💊Exciting news today about another oral therapy for early COVID: reduced hospitalization & mortality.
Here’s a Deep dive 🧵 on the new PF-07321332 protease inhibitor (“Paxlovid”) & the very impressive results announced from the EPIC-HR trial.
TL/DR: this is a big deal.
1/


Here’s a Deep dive 🧵 on the new PF-07321332 protease inhibitor (“Paxlovid”) & the very impressive results announced from the EPIC-HR trial.
TL/DR: this is a big deal.
1/



What the heck is PF-07321332?
All coronaviruses produce a polypeptide that must be cleaved by a protease into 11 proteins. Without this protease the virus can’t co-opt cellar machinery & reproduce.
PF-07321332 Inhibits the viral main protease (Mpro).
2/
pdb101.rcsb.org/motm/242

All coronaviruses produce a polypeptide that must be cleaved by a protease into 11 proteins. Without this protease the virus can’t co-opt cellar machinery & reproduce.
PF-07321332 Inhibits the viral main protease (Mpro).
2/
pdb101.rcsb.org/motm/242

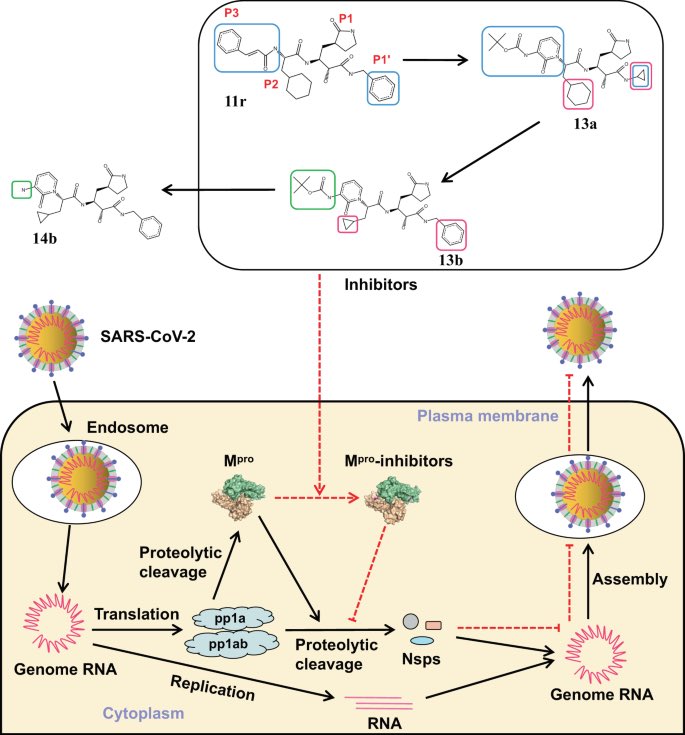
Specifically PF-07321332 binds to the catalytic site of Mpro.
Mpro is a great target because there are unique features of Mpro not found in *any* human enzymes & because spike protein mutations wouldn’t confer resistance.
In short, an ideal drug🎯
3/
medrxiv.org/content/10.110…
Mpro is a great target because there are unique features of Mpro not found in *any* human enzymes & because spike protein mutations wouldn’t confer resistance.
In short, an ideal drug🎯
3/
medrxiv.org/content/10.110…

In contrast to other SARS-CoV-2 drugs (remdesivir, Molnupiravir) which are nucleoside analogs, protease inhibition (PI) should have fewer off target effects. (E.g. No risk of mutagenesis).
Also analogous PI drugs are very effective against HIV & HCV. en.wikipedia.org/wiki/Protease_…
4/
Also analogous PI drugs are very effective against HIV & HCV. en.wikipedia.org/wiki/Protease_…
4/
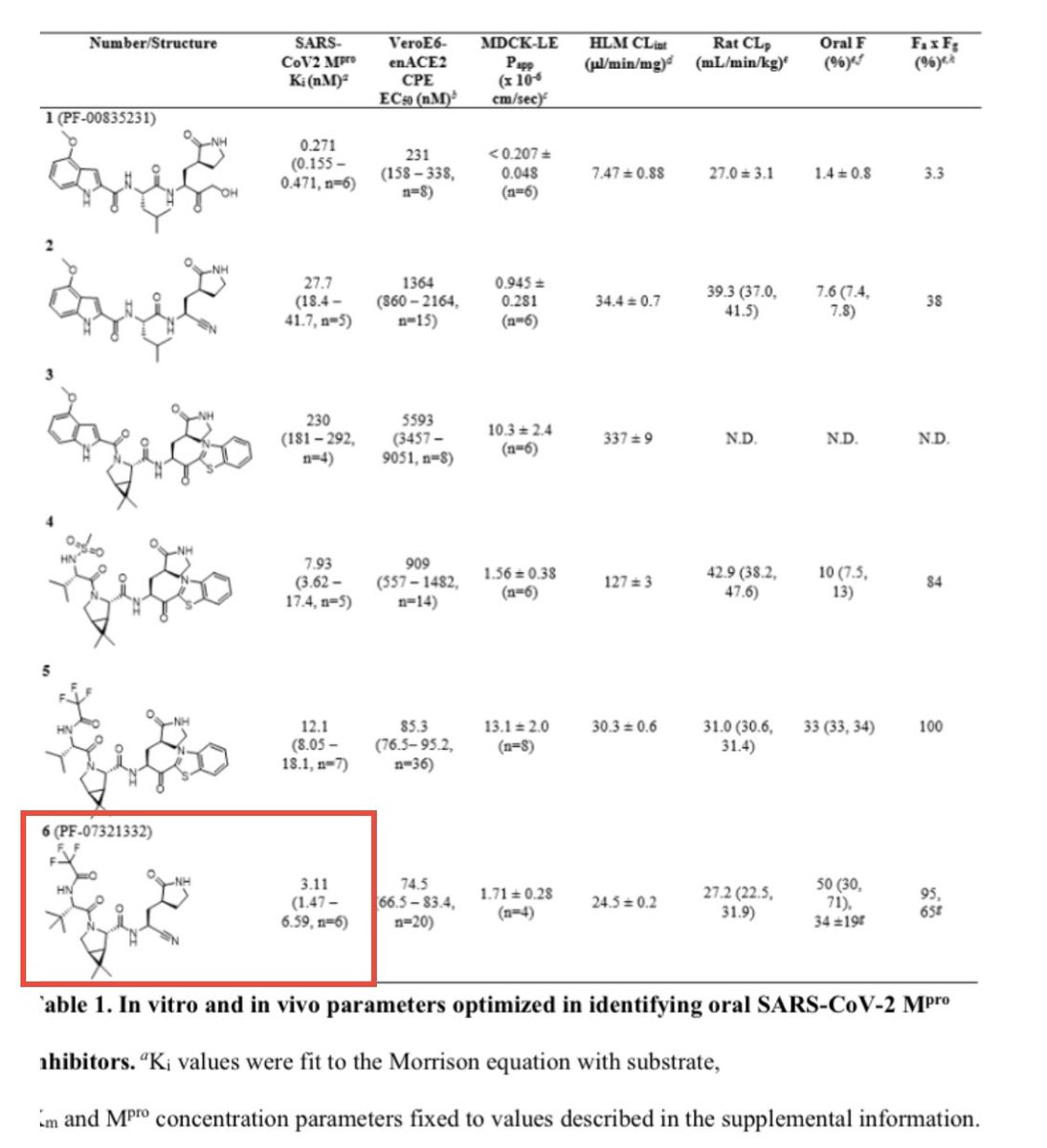
Building on work with SARS-CoV1 (which has a 100% identical Mpro catalytic site) researchers developed potent covalent inhibitors of the viral Mpro: PF-07321332
(Sidebar: “electrophilic warhead” would be an excellent name for a band)
5/
pubmed.ncbi.nlm.nih.gov/33054210/?dopt…

(Sidebar: “electrophilic warhead” would be an excellent name for a band)
5/
pubmed.ncbi.nlm.nih.gov/33054210/?dopt…


After development of candidate Mpro inhibitors in vitro, the drug showed promise in mouse models.🐁
First in human trials (NCT04756531) began in February 2021. These studies found an effective Cmax and tolerable AE profile.🤞
5/
medrxiv.org/content/10.110…
clinicaltrials.gov/ct2/show/NCT04…



First in human trials (NCT04756531) began in February 2021. These studies found an effective Cmax and tolerable AE profile.🤞
5/
medrxiv.org/content/10.110…
clinicaltrials.gov/ct2/show/NCT04…



The Evaluation of Protease Inhibition in COVID-19 High Risk Patients (EPIC-HR) study was begun in July 2021.
It was a n=3000 blinded RCT comparing PF-07321332 vs placebo. It was performed at 359 sites in the 🇺🇸 & other countries (🇧🇷🇨🇴🇯🇵 🇲🇾🇰🇷 & others)
6/
clinicaltrials.gov/ct2/show/NCT04…
It was a n=3000 blinded RCT comparing PF-07321332 vs placebo. It was performed at 359 sites in the 🇺🇸 & other countries (🇧🇷🇨🇴🇯🇵 🇲🇾🇰🇷 & others)
6/
clinicaltrials.gov/ct2/show/NCT04…
Sidebar: Why combine w/ ritonavir esp since lopinavir/ritonavir wasn't effective against COVID19?
They added Ritonavir not for anti-viral effects but to "boost" drug levels of PF-07321332 by inhibiting CYP3A. We do something analogous w/ "ritonavir boosted darunavir" in HIV.
7/
They added Ritonavir not for anti-viral effects but to "boost" drug levels of PF-07321332 by inhibiting CYP3A. We do something analogous w/ "ritonavir boosted darunavir" in HIV.
7/
EPIC-HR enrolled "high risk" COVID19 patient w/i 5 days of symptoms.
High risk was defined as ≥ 1 high risk condition by CDC criteria (cdc.gov/coronavirus/20…)
Notably they are doing similar trials in standard risk pts (EPIC-SR) & post exposure prophylaxis (EPIC-PEP)
8/
High risk was defined as ≥ 1 high risk condition by CDC criteria (cdc.gov/coronavirus/20…)
Notably they are doing similar trials in standard risk pts (EPIC-SR) & post exposure prophylaxis (EPIC-PEP)
8/

The primary endpoint of EPIC-HR was hospitalization or death within 28 days of randomization.
Secondary endpoints were pretty much what you'd expect (resolution of symptoms, clearance of virus, longer term outcomes, and adverse effects).
9/
Secondary endpoints were pretty much what you'd expect (resolution of symptoms, clearance of virus, longer term outcomes, and adverse effects).
9/

The trial record and statistical plan seem normal & rigorous.
As far as I can see no🚩 in the study design or protoocl changes. (admittedly I'm reading quickly & having worked overnight in the ICU!)
10/
As far as I can see no🚩 in the study design or protoocl changes. (admittedly I'm reading quickly & having worked overnight in the ICU!)
10/

The results of PF-07321332 vs placebo were impressive! So impressive that EPIC-HR was stopped early by IDMC/FDA at interim analysis.
Hospitalizations
6/607 (1%) vs 41/612 (6.7%) [p<0.0001]
28 Day mortality
0/389 (0%) vs 10/385 (1.6%) [p<0.0001]
pfizer.com/news/press-rel…
11/
Hospitalizations
6/607 (1%) vs 41/612 (6.7%) [p<0.0001]
28 Day mortality
0/389 (0%) vs 10/385 (1.6%) [p<0.0001]
pfizer.com/news/press-rel…
11/

Overall this was an 89% reduction in the composite outcome of death/hospitalization.
A NNT of 17 to prevent a hospitalization & a NNT of 62 to prevent a death.
& the pre-specified subgroup of patients who presented sooner (within 3 days of symptom onset) did even better.
12/
A NNT of 17 to prevent a hospitalization & a NNT of 62 to prevent a death.
& the pre-specified subgroup of patients who presented sooner (within 3 days of symptom onset) did even better.
12/
Only limited safety data provided:
Of 1881 pts, side effects "most of which were mild" were 19% w/ PF-07321332 vs 21% w/ placebo
There were fewer severe AEs w/ drug than placebo: 1.7% vs. 6.6%, & discontinuation due to side effect was more common with placebo: 2.1% vs. 4.1%
13/
Of 1881 pts, side effects "most of which were mild" were 19% w/ PF-07321332 vs 21% w/ placebo
There were fewer severe AEs w/ drug than placebo: 1.7% vs. 6.6%, & discontinuation due to side effect was more common with placebo: 2.1% vs. 4.1%
13/

Bottom line:
-the anti-viral PF-07321332 seems promising in vitro
-there were significant reductions in hospitalizations & mortality in a large phase 2/3 RCT; these are clinically meaningful effects
-I'm excited to see more data when they go to the FDA later this month!
14/14
-the anti-viral PF-07321332 seems promising in vitro
-there were significant reductions in hospitalizations & mortality in a large phase 2/3 RCT; these are clinically meaningful effects
-I'm excited to see more data when they go to the FDA later this month!
14/14
• • •
Missing some Tweet in this thread? You can try to
force a refresh
































