🧵What’s layer strain, and what does it mean? With speckle tracking, the ROI can be divided into layers, and strain measured selectively in each layer, both longitudinal strain in apical views, and circumferential strain in short axis views. But what is this actually?
Strains differ between layers, but the difference is NOT due to differences in fibre function in the different layers, it is again a function of geometry. 

1/ 1/ starting with circumferential strain, which is conceptually easiest, in the HUNT study, with linear strains, we found outer Sc ca 13%, midwall Sc ca 23% and endocardial Sc 36%, so there is a clear gradient of Sc across the wall. pubmed.ncbi.nlm.nih.gov/31673384/
2/ In the previous thread on strain in three dimensionshttps://twitter.com/strain_rate/status/1459845380414353415?s=20, I showed Sc to mainly be a function of wall thickening, except the outer Sc, which is circumferential fibre shortening. 

3/ let's look at that in more detail: Outer Sc pushes the myocardium inwards, where cross sectional area is smaller. Thus the wall will thicken a bit as the circumference decreases . And this wall thickening will push the endocardium more inwards that the outer. 

4/ In addition to that, of course there is wall thickening due to the longitudinal shortening, as explained in the previous thread
This will push the endocardium even further inwards.
https://twitter.com/strain_rate/status/1459845380414353415?s=20.
This will push the endocardium even further inwards.

5/ Consider the wall as two layers, separated by the midwall circumference. Outer layer expands due to being pushed inwards from circumferential shortening and thickens from longitudinal shortening. Thus midwall circumference, is pushed further inwards, and thus, shortens more. 

6/ The outer layer will push the inner layer into an even smaller space, so the inner layer has to thicken even more, in addition to also thickening from longitudinal shortening, so it thickens more than the outer, expanding in a smaller space 

7/ So there is a gradient of Sc across the wall but due to geometry, not differential fibre function. In the previous thread, I showed that Sc = relative diameter shortening. 

8/ Midwall Sc is closest to mean wall Sc as measured by speckle tracking. But as it can be estimated by diameter shortening, In M-mode midwall diameter shortening will be: Sc = (((IVSd + LVPWd)/2 + LVIDd) - ((IVSs + LVPWs)/2 + LVIDs))/ ((IVSd + LVPWd)/2 + LVIDd) 

9/ the gradient of Sc across the wall, will simply be the ratio of endocardial Cs / Outer Cs: Outer Sc = ((IVSd + LVPWd + LVIDd) - (IVSs + LVPWs + LVIDs))/ (IVSd + LVPWd + LVIDd), endocardial Sc = (LVIDd - LVIDs) / LVIDd. 

10/ The gradient may give additional information, as a function of both longitudinal shortening, circumferential fibre shortening, wall thickness and LV diameter, but the concept "layer strain" is erroneous, as the gradient is continuous.
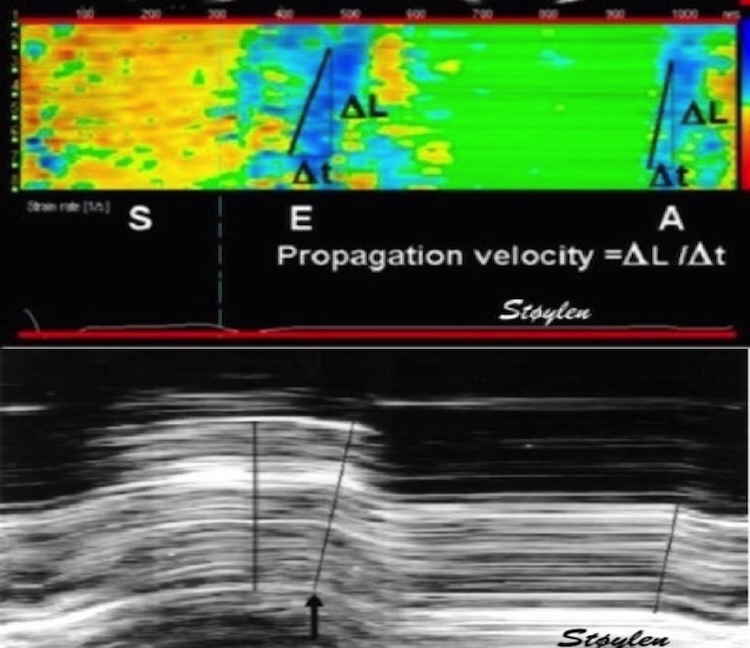
Now let’s look at longitudinal layer strain, which has also been reported with a gradient from outer to inner. As stated in a previous thread on GLS,
https://twitter.com/strain_rate/status/1458458025056997378?s=20, ST based LS, do not only track in the longitudinal direction, but also in the inward direction
This inward tracking means that the longitudinal shortening adds a shortening due to inwards motion as well, so ST based GLS overestimates the true shortening. In fact, there would have been apparent shortening even without shortening of the LV 

12/ This effect is not due to curvature, but as the lines move inwards in a cone, they become shorter. 

13/ As the wall thickens, the midwall line moves more inwards than the outer, and the endocardial line moves more inwards than the midwall. Thus the ST based GLS incorporates more of this artefact towards the endocardium. 

14/ Just consider the absurdity if there had been more longitudinal shortening in the endocardium, the mitral ring would have torsion. And as the mitral ring is a part of the fibrous AV-plane this would make total havoc with the structure of the heart! 

unroll @threadreaderapp
• • •
Missing some Tweet in this thread? You can try to
force a refresh