Session 3 of #BacktoHeart21 happening now and covering #Lipids moderated by @FaRodriguezMD @PamelaBMorris & @DLBHATTMD!
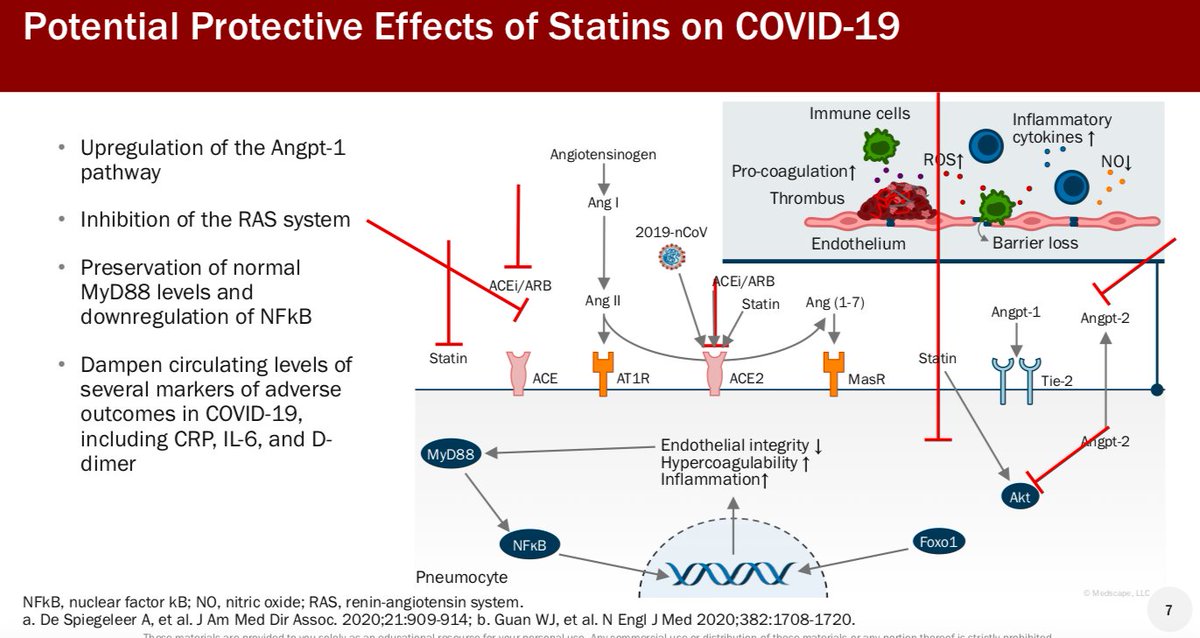
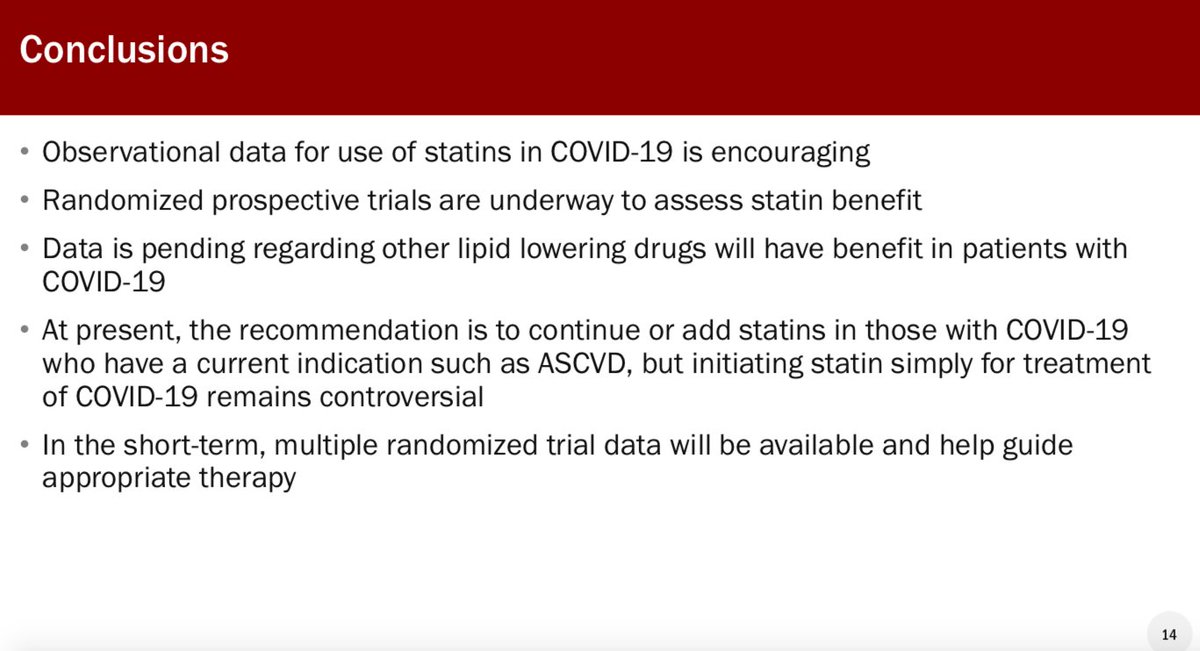
First up @alanbrownmd covers COVID-19 and statin therapy! Promising observational data and many RCTs ongoing!
@MedscapeLIVE



First up @alanbrownmd covers COVID-19 and statin therapy! Promising observational data and many RCTs ongoing!
@MedscapeLIVE


@FaRodriguezMD @PamelaBMorris @DLBHATTMD @alanbrownmd @MedscapeLIVE Next up @PamelaBMorris discusses lipid lowering beyond statins!
More data to come for bempedoic acid, Evinacumab, and Inclisiran! Lots of options emerging for LDL lowering



More data to come for bempedoic acid, Evinacumab, and Inclisiran! Lots of options emerging for LDL lowering




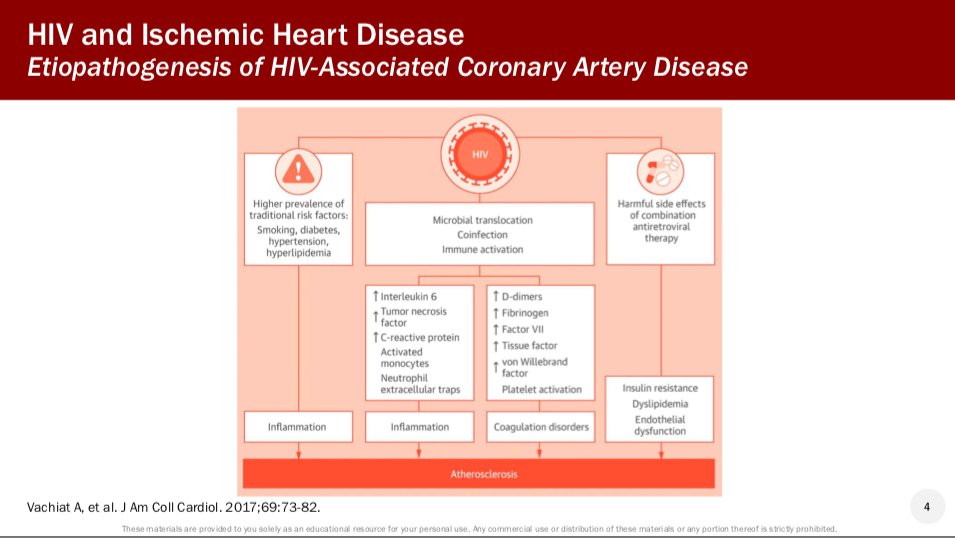
@FaRodriguezMD @PamelaBMorris @DLBHATTMD @alanbrownmd @MedscapeLIVE @DrRSRosenson provides a expert review of HIV and ischemic heart disease!
> HIV patients have high rates of CV events
> Lipid lowering therapy are underutilized
> 1/4 patients are treated with contraindicated statins or doses



> HIV patients have high rates of CV events
> Lipid lowering therapy are underutilized
> 1/4 patients are treated with contraindicated statins or doses



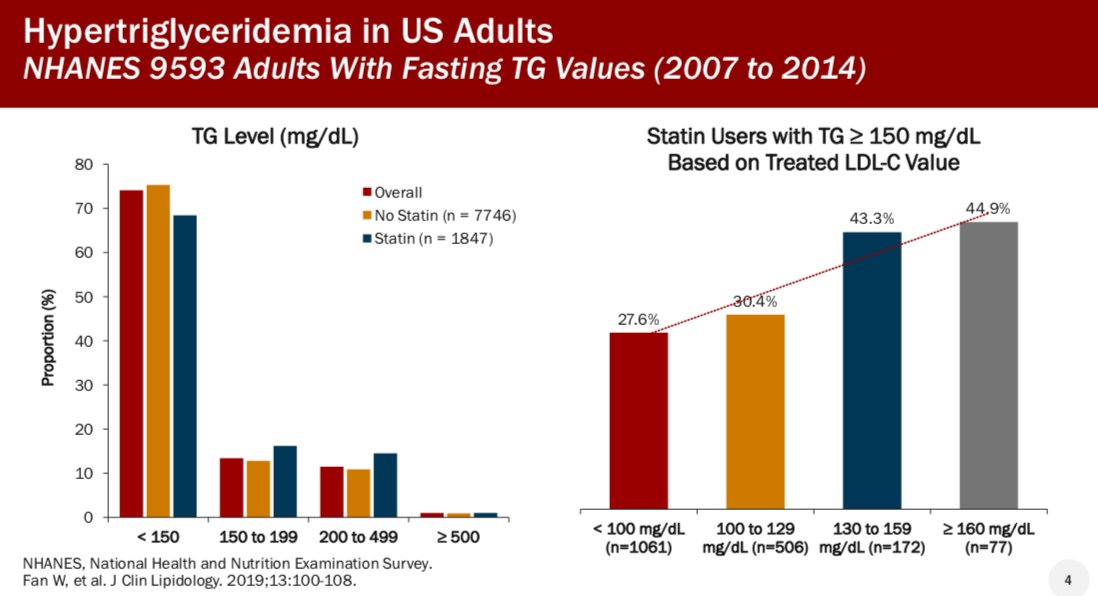
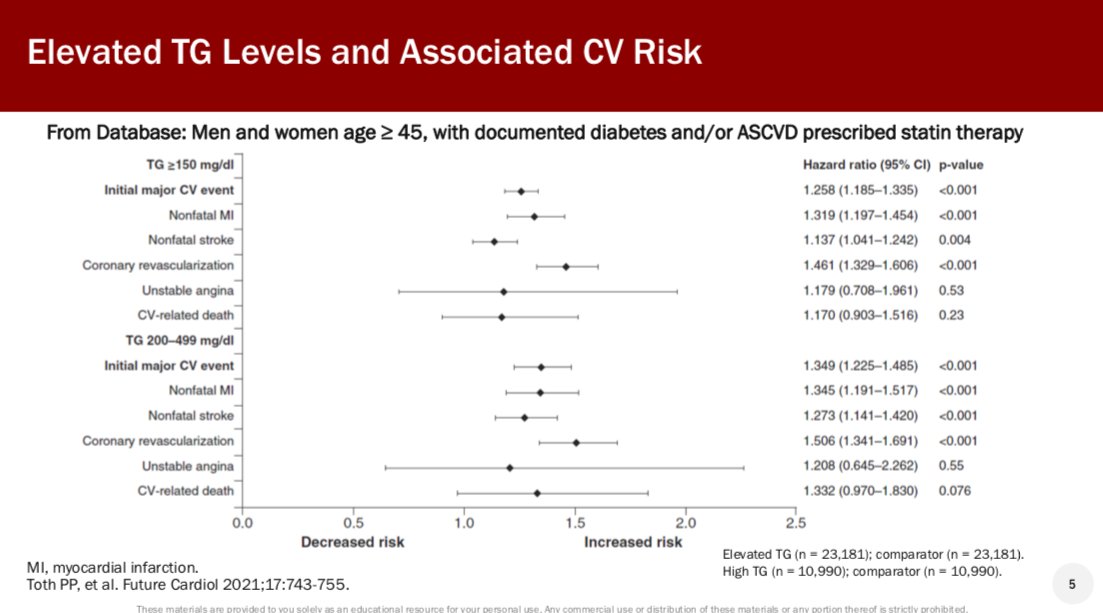
@FaRodriguezMD @PamelaBMorris @DLBHATTMD @alanbrownmd @MedscapeLIVE @DrRSRosenson @JSaseenPharmD discussed TG lowering therapy and CV disease!
> EPA only omega 3 products beneficial with significant reduction in CV events demonstrated in the REDUCE-IT trial
> Be mindful of the increased risk of AF



> EPA only omega 3 products beneficial with significant reduction in CV events demonstrated in the REDUCE-IT trial
> Be mindful of the increased risk of AF

@PamTaubMD discusses primary prevention for high-risk patients
> Dr. Taub makes a strong argument for incorporting more biomarkers beyond LDL to guide risk and management
> More personalized management needed to prevent events!



> Dr. Taub makes a strong argument for incorporting more biomarkers beyond LDL to guide risk and management
> More personalized management needed to prevent events!




@DLBHATTMD provides a masterclass overview on antiplatelet and anticoagulant therapy for CVD to wrap up the session!
Dr. Bhatt discusses duration of DAPT & addition of low dose anticoagulation for stable CAD!
#BacktoHeart21



Dr. Bhatt discusses duration of DAPT & addition of low dose anticoagulation for stable CAD!
#BacktoHeart21




• • •
Missing some Tweet in this thread? You can try to
force a refresh