This headline is inappropriately alarmist given the content of the paper.
It will obviously be misused by anti vaxxers.
I thought it worth a short thread to highlight what it means.
TL;DR nothing in this paper undermine trust in data on BioNtech / Pfizer trials.
/1
It will obviously be misused by anti vaxxers.
I thought it worth a short thread to highlight what it means.
TL;DR nothing in this paper undermine trust in data on BioNtech / Pfizer trials.
/1
https://twitter.com/bmj_latest/status/1455531359536128014
A whistle blower reports poor compliance with Good Clinical Practice at a CRO managing 3 US sites in the Pfizer study.
There is no evidence that these errors would have undermined the scientific integrity of the trial results.
Example 1: needle disposal
/2
There is no evidence that these errors would have undermined the scientific integrity of the trial results.
Example 1: needle disposal
/2

The Texas CRO being criticised was managed by large global CRO icon. The article tells us icon raised concerns about turn around time. This is the system working.
In any large clinical trial there are numerous little arrow made at sites. This trial was done at huge speed.
/3
In any large clinical trial there are numerous little arrow made at sites. This trial was done at huge speed.
/3

And the paper spends a lot of time discussing FDA inspections.
What do we learn? The CRO was clearly aware there were GCP issues that an FDA inspection would find.
And we are told "corrective action" was undertaken.
Also a good sign that management was aware and acting.
/4

What do we learn? The CRO was clearly aware there were GCP issues that an FDA inspection would find.
And we are told "corrective action" was undertaken.
Also a good sign that management was aware and acting.
/4


Anyone who has ever been involved in a large complex clinical trial knows errors are made. The regulations are all about putting in place systems and documentation to help reduce the errors, spot them, and correct them when they happen.
Going fast stresses the system.
/6
Going fast stresses the system.
/6
The covid vaccines were developed at speed in a pandemic. That inevitably put everyone and everything under pressure.
It is no surprise that speed resulted in some compliance issues and that staff were working outside of their comfort zone.
/7
It is no surprise that speed resulted in some compliance issues and that staff were working outside of their comfort zone.
/7

The key question is : were any of these issues serious enough to undermine the scientic integrity of the trial results?
The paper does not all claim that they did.
How does the paper end?
/8

The paper does not all claim that they did.
How does the paper end?
/8

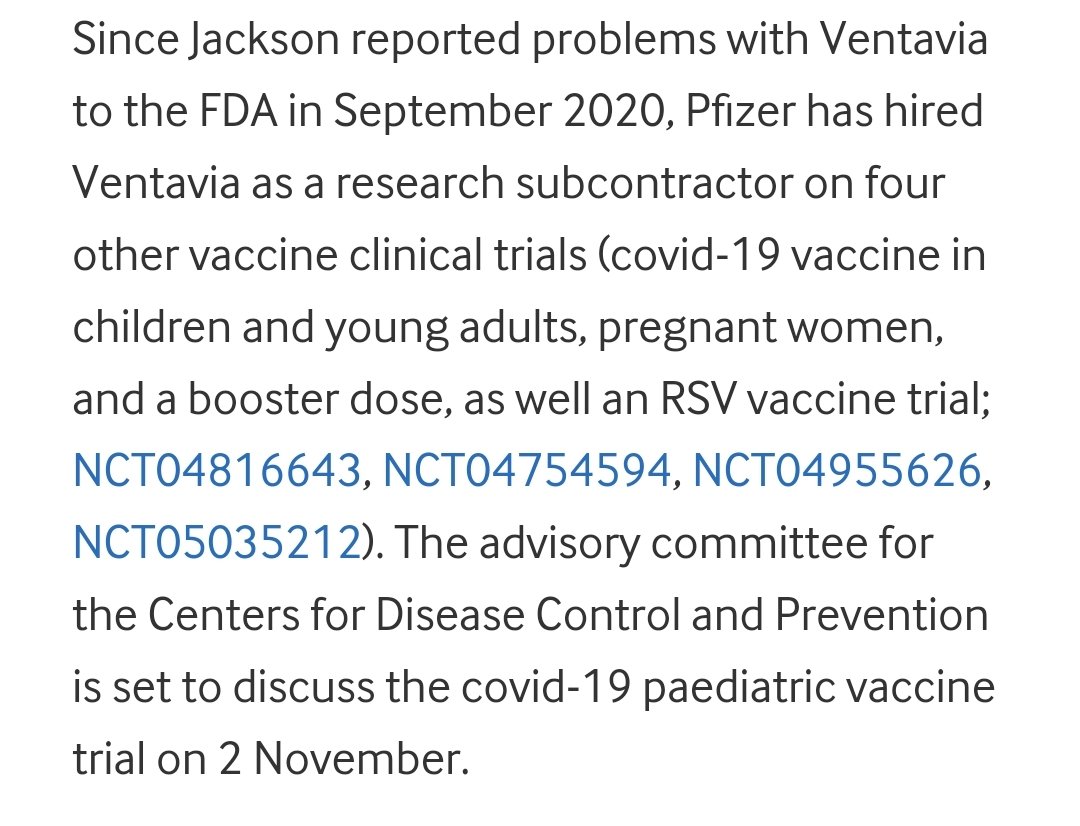
Well we learn at the end of the paper that the study Sponsor (Pfizer) conducted an audit and clearly was sufficiently happy with the data quality and CRO performance that used the company again.
This is a non story.
But it will be abused by anti-vaxxers.
/9
This is a non story.
But it will be abused by anti-vaxxers.
/9
This is a story of a CRO operating under pressure, with mistakes made, and some poor people management.
But nothing here justifies the sort of anti-vaxx comments the BMJ tweet has generated.
@bmj_latest should surely know better.
But nothing here justifies the sort of anti-vaxx comments the BMJ tweet has generated.
@bmj_latest should surely know better.
I have recently seen this article that makes the same point as this thread.

https://twitter.com/skepticalraptor/status/1457449071443054596?s=20

• • •
Missing some Tweet in this thread? You can try to
force a refresh