
I feel like it's “time” for a shoddily-organized scratching-the-surface #neuropsychtwitter #tweetorial on clock drawing in dementia. 1/x 
I will focus on the most common (or arguably best) version of the clock drawing test (CDT): command (free) drawing of a “10 after 11” clock followed by copy of a clock stimulus. 2/x 

The first documented use of CDT was by Sir Henry Head. Per Hazan et al. 2017: “Head's reasoning behind using the clock tests was that they required the execution of meaningful speech, an almost impossible task for people with aphasia.” 3/x bit.ly/3mJDVrb
Instructions per Hazan (above), which is more or less what I use too, are: “Draw the face of the clock. Put in the numbers and set the time to 10 after 11.” I argue that it is important not to say “hands”—part of the test is knowing the mechanism for showing the time. 4/x
CDT is used for all sorts of purposes, presumably bc it recruits so many disparate skills that it can also be said to evaluate all of those skills. Constructional praxis, semantic retrieval, memory, cognitive flexibility, attention, & graphomotor skills are all involved. 5/x
A table in the Grande et al. (2013) CDT chapter unfortunately got screwed up in the publication process, but this is the correct original properly-formatted version that summarizes some most likely errors associated with various lesion locations. 6/x 

Most studies have introduced, or reused, various scoring approaches to differentiate “dementia” or Alzheimer’s disease from healthy controls or an MCI group. See this paper using machine learning to do this using a digital version of the CDT. 7/x bit.ly/3GTE7Mn
This study found a set of 6 specific errors that were nearly pathognomonic for dementia presence and created an algorithm based on those errors. 8/x bit.ly/3GTohBk
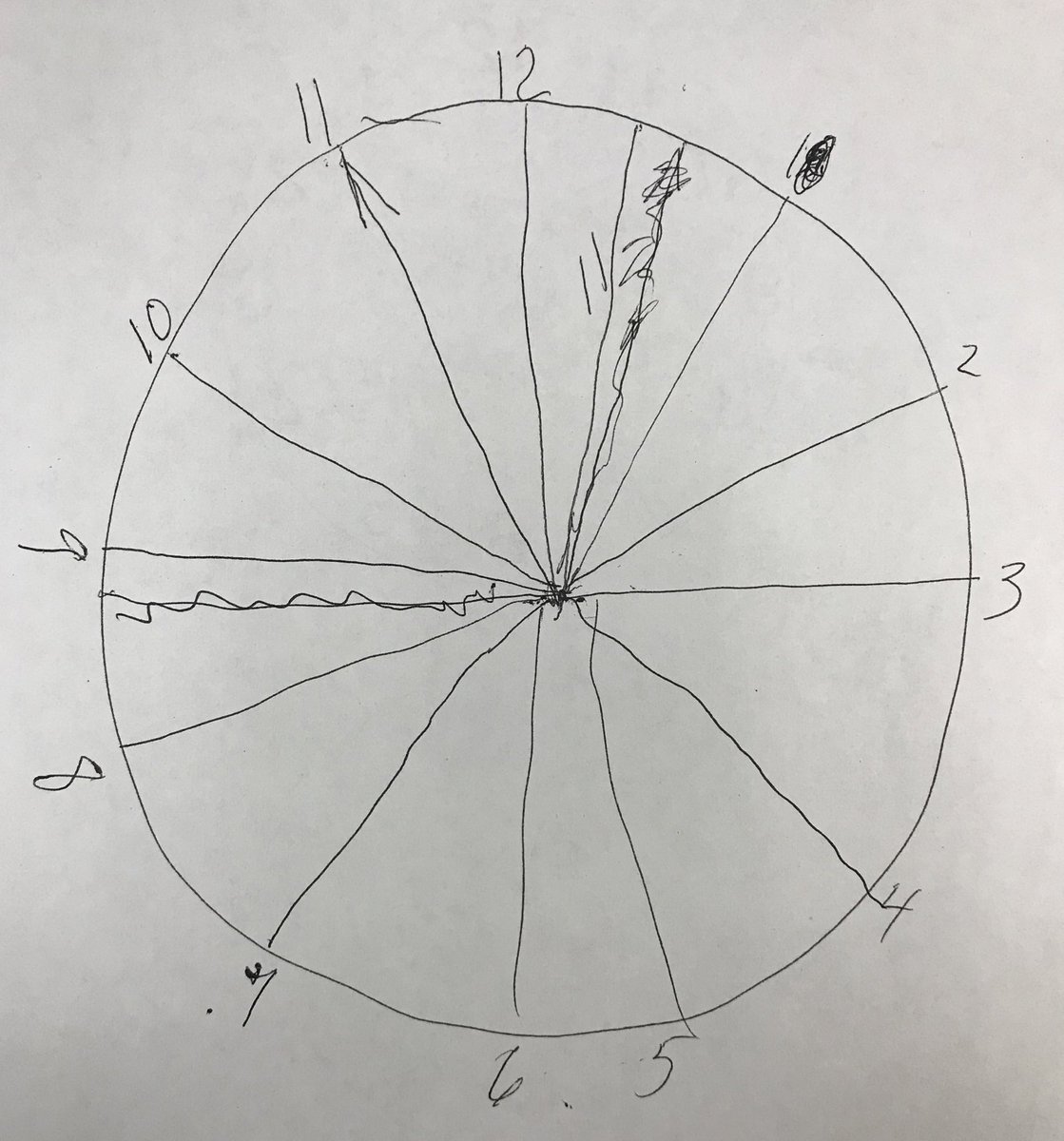
Error-based (“qualitative”) scoring systems tend to outperform the so-called “quantitative” systems (is there a contour, are there numbers, etc.). (Here is a clock from someone who was impaired enough to probably not require a clock) 9/x 

What do I use clinically? I don’t use any, but I expect that data will soon even more strongly support the clinical use of such error-based methods like the one by @cosentinolab 10/x bit.ly/3BPQEg1
Moving from assessment of impaired/intact to differential diagnosis, a “classic” dichotomized error analysis says that conceptual errors are more typical of “cortical” dementias (think AD), while dysexecutive errors are more typical of “subcortical” dementias (think VascD). 11/x
Also note that the copy drawing is very important! Even if command is intact, it is critical to also administer the copy condition. Libon et al. (1996) had shown that people with AD improve from command to copy whereas people with VascD do not. 12/x bit.ly/2ZLOgK5
Also see, for example, this work on the MoCA clock item by @Cep23Katie @cosentinolab @dawnbowersphd: differences between diagnostic groups were not detected by the standard command condition and only appeared when comparing command and copy drawings. 13/x bit.ly/2Yh2vWR
Kaplan & colleagues met for years to develop the FHS scoring system—that’s actually where she was when I met her--but FHS has switched to a digital CDT so I’m not sure this particular system will be investigated much more beyond this normative paper. 14/x bit.ly/3EJSkJZ
There’s a rumor that people aren’t learning analog clocks & the test will be phased out eventually. Maybe. My kids learned in school to read analog, we have one on our wall, but in households that don’t, this seems like a possibility. 15/x bit.ly/2ZNL7JM
Despite zillions of papers examining group classification in AD, PD, etc., there’s not much looking at actual association between CDT and neuropsychological performance, or at least not in any way that would facilitate the application of the findings. More work to be done! 16/x
Finally, an obscene number of articles and chapters on CDT include a clock-related pun in their titles. I love a good joke as much as anyone else, but there's enough out there now, and it’s about damn “time” for y’all to stop that. 17/17 fin
Shout out to myself, for making like 5 attempts to tweet this out over the course of today. Hopefully Twitter didn’t lie and this last attempt is the only one that actually worked. Sorry if there are 4 other instances of the same tweetorial in your feed. Don’t blame me.
• • •
Missing some Tweet in this thread? You can try to
force a refresh



