
🧵🚨 THREAD ALERT 🚨🧵
I think there is a misconception about hemodialysis (HD), definitely not a recipe. We have to individualize every patient; when we combine HD + plasma refilling rate (PRR) + #POCUS I can assure you, we are improving our game! All made in @NefrologiaINC
I think there is a misconception about hemodialysis (HD), definitely not a recipe. We have to individualize every patient; when we combine HD + plasma refilling rate (PRR) + #POCUS I can assure you, we are improving our game! All made in @NefrologiaINC
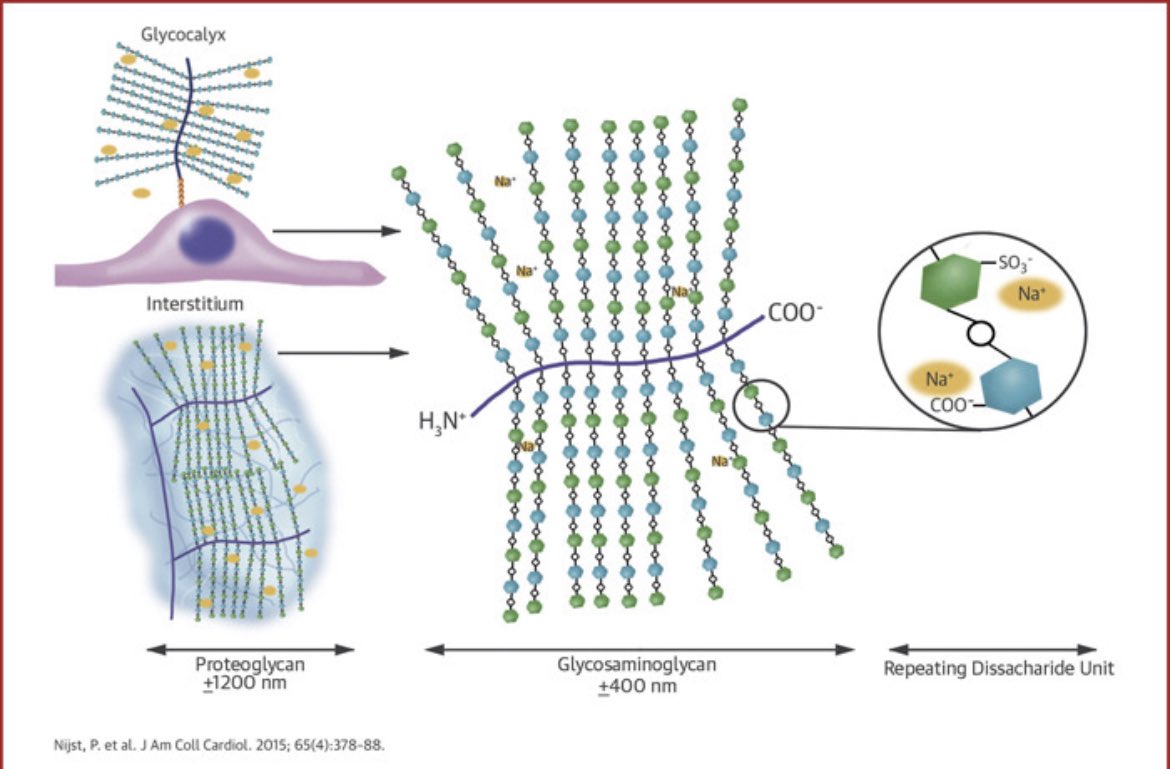
As we all know, 2/3 of total body water (TBW) is intracellular and 1/3 extracellular this last one subdivides in extravascular (75%, interstitial & lymph; connective tissue & bone; body cavities; adipose tissue), and intravascular (25%, plasma volume) DOI: 10.1681/ASN.2011080865 

What about forces governing water distribution? Starling forces pops out into our head, but we should not forget charged proteins, which generate colloid osmotic pressure (Donnan effect) favoring untenable water entry. 

However, Na/K ATPase fixes Na ions extracellulary forming double-Donnan steady state with NO transmembrane osmotic gradient. 

Finally,Aukland & Reed proposed endothelial glycocalyx as the primary interendothelial,small pore permeability barrier w/subglycocalyx oncotic pressure as the 1ry determinant of filtration;so oncotic pressure gradient is ruled by intravascular and subglycocalyx oncotic pressure.
Now, in our patients with ESKD & KRT water distribution is abnormal for so many factors, one of the main characters is the glycocalyx, which is tear by VCAM-1 and other inflammatory mediators that are increased in this population.
Some authors have established the glucocalyx as a Na-buffer and it’s rupture is associated with endothelial edema, vascular rigidity and Na leak to skin, muscle & other tissues.
Want to know more of interstitial Na? doi: 10.1016/j.jacc.2014.11.025 @FH_Verbrugge
Want to know more of interstitial Na? doi: 10.1016/j.jacc.2014.11.025 @FH_Verbrugge
Also, our patients have other manifestations of this inflammatory state:
📌 Hypoalbuminemia
📌 ⬆️ vascular permeability
📌 Poot nutritional status leading to ⬇️ lean body mass
Because of the above, achieving optimal fluid removal for an adequate volume status is challenging.
📌 Hypoalbuminemia
📌 ⬆️ vascular permeability
📌 Poot nutritional status leading to ⬇️ lean body mass
Because of the above, achieving optimal fluid removal for an adequate volume status is challenging.
Ultrafiltration rates (UFR) >10-13mL/kg/h are considered a risk factor for development of intradialytic hypotension (IDH) in patients with KRT, however PRR of each patient it’s not take into account.
One of the goals of HD is to safely remove volume excess in pursuit of the “dry weight”; as ultrafiltrate is remove from the infra vascular compartment, refilling from the interstitial and intracellular compartments ensues, in order to maintain hemodynamic stability. 

PRR can be ⬆️ w/albumin, hypertonic solutions & ⬆️ Na dialysate, however, thirst, ⬆️IDWG & HTA are some of the drawbacks with this strategy; some reports favor sequential isolated UF followed by HD to ⬆️PRR and ⬇️IDH. There isn’t much evidence of PRR in HD
Here’s an example. Let’s say we have a patient with plasma volume (PV): 4000mL (RBV 100%), 100mL of UF in 10min (RBV 99%), the expected PV (PVe) would be 3900mL, however the REAL PV (PVr) would be 3960mL (99*4000/100).
PVr-PVe = +60mL, this means that in one hour, with the same UFR = 600mL/h & PRR = 360mL/h (assuming no changes); so, PRR/UFR = 0.6 (360/600) & UFR-PRR delta = 240mL (600-360). Indicating a positive tendency of refilling rate.
An observational study done and presented in #KidneyWeek by @JuanPabloRdN in @NefrologiaINC in 30 HD patients was done, we found that UFR-PRR delta during the first 50min of the HD session was associated with IDH; no difference in UFR, PRR & PRR/UFR ratio for IDH. 

Despite principal finding in the previous study, in the general linear model of repeated measures, we found a trend toward significance between the PRR/UFR ratio and IDH (p = 0.07)
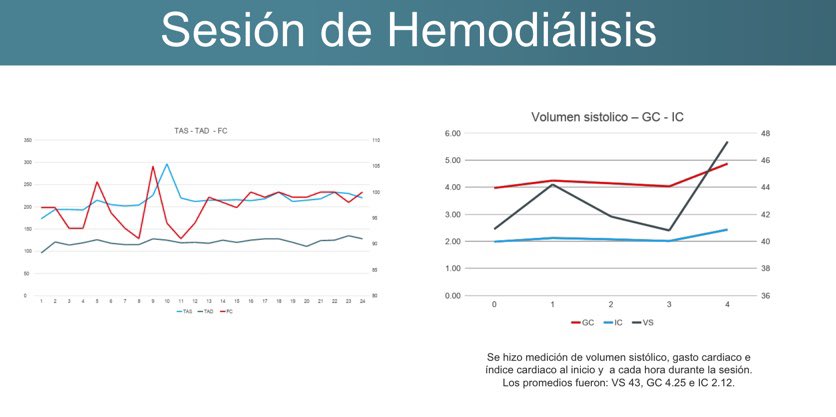
So, how do we, in @NefrologiaINC individualize every HD patient? Check out this case, 28yo male patient with uremic pericarditis & cardiac tamponade. IDWG (5.9), increased risk of hemodynamic instability.
Post-dilution HF was prescribed, 240min, we measure PRR every 10min. PRR/UFR 0.8 during the whole session, achieving UF >3000mL. Lovely graphics by @DanyXC4 

Maximal UFR was 12.3mL/kg/h with a RBV of 90% during the 240min; we monitor VS and thanks to our Chief of HD @salvadorlgil , we went beyond that and follow CO and CI, assuring hemodynamic instability. 
Bottom line, I think we should not be restraint to monitor VS during HD session, we should and MUST use all the tools we have, PRR, #POCUS (pipes, leaks and pump as @NephroP says), dry weight, bioimpedance, etc so we can provide the best for our patients
Love to hear thoughts, insights, corrections etc
@ecocritico_UTIC @salvadorlgil @JuanPabloRN @ArgaizR @ThinkingCC @khaycock2 @croncoIRRIV @TaotePOCUS @Dan_Batlle @NephroP @NephRodby @VelezNephHepato @NephroGuy @SENefrologia @NefrologiaMex @SemInDial @AJKDonline @kidney_boy
@ecocritico_UTIC @salvadorlgil @JuanPabloRN @ArgaizR @ThinkingCC @khaycock2 @croncoIRRIV @TaotePOCUS @Dan_Batlle @NephroP @NephRodby @VelezNephHepato @NephroGuy @SENefrologia @NefrologiaMex @SemInDial @AJKDonline @kidney_boy
• • •
Missing some Tweet in this thread? You can try to
force a refresh



