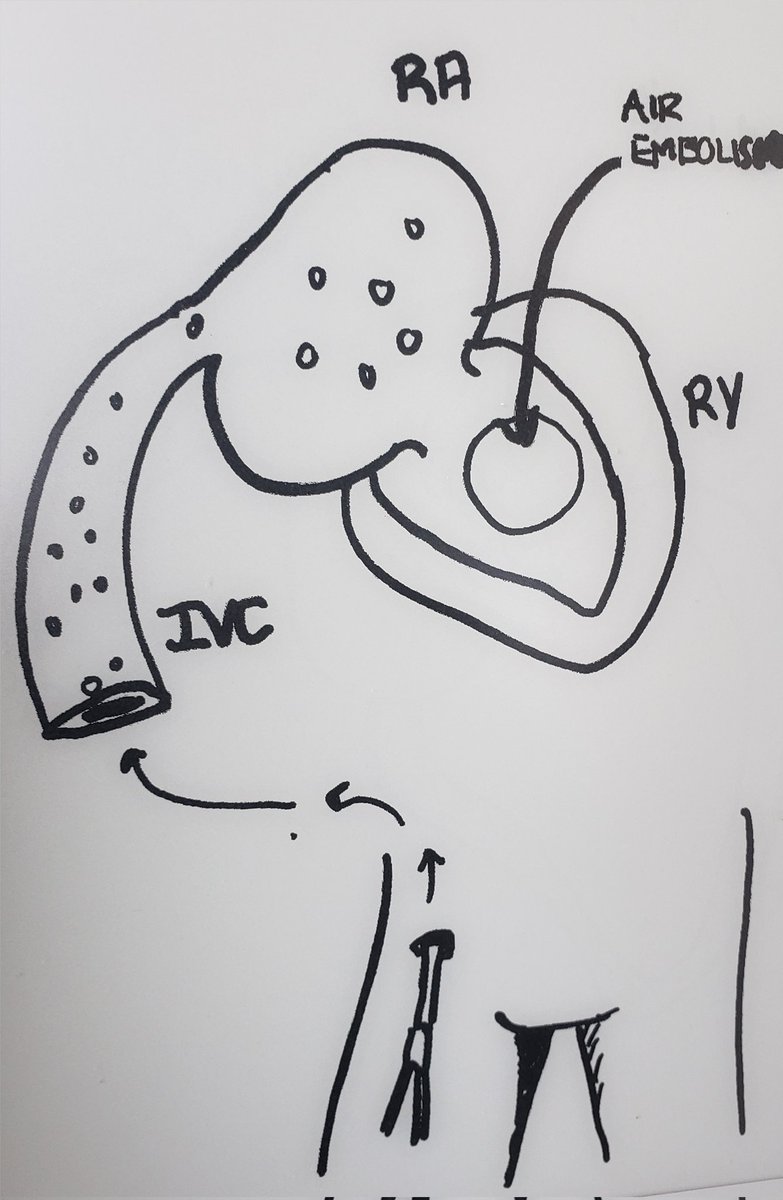
Exhibit D:
Agitated saline for intra and extra cardiac shunting with provocative maneuvers and/or preexisting pulmonary hypertension
1. Atrial septal defects
2. Ventricular septal defects
3. Intrapulmonary shunting
4. Patent ductus arteriosus
5. Persistent L SVC
Agitated saline for intra and extra cardiac shunting with provocative maneuvers and/or preexisting pulmonary hypertension
1. Atrial septal defects
2. Ventricular septal defects
3. Intrapulmonary shunting
4. Patent ductus arteriosus
5. Persistent L SVC
For an amazing in depth review
Check out the review article by Bernard et al "Agitated Saline Contrast Echocardiography in the Identification of Intra and Extracardiac Shunts: Connecting the Dots." JASE 2020
Check out the review article by Bernard et al "Agitated Saline Contrast Echocardiography in the Identification of Intra and Extracardiac Shunts: Connecting the Dots." JASE 2020

Exhibit E:
Bubbles in the portal vein can be an ominous sign indicative of GI tract infection/inflammation.
Bubbles in the portal vein can be an ominous sign indicative of GI tract infection/inflammation.

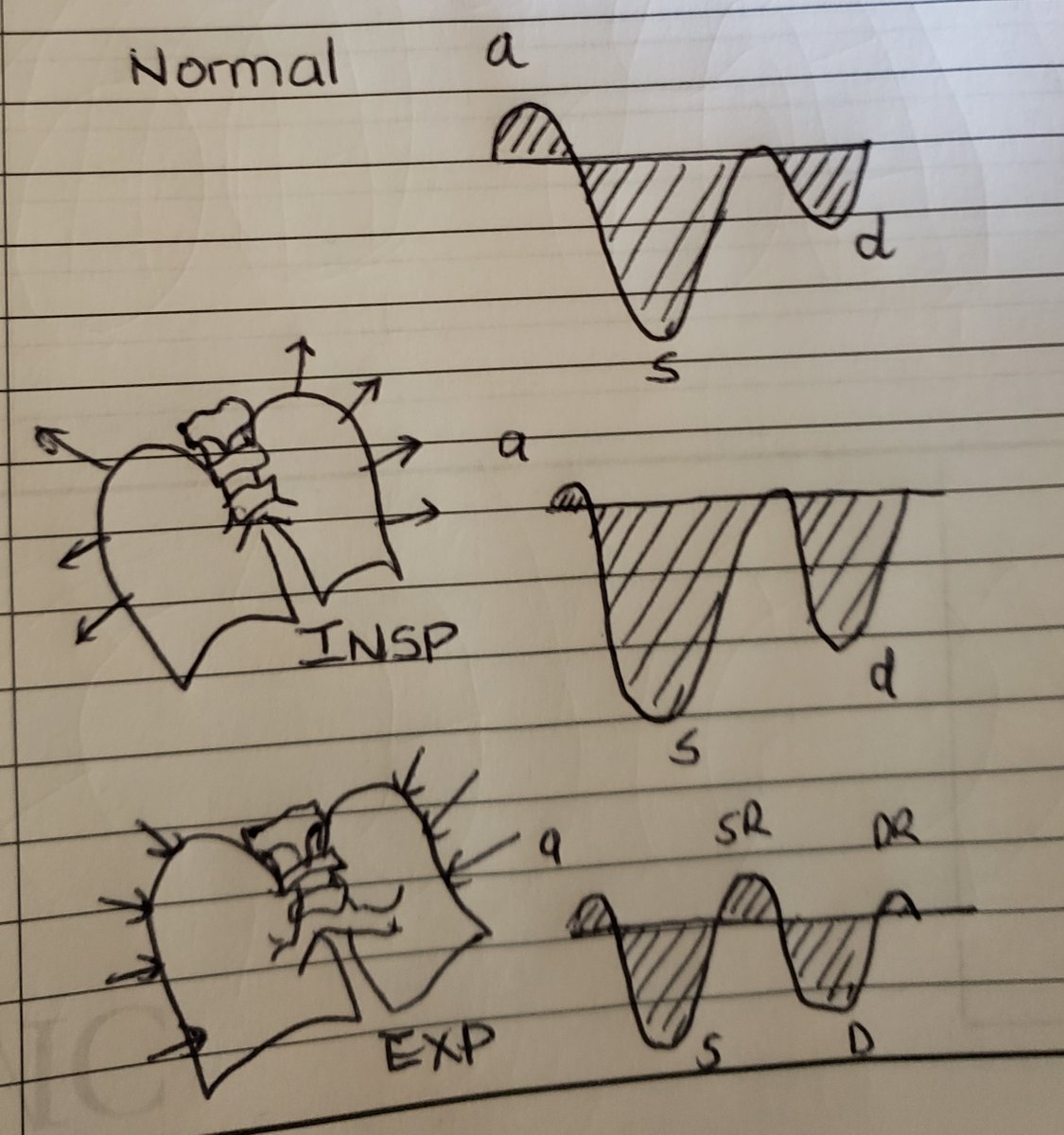
In this example, the patient has the double whammy. Portal vein bubbles and systolic flow reversal in hepatic veins due to right sided heart failure!
In conclusion, Be one with the bubble and follow the bubble for it reveals much about flow in our vascular system.
Uses
1. Assess congestion
2. Intra and Extra cardiac shunting
3. Line placement
4. Gas forming organism /GI tract woes
Any other uses..Oh, Twitterverse?
Uses
1. Assess congestion
2. Intra and Extra cardiac shunting
3. Line placement
4. Gas forming organism /GI tract woes
Any other uses..Oh, Twitterverse?
• • •
Missing some Tweet in this thread? You can try to
force a refresh