
28 November: ROS1, single arm trials
For Lung Cancer Awareness Month #LCAM I’m going to summarize 30 important lung cancer trials over 30 days. These posts are directed at non-medical professionals, with descriptions of the results and of what makes a good trial. #lcsm 1/15
For Lung Cancer Awareness Month #LCAM I’m going to summarize 30 important lung cancer trials over 30 days. These posts are directed at non-medical professionals, with descriptions of the results and of what makes a good trial. #lcsm 1/15
This month I have focused exclusively on randomized studies, because I believe strongly that they are our best tools for evaluating the benefits and harms of cancer therapies. Today will be my sole foray into non-randomized studies. I hope to illustrate some of their limitations. 



In a single-arm study, every patient receives the study treatment. A common method of describing drug activity is the waterfall plot, below. Each bar on the plot is an individual patient. The height and direction of the bar show how the size of the tumours changed with treatment. 
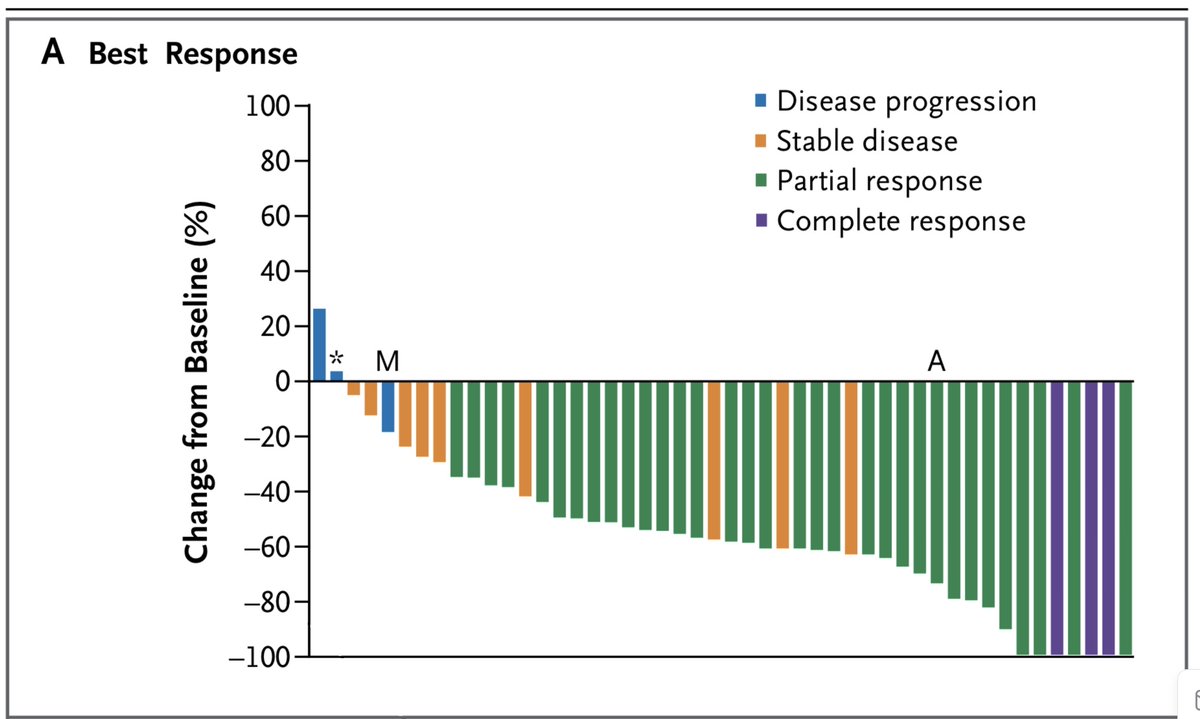
The horizontal bar at zero indicates the tumour neither grew nor decreased. Bars below the line indicate tumours that decreased in size by the percentage indicated on the vertical axis. Similarly, bars above the line indicate tumours that grew despite treatment.
4/15
4/15
The responses are arranged in order from worst to best, to give the “waterfall” appearance. In the example above, only two patients had their tumours grow after starting treatment. By convention, those who have had their tumour shrink by >30% are said to have had a response.
The other information often given is a KM curve (5, 16 Nov). Obviously, there is only one curve, not two like the others we’ve seen this month. In the example below the grey bars are 95% confidence intervals (10 Nov) around each point. 6/15 
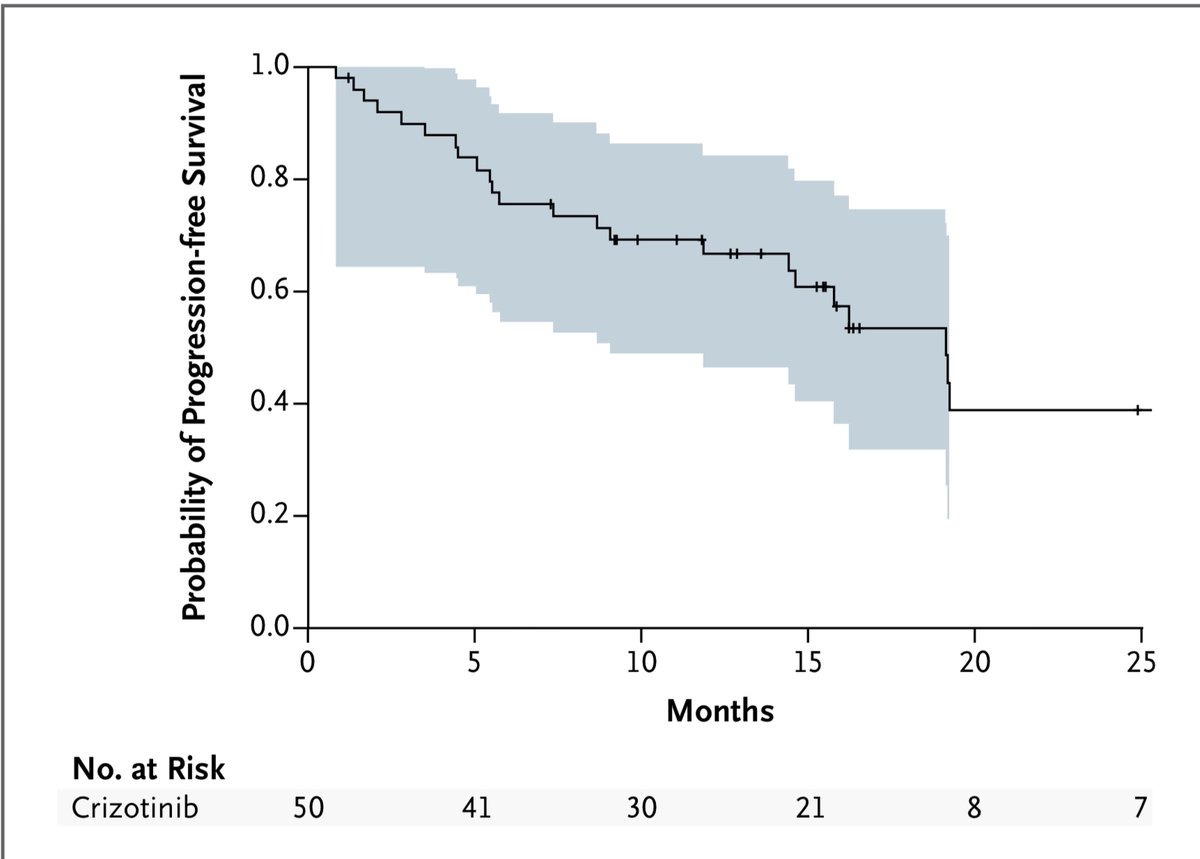
Both of the examples above are from a study of crizotinib in people with ROS1 mutated cancers. Below are the waterfall plot and KM curve for a study of entrectinib in the same cancer. Note FWIW not an intention-to-treat population, but people who got a certain amount of drug.7/15 

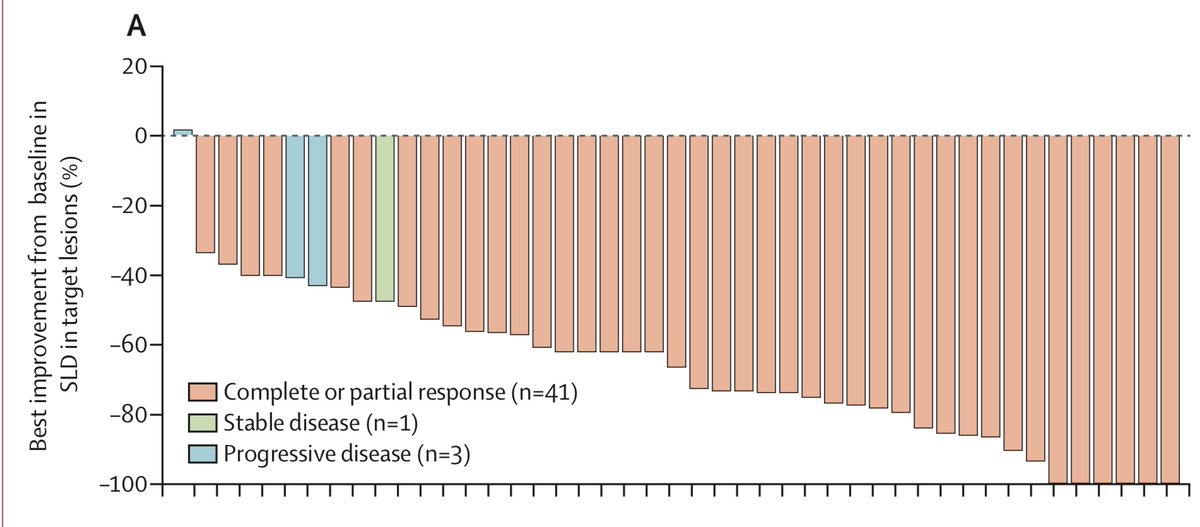

On the basis of these graphs, do you feel confident in saying that these drugs are all comparable, or that one or the other is likely superior? I admit that I do not. We go back to the papers, trying to find differences in toxicity, or in patient selection between trials. 9/15
Even if one drug were obviously superior, would it be better to take it alone, or in sequence with another drug? Are any of these drugs better than standard chemotherapy? We look for answers in vain. These answers come from randomized studies. 10/15
Since 2013 the FDA has approved numerous drugs on the basis of such non-randomized data. This has the advantage of getting the drug to patients more quickly. The disadvantage is that once regular approval is granted, pharma has no more incentive to do trials of the drug. 11/15 

To me, this seems a steep price to pay. Hundreds of patients today may access the drug sooner, but thousands of patients in the future will have to make decisions about these drugs with scant evidence about their relative effectiveness or survival outcomes. 12/15
I'm sensitive to the idea that it would be difficult to do a large randomized trial in rare cancer like ROS-1 lung cancer (~2% of lung cancers).
I would counter that initial randomized trials in ALK (~3% of lung ca) were feasible at a time when most hospitals didn’t test for ALK.
I would counter that initial randomized trials in ALK (~3% of lung ca) were feasible at a time when most hospitals didn’t test for ALK.
Many TKIs for driver-mutated lung cancer are excellent drugs: many people have long responses with manageable side effects. Other TKIs have lower response rates or worrying toxicity.
The absence of randomized data impairs our ability to rationally use these new drugs. 14/15
The absence of randomized data impairs our ability to rationally use these new drugs. 14/15
Though I’ve focused on ROS1, I could have written a similar thread about RET, NTRK, METex14, or any driver mutation with multiple available TKIs.
Tomorrow we’ll take a look at a study design somewhere between single-arm and full randomized trial, the randomized phase II trial.
Tomorrow we’ll take a look at a study design somewhere between single-arm and full randomized trial, the randomized phase II trial.
• • •
Missing some Tweet in this thread? You can try to
force a refresh














