
1/ I enjoyed this chat with @hubermanlab and @davidasinclair - two very knowledgeable scientists that I have enormous respect for.
I would like to clarify one thing when it comes to cholesterol and heart disease risk that came up in this exchange (and daily on Twitter)
I would like to clarify one thing when it comes to cholesterol and heart disease risk that came up in this exchange (and daily on Twitter)
https://twitter.com/davidasinclair/status/1475548294680125445
2/ There’s a lot of confusion online about dietary cholesterol, serum cholesterol and heart disease. I hope to clarify a few points here. It’s important as this is the number one cause of death globally - impacting healthspan and lifespan.
3/ Firstly, the mechanism by which elevated LDL cholesterol (LDL-C) increases risk of atherosclerotic CVD is by increasing the # of circulating ApoB containing lipoproteins.
pubmed.ncbi.nlm.nih.gov/27472409/
pubmed.ncbi.nlm.nih.gov/27472409/
4/ApoB is a protein on LDL (& other) lipoproteins that causes the particles to get trapped (retained) in the artery wall. Over time this leads to fatty plaque building up that can obstruct blood flow to the heart or brain depending on the vessel/s involved.
5/ Genetic studies, observational studies and RCT’s unequivocally show that elevated LDL-C, and more specifically ApoB, CAUSES atherosclerosis. Yes this is considered adequate evidence to make a causal claim.
pubmed.ncbi.nlm.nih.gov/27472409/
pubmed.ncbi.nlm.nih.gov/27472409/
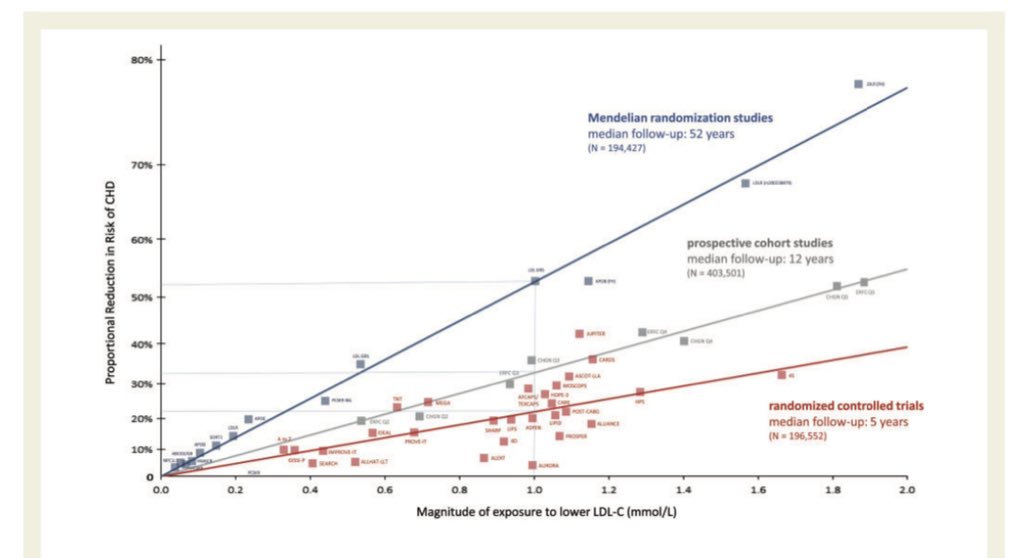
6/ While it’s true observational research shows lower LDL-C is associated with increased mortality this finding is not consistent with higher quality evidence - genetic and RCT data shows lower LDL-C = reduced mortality.
7/ Further to this we know from that at ApoB levels of 80-90mg/dL and lower you rarely see atherosclerosis. We also know from RCT’s when you lower someone’s ApoB below this level you can see regression of atherosclerosis.
8/ When it comes to diet what elevates ApoB? Sat fats & trans fats are the biggest culprits.
(Note* not all sat fats raise ApoB to the same degree, or at all. E.g stearic acid as found in chocolate doesn’t seem to appreciably elevate ApoB)
(Note* not all sat fats raise ApoB to the same degree, or at all. E.g stearic acid as found in chocolate doesn’t seem to appreciably elevate ApoB)
9/ Research stemming back to the 1950s has unearthed this in highly controlled metabolic ward trials.
pubmed.ncbi.nlm.nih.gov/9006469/
pubmed.ncbi.nlm.nih.gov/9006469/
10/ What about dietary cholesterol? Does this raise LDL-c & ApoB? Yes but to a lesser extent to saturated/trans fats & importantly the dose response relationship is NON-LINEAR. Once you go above approx 400-500mg a day of dietary cholesterol it not longer raises serum cholesterol.
11/ However, given the average (‘normal’) ApoB levels are well above levels where we do not see atherosclerosis, reducing dietary cholesterol towards 0mg is a tool that can be clinically meaningful for certain individuals at high risk of cvd.
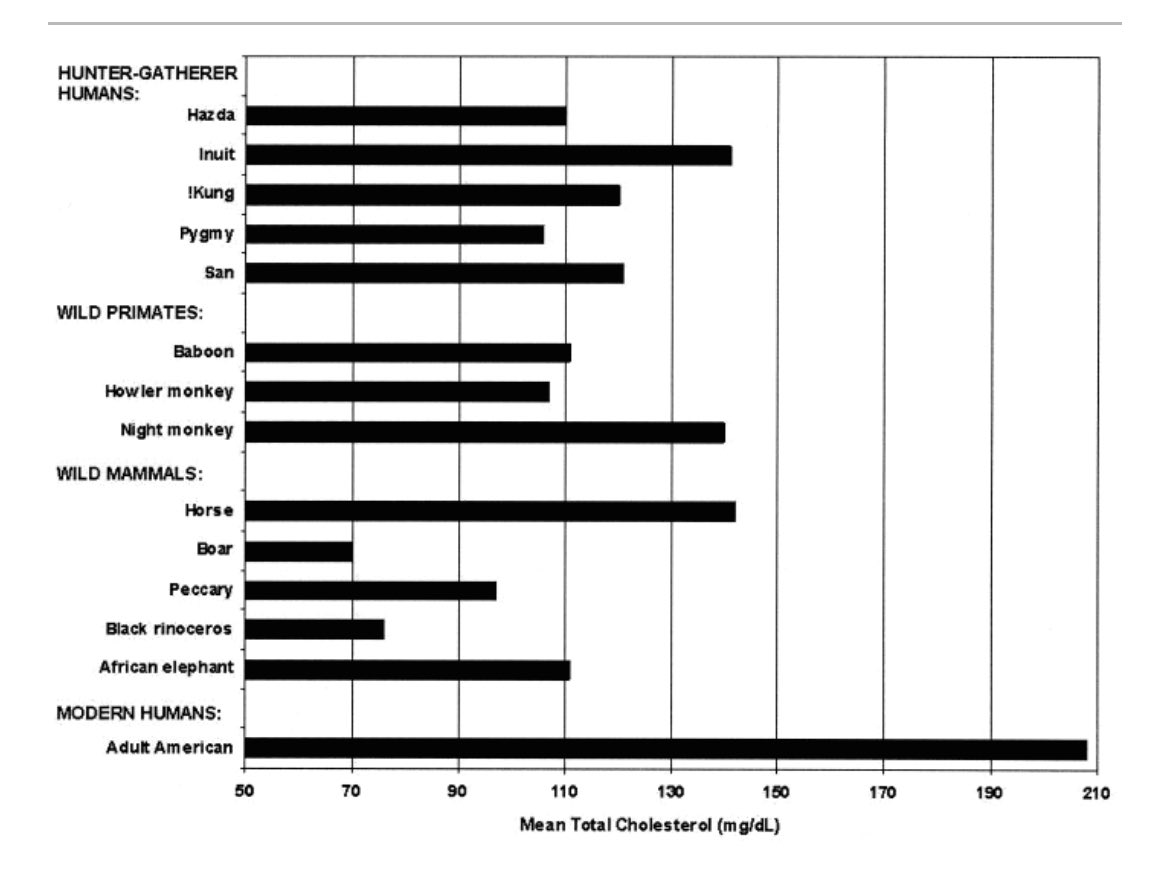
12/ You can see in this paper how our current LDL-C levels are greater than that of hunter gatherers and non-human primates. This is a peer reviewed paper published by father of the Paleo Diet Loren Cordain.
pubmed.ncbi.nlm.nih.gov/17663803/
pubmed.ncbi.nlm.nih.gov/17663803/
13/ People often wonder about plant fats. How do they affect serum cholesterol/ApoB? The tropical oils (coconut/palm) raise ApoB. Whereas unsaturated fats, particularly polyunsaturated fats (nuts, seeds, some oils) lower cholesterol and ApoB levels.
14/ What’s this mean for risk management? If you can - ask your physician for an ApoB test. While non-HDL and LDL-C are generally good measures of cvd risk, ApoB is more reliable across an entire population due to reasons I won’t go into here.
15/ Point being - ApoB is the gold standard test for determining the level of atherogenic lipoproteins circulating in your blood. Non-HDL would be the second best option.
16/ Side note: Observational studies show higher HDL-C = lower risk of CHD but genetic & RCTs show clearly that raising HDL-C does not lower risk. A clear example of a biomarker that’s associated with risk but not part of of the causal chain. This is a regular point of confusion.
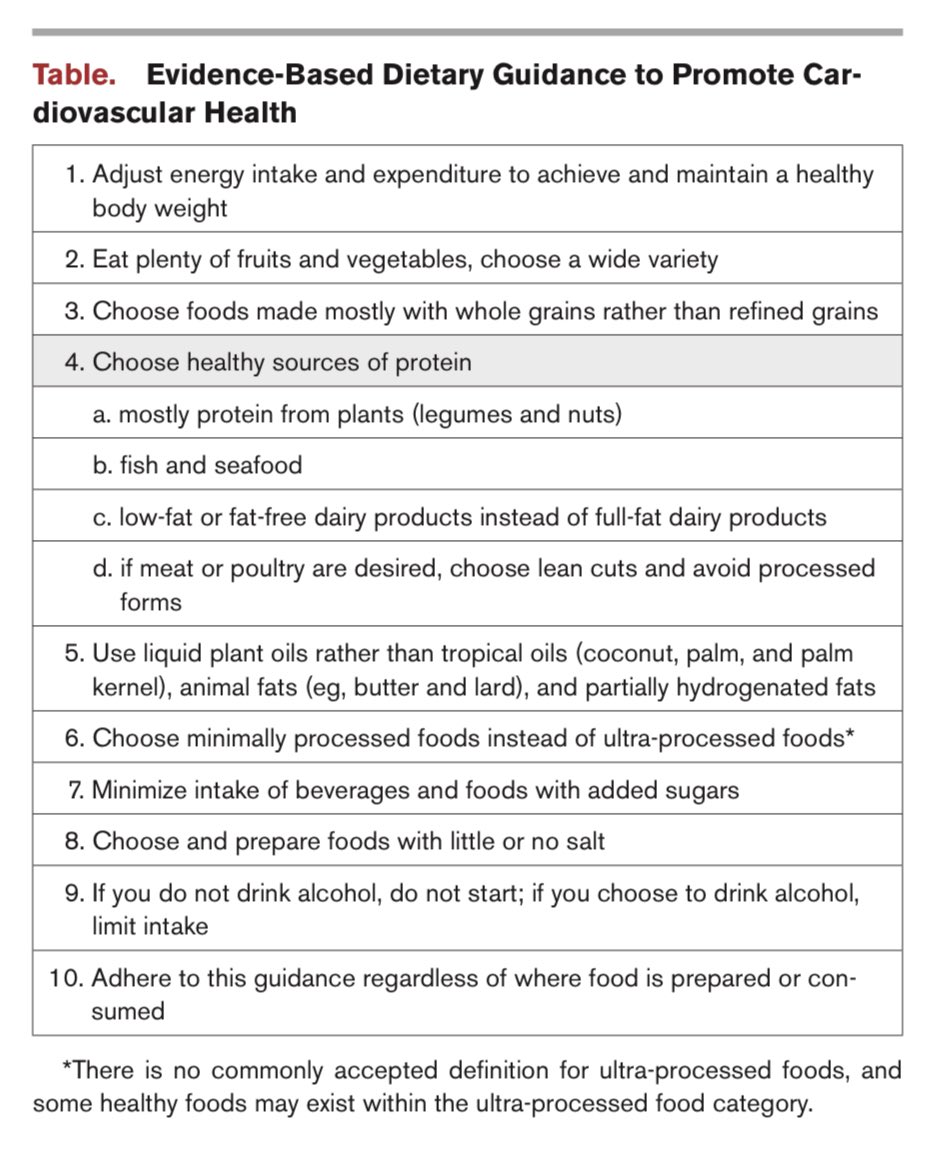
17/ Back to ApoB. If your ApoB is high you can discuss pharmaceutical management with your physician. Based on your presentation it may be required it may not be. Additionally there are dietary changes you can make to lower ApoB. What do these look like?
18/
1- Swap red and white meat for legumes (e.g lentils, chickpeas, beans) and fatty fish (if you eat seafood). Depending on your goal, a few times a week or daily.
2 - Swap animal fats for non-tropical plant fats. E.g butter for olive/canola/avocado oil.
1- Swap red and white meat for legumes (e.g lentils, chickpeas, beans) and fatty fish (if you eat seafood). Depending on your goal, a few times a week or daily.
2 - Swap animal fats for non-tropical plant fats. E.g butter for olive/canola/avocado oil.
19/
3- Eat more sources of soluble fibre. Nuts, seeds, oats, eggplant, apple, berries etc
3- Eat more sources of soluble fibre. Nuts, seeds, oats, eggplant, apple, berries etc
20/ I’m a big fan of the Portfolio Diet which has been designed and clinically tested by Dr David Jenkins. It focusses on what you ADD versus what you remove. Data suggests following this can lower your LDL-C by approx 30% which will have a meaningful affect on ApoB. 
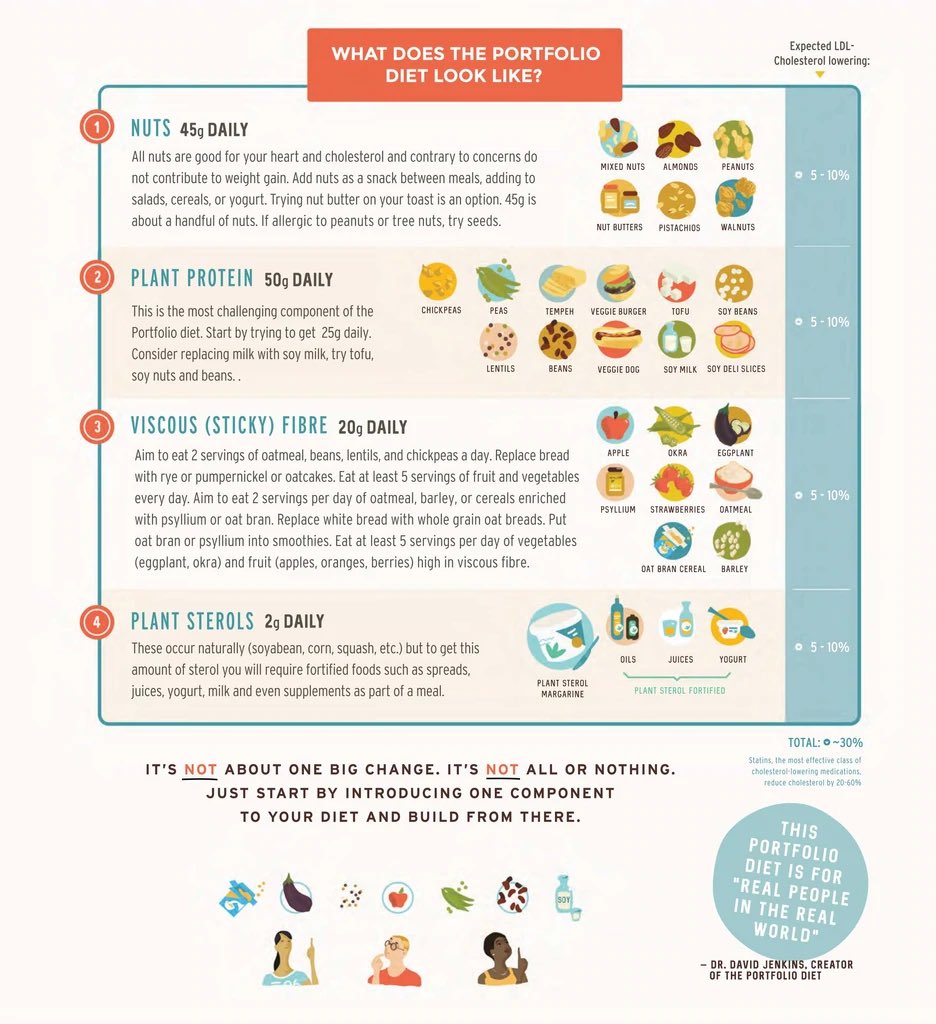
21/ Here is one clinical study showing the Portfolio Diet intervention was comparable in its effect on cholesterol to a statin. This speaks to the power of dietary changes.
pubmed.ncbi.nlm.nih.gov/17663803/
pubmed.ncbi.nlm.nih.gov/17663803/
22/ Again - statins, or other lipid lowering drugs, may be required in addition to dietary changes. These drugs have been proven to be very effective. And while all drugs have side effects the online rhetoric against statins is not supported by the evidence.
24/
In summary get your ApoB tested. If it’s elevated (particularly above 100mg/DL) devise a plan with your physician/cardiologist to get it down to a more favourable level.
In summary get your ApoB tested. If it’s elevated (particularly above 100mg/DL) devise a plan with your physician/cardiologist to get it down to a more favourable level.
25/ Yes there are other risk factors. Yes one should exercise, sleep well, avoid excessive alcohol consumption, avoid ultra-processed foods,
avoid smoking etc. None of this detracts from elevated ApoB being necessary to develop atherosclerosis.
avoid smoking etc. None of this detracts from elevated ApoB being necessary to develop atherosclerosis.
26/ Lastly, I’m often asked. Well what about the fact that even though my ApoB has increased I’ve lost weight and my blood glucose has improved with this diet?
27/ Based on today’s data all things equal you’re still at higher risk. And with a few diet modifications you can lower your ApoB & still achieve a healthy body weight & blood glucose control. You can even do this within a keto framework. It just becomes more plant-based.
28/ For an academic guideline paper that considers all of this I refer you to the 2021 ESC guidelines
academic.oup.com/eurheartj/arti…
academic.oup.com/eurheartj/arti…
29/ For an easier to digest dietary guideline paper that considers this I refer you to the 2021 AHA guidelines
ahajournals.org/doi/10.1161/CI…
ahajournals.org/doi/10.1161/CI…
30/ Thanks for reading. My interest in CVD stems back to watching my dad have a heart attack in front of me.
He’s a Professor of Physiology with 40 yrs experience researching how our arteries work.
Happy to expand on anything - I suspect there will be various questions.
He’s a Professor of Physiology with 40 yrs experience researching how our arteries work.
Happy to expand on anything - I suspect there will be various questions.
I should also note this comparable lipid lowering effect was between the Portfolio Diet and a LOW intensity statin. Not a high intensity statin.
*Addendum -this particular graph is total cholesterol not LDL-C. We would see the same discrepancies if we looked at LDL-C.
• • •
Missing some Tweet in this thread? You can try to
force a refresh



