🧵What is GLS?
1/ It is evident that it is some measure of the systolic LV longitudinal shortening, normalised for the diastolic LV length, after the basic Lagrangian formula S = (L-L0)/L0
1/ It is evident that it is some measure of the systolic LV longitudinal shortening, normalised for the diastolic LV length, after the basic Lagrangian formula S = (L-L0)/L0

But how do we chose the numerator and denominator?
2/ The simplest measure would be LV systolic shortening / LV end diastolic length. In the HUNT 3 study, strain by this method was -17.1%. pubmed.ncbi.nlm.nih.gov/32978265/
2/ The simplest measure would be LV systolic shortening / LV end diastolic length. In the HUNT 3 study, strain by this method was -17.1%. pubmed.ncbi.nlm.nih.gov/32978265/

LV shortening can be approximated by MAPSE, so GLS is similar to MAPSE normalised for LV diastolic length. Average MAPSE of sep-lat was similar to average of sep-ant-lat-inf within the measurement accuracy in the HUNT3 study. pubmed.ncbi.nlm.nih.gov/29399886/ 

But choosing the denominator is the tricky part. Chamber length, or wall length?
4/In the HUNT3 study an approximation to wall length, was the straight lines from mitral annulus to apex. Larger denominator: Normal strain by this method was - 16.3%.
4/In the HUNT3 study an approximation to wall length, was the straight lines from mitral annulus to apex. Larger denominator: Normal strain by this method was - 16.3%.

But even that is not unambiguous.
5/ Do you draw the mid line or skewed lines to the endocardium, midway or epicardium?
5/ Do you draw the mid line or skewed lines to the endocardium, midway or epicardium?

And none of these use wall length, which is curved.
6/ Using the curved (true) wall length, would result in an even larger denominator, and a lower (absolute value) of GLS. Thus the closer we get to anatomy, the farther we move from the normal values by speckle tracking.
6/ Using the curved (true) wall length, would result in an even larger denominator, and a lower (absolute value) of GLS. Thus the closer we get to anatomy, the farther we move from the normal values by speckle tracking.

7/ Speckle tracking GLS shows normal values of -19% to - 21%. So why this discrepancy, speckle tracking should be incorporating wall curvature and follow the wall? 

8/ Looking at a speckle tracking loop, what we see is that the tracking follows both longitudinal shortening and thickening of the wall.
9/ Inward motion of the wall is due to wall thickening, and is greatest in the endocardium, less in the midwall and least in the epicardium, because the innermost layers thicken into a smaller space, and thus thickens most. This inward motion will also shorten the wall lines: 

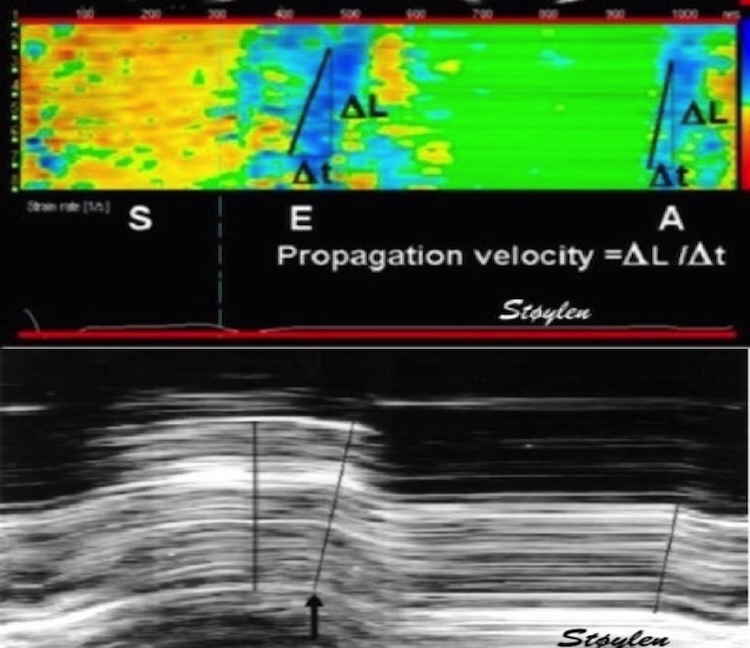
10/ Thus speckle tracking strain is a composite of longitudinal and transmural (radial) strain, and over estimates the longitudinal strain per se, and is no gold standard. This would in itself not be a problem if the method was absolutely standardised, but it isn't.
11/ Firstly, inward tracking ability depend on speckle width, which again depends on a/ the scanner generation, b/ the chosen frame rate and c/ the image quality (near shadows result in smaller virtual aperture and reduced lateral resolution). 

12/ as measured long. shortening is partly due to inward tracking, which increases towards the endocardium, longitudinal strain also depends on whether longitudinal strain is tracked a/ along the endocardium (e.g. VVI), b/ along the midline, or c/ as an average of the whole ROI
13/The shortening of longitudinal measurement due to inward motion depends on the curvature of the ROI, as illustrated by this example processed twice in the same loop 

14/ -and we haven't touched into the technical details: How are speckles weighted according to a/ intensity, b/ stability, c/ drift and d/ amount of clutter filtering and c/ smoothing (usually AV plane motion is weighted highly, ant this motion is spline smoothed along the ROI)
15/ this means:
-no universal definitions
-geometrical differences
-user differences
-technical differences that to a large degree are industrial secrets, and thus vendor differences
Thus there is no gold standard, no possibility of validating GLS, and no universal normal limits
-no universal definitions
-geometrical differences
-user differences
-technical differences that to a large degree are industrial secrets, and thus vendor differences
Thus there is no gold standard, no possibility of validating GLS, and no universal normal limits
16/ My take home message is: GLS at its present level has no objective reference outside the system used, which means both scanner, application and user. Measures are not transferrable between vendors, scanner models, analysis software or even different generation of software.
17/ Also not from one user to another, and the user should make every effort do do analysis the same way every time. Standardisation of measurements may improve reproducibility, but there is no reference for comparison, and we do not know how it works across pathologies.
18/ EF has been the entry point in trials, but the weakness of EF is that it do not diagnose reduced systolic function where LVEDV and SV ar equally reduced. Long axis finction is much more sensitive, both for diagnosis and prognosis
19/ MAPSE, measures motion of the mitral ring. It only depends on M-mode, is generic and objectively verifiable, and is sensitive for reduced myocardial function, both in HFrEF and HFpEF, both in diag. and progn. Unfortunately, it's not sexy enough, so the GLS trials dominate. 

• • •
Missing some Tweet in this thread? You can try to
force a refresh