
1/ #EmoryNCCTweetorials 🚨
The setup: Neuro ICU at @EmoryNeuroCrit
The pt: John Doe transferred for status epilepticus
You’re told about the pt’s ammonia lvl ➡️ 181 (where's @Capt_Ammonia?!). He’s also on 5 different AED’s...
@MedTweetorials
#MedEd #tweetorial #neurotwitter
The setup: Neuro ICU at @EmoryNeuroCrit
The pt: John Doe transferred for status epilepticus
You’re told about the pt’s ammonia lvl ➡️ 181 (where's @Capt_Ammonia?!). He’s also on 5 different AED’s...
@MedTweetorials
#MedEd #tweetorial #neurotwitter
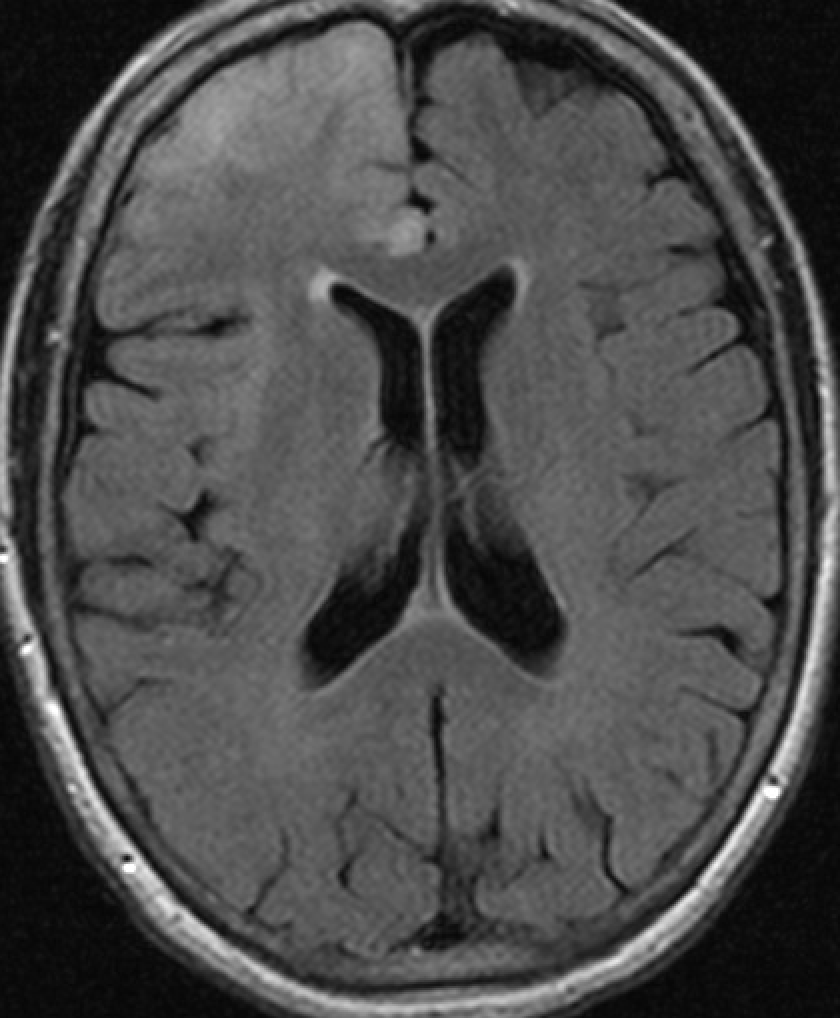
2/ On quick review, patient was admitted 5 days earlier at the OSH. Initially admitted for encephalopathy that was then c/b seizures the following day. Initial ammonia was normal. CT/CTA unremarkable. MRI brain w/ contrast shows the following abnormality over the R frontal area 


3/ Further hx significant for excessive EtOH (~2-3 glasses of wine/day). Recently in the mountains drinking homemade moon shine. He had nausea and vomited ~24-48 hrs later before becoming encephalopathic. Eventually admitted ~4 days later.
4/ You take a quick look at his EEG. Thankfully you have an amazing epileptologist @DeniseFChen helping you out for the day 



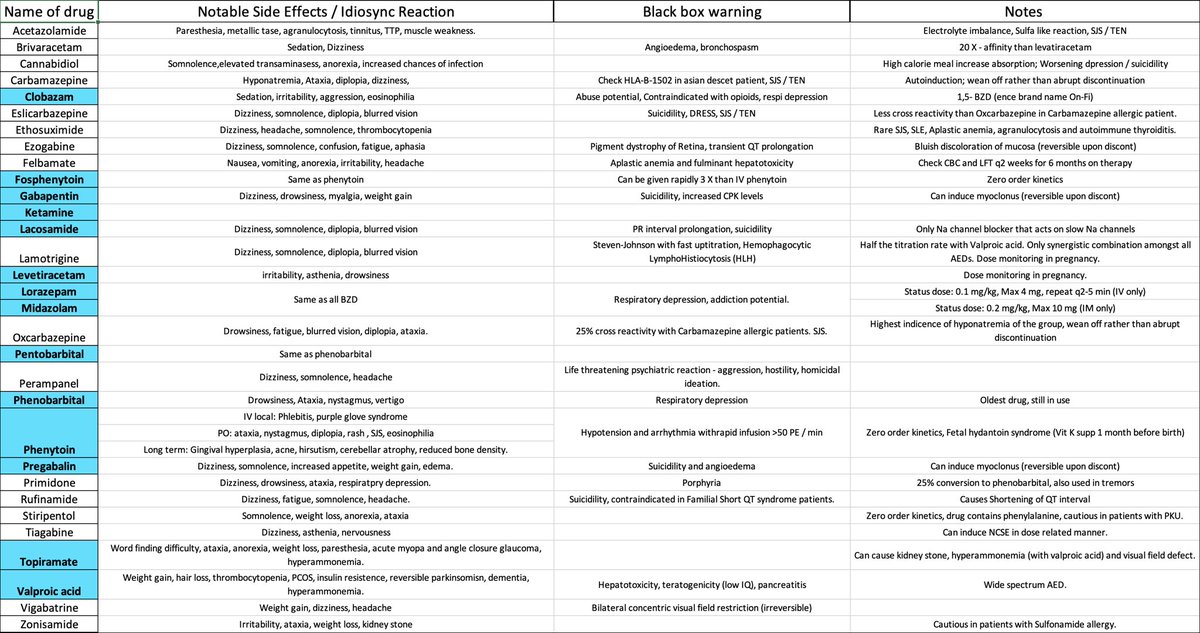
5/ A quick look at his current medications ➡️ fosphenytoin, keppra, valproic acid, and a versed gtt along with acyclovir. You quickly d/c valproic acid given his ammonia level…thank you @JayKinariwala for the beautiful AED cheatsheet

6/ Extensive workup was unremarkable.
LP x2 showed a bland CSF profile w/o any concerns of bacterial/viral/fungal etiologies. Cytology and flow negative. HSV negative x4 . Anti TPO and TG normal. Crypto negative. Encephalopathy, Autoimmune, and Paraneoplastic panel negative.
LP x2 showed a bland CSF profile w/o any concerns of bacterial/viral/fungal etiologies. Cytology and flow negative. HSV negative x4 . Anti TPO and TG normal. Crypto negative. Encephalopathy, Autoimmune, and Paraneoplastic panel negative.
7/ You decide to make a quick differential
1. Alcohol withdraw seizures (AWS)
2. Marchiafava-Bignami disease (MBD)
3. Primary or Secondary tumor
4. HSV encephalitis (HSV)
5. Wernicke encephalopathy (WE)
6. Hepatic encephalopathy (HE)
1. Alcohol withdraw seizures (AWS)
2. Marchiafava-Bignami disease (MBD)
3. Primary or Secondary tumor
4. HSV encephalitis (HSV)
5. Wernicke encephalopathy (WE)
6. Hepatic encephalopathy (HE)
8/ So which one is it? 🤔
9/ Let's think about each one...
1⃣ AWS usually occurs ~24-72 hrs after cessation w/ seizures being more generalized (EEG and MRI findings as well).
2⃣ MBD characteristically has the corpus callosum involved on MRI.
3⃣ Primary/Secondary tumors usually progress on repeat imaging.
1⃣ AWS usually occurs ~24-72 hrs after cessation w/ seizures being more generalized (EEG and MRI findings as well).
2⃣ MBD characteristically has the corpus callosum involved on MRI.
3⃣ Primary/Secondary tumors usually progress on repeat imaging.
10/
4⃣ HSV often involves the medial temporal lobes +/- possible xanthochromia on LP.
5⃣ WE = typical triad of confusion, ataxia, and nystagmus from thiamine deficiency.
6⃣ HE commonly causes a DWI restriction pattern of the cortex + thalamus + cingulate gyrus.
4⃣ HSV often involves the medial temporal lobes +/- possible xanthochromia on LP.
5⃣ WE = typical triad of confusion, ataxia, and nystagmus from thiamine deficiency.
6⃣ HE commonly causes a DWI restriction pattern of the cortex + thalamus + cingulate gyrus.
11/ As you’re trying to decide which is the likely culprit, @CaseyAlbin walks up and drops some great knowledge as always. “I wonder if he has SESA.”
It takes you a few seconds to process it...wait what?
Did she say sista, sissy, or see-saw? What in the world is SESA?
It takes you a few seconds to process it...wait what?
Did she say sista, sissy, or see-saw? What in the world is SESA?
12/ Subacute Encephalopathy and Seizures in Alcoholics or SESA was first described by Niedermeyer in 1981. It’s a rare neurologic disorder complicating the chronic abuse of alcohol. It p/w neuro deficits, encephalopathy, & seizures / IIC!
13/ The key here is the severe lateralized abnormalities on EEG.
These patients are persistently altered because of ongoing NCSE or IIC!
These patients are persistently altered because of ongoing NCSE or IIC!
14/ This is a can’t miss alcohol-related diagnosis because it is potentially reversible with treatment of the ictal patterns, even if those patterns are progressing to frank seizures.
As the ictal patterns are treated, patients and their radiographs improve!
As the ictal patterns are treated, patients and their radiographs improve!
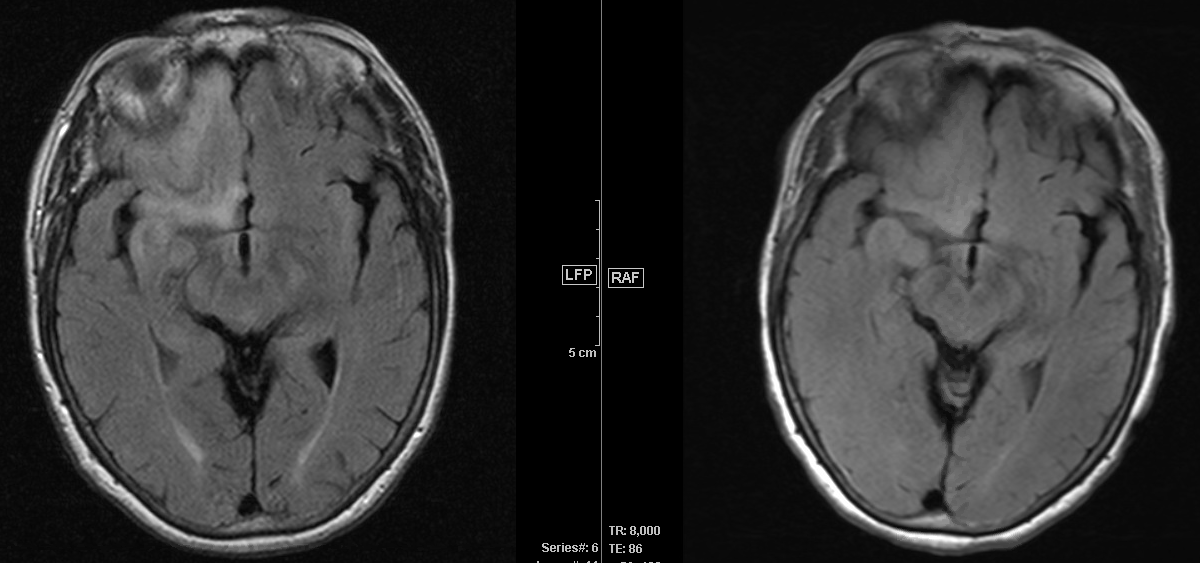
15/ A repeat MRI w/ contrast 1 week later shows interval improvement over the R frontal area and is shown below (more recent one on the left, older one on the right for comparison). 






16/ The patient was eventually extubated and slowly returned to his baseline. He was weaned to just one AED and ultimately discharged to rehab without any further complications.
17/ Thankfully we already had some great highlights on EtOH and some of it’s effects on the brain
https://twitter.com/caseyalbin/status/1461085413423173634
18/ Here are two great papers below
☑️ Reviewing image findings of SESA sciencedirect.com/science/articl…
☑️ Highlighting the differences between SESA and EtOH withdraw seizures
ncbi.nlm.nih.gov/pmc/articles/P…
☑️ Reviewing image findings of SESA sciencedirect.com/science/articl…
☑️ Highlighting the differences between SESA and EtOH withdraw seizures
ncbi.nlm.nih.gov/pmc/articles/P…
19/ Next time you see an EtOH patient with encephalopathy and seizures with abnormal EEG findings (especially if unilateral) +/- image abnormalities, make sure you drop some great knowledge by adding SESA to the differential!
20/ And as always, a big thank you to @CaseyAlbin and @CajalButterfly
@mallyaa @sigman_md @EricLawson90 @maness_caroline @JayKinariwala @JackieKraft4 @neuro_intensivist @Capt_Ammonia @DeniseFChen @Raf_Perz @drhibahaider @EmoryNeurology
@mallyaa @sigman_md @EricLawson90 @maness_caroline @JayKinariwala @JackieKraft4 @neuro_intensivist @Capt_Ammonia @DeniseFChen @Raf_Perz @drhibahaider @EmoryNeurology
• • •
Missing some Tweet in this thread? You can try to
force a refresh



