1/11
Time for a #tweetorial on one of my favorite topics: Wrist Drop. @AANMember @NMatch2022 #neurology #futureneurologist #neurotwitter #neurotwitternetwork @AANEMorg #meded @KoriPoRodri
The first thing you should think of when you see a patient with weak wrist extension is…
Time for a #tweetorial on one of my favorite topics: Wrist Drop. @AANMember @NMatch2022 #neurology #futureneurologist #neurotwitter #neurotwitternetwork @AANEMorg #meded @KoriPoRodri
The first thing you should think of when you see a patient with weak wrist extension is…
2/11
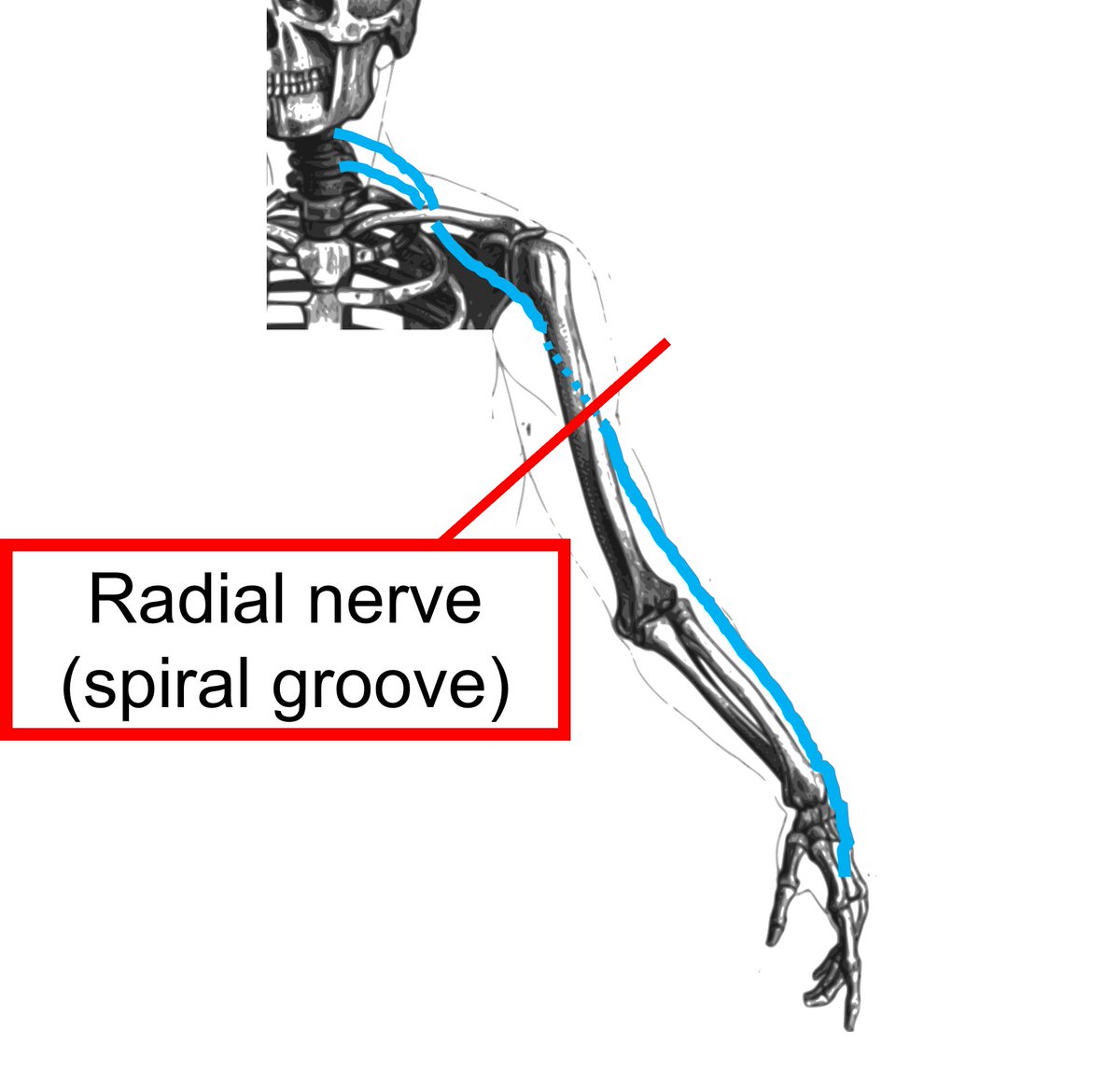
This. Compression of the radial nerve at spiral groove. And usually, we think of it as being caused by...
This. Compression of the radial nerve at spiral groove. And usually, we think of it as being caused by...
3/11
This. And by the way, if you’re ever curious about the surprising origins of the term “Saturday Night Palsy,” read this article. pubmed.ncbi.nlm.nih.gov/12188953/
But I digress. The spiral groove (aka radial groove) is not the only peripheral localization for wrist drop.
This. And by the way, if you’re ever curious about the surprising origins of the term “Saturday Night Palsy,” read this article. pubmed.ncbi.nlm.nih.gov/12188953/
But I digress. The spiral groove (aka radial groove) is not the only peripheral localization for wrist drop.

4/11
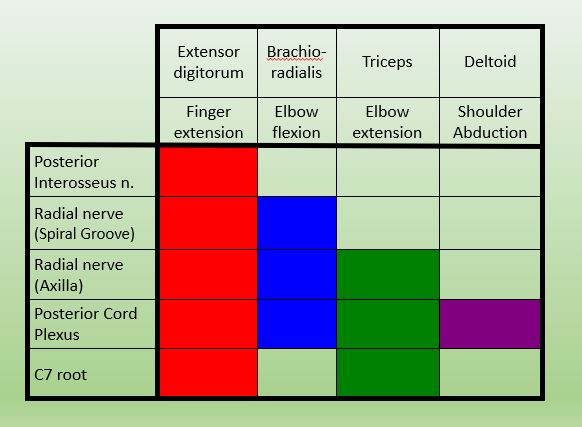
This chart shows you who you can distinguish five peripheral localizations by only testing four other muscles. (How is that even mathematically possible?)
This chart shows you who you can distinguish five peripheral localizations by only testing four other muscles. (How is that even mathematically possible?)
5/11
But when a patient shows up in the ED with a wrist drop that wasn’t there the night before, you are really thinking of the 2 most likely things:
1. Radial mononeuropathy at the spiral groove
2. Stroke. (In the infamous hand knob!)
How do you tell them apart without imaging?
But when a patient shows up in the ED with a wrist drop that wasn’t there the night before, you are really thinking of the 2 most likely things:
1. Radial mononeuropathy at the spiral groove
2. Stroke. (In the infamous hand knob!)
How do you tell them apart without imaging?

6/11
The brachioradialis may be particularly helpful. It is supplied by the radial nerve, but it is a FLEXOR. It flexes the elbow with the thumb pointing up. CNS lesions often affect extensors more, so the brachioradialis (both the muscle and reflex) may be spared in stroke.
The brachioradialis may be particularly helpful. It is supplied by the radial nerve, but it is a FLEXOR. It flexes the elbow with the thumb pointing up. CNS lesions often affect extensors more, so the brachioradialis (both the muscle and reflex) may be spared in stroke.
7/11
And patients with radial neuropathy can’t extend the wrist at all. Patients with a stroke may have trouble extending it volitionally, but (and I just learned this!) they may be able to extend it when they try to make a fist, because of synkinetic activation of the extensors.
And patients with radial neuropathy can’t extend the wrist at all. Patients with a stroke may have trouble extending it volitionally, but (and I just learned this!) they may be able to extend it when they try to make a fist, because of synkinetic activation of the extensors.
8/11
So a patient with a radial mononeuropathy trying to make a fist would look like this.
So a patient with a radial mononeuropathy trying to make a fist would look like this.
9/11
While a patient with a cortical wrist drop trying to make a fist might be able to do this.
While a patient with a cortical wrist drop trying to make a fist might be able to do this.
10/11
Localization take homes:
1. Check the brachioradialis and compare sides. If weak, you may not need imaging.
2. Have the patient make a fist. If they extend, it's probably a brain problem.
3. Still not sure? Go look at that chart to figure out all the less common things!
Localization take homes:
1. Check the brachioradialis and compare sides. If weak, you may not need imaging.
2. Have the patient make a fist. If they extend, it's probably a brain problem.
3. Still not sure? Go look at that chart to figure out all the less common things!
11/11
The last point I wanted to make is what to do if you think it's a radial neuropathy.
1. Order OT and get them a cock up wrist splint.
2. Refer for an EMG in 3-4 weeks and tell them to cancel the appt if they are better. And guess what... they almost always are by then!
The last point I wanted to make is what to do if you think it's a radial neuropathy.
1. Order OT and get them a cock up wrist splint.
2. Refer for an EMG in 3-4 weeks and tell them to cancel the appt if they are better. And guess what... they almost always are by then!
• • •
Missing some Tweet in this thread? You can try to
force a refresh