Classic conundrum... PNA vs cardiogenic pulmonary edema
60 y/o no PMH presents with dyspnea, hypoxemia. SpO2 92% 6L NC HR 120 RR 30 BP 110/70. B/l crackles. No JVP or LE edema. Lactate 4.0. BNP 3x ULN (nco baseline). Tn 2xULN Procal 0.2. Pre-COVID.
How can we apply #POCUS
1/
60 y/o no PMH presents with dyspnea, hypoxemia. SpO2 92% 6L NC HR 120 RR 30 BP 110/70. B/l crackles. No JVP or LE edema. Lactate 4.0. BNP 3x ULN (nco baseline). Tn 2xULN Procal 0.2. Pre-COVID.
How can we apply #POCUS
1/

For the sake of argument, let's assume for this case
1) pre-test probability of PNA is 50%
2) pre-test probability of cardiogenic pulmonary edema is 50%
3) one or both of the above must be present to explain the presentation
2/
1) pre-test probability of PNA is 50%
2) pre-test probability of cardiogenic pulmonary edema is 50%
3) one or both of the above must be present to explain the presentation
2/
Importantly, it is not so simple as "B lines = CHF, consolidation = PNA"
Pneumonia can cause alveolar filling (which radiographically appears as consolidation) and/or interstitial thickening (which appears as B lines).
See our prior thread on this
3/
Pneumonia can cause alveolar filling (which radiographically appears as consolidation) and/or interstitial thickening (which appears as B lines).
See our prior thread on this
https://twitter.com/IMPOCUSFocus/status/1177700595509186560?s=20
3/
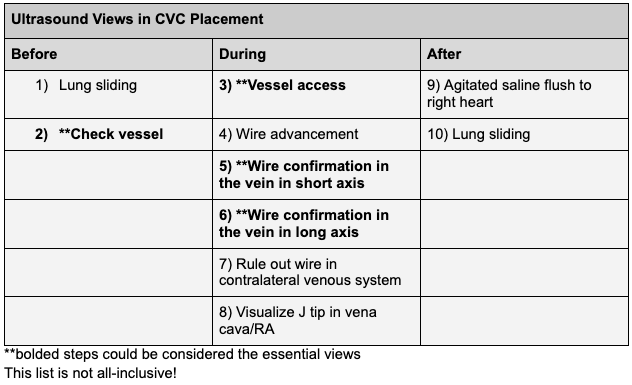
In theory, inflammatory cause of B lines is expected to be associated w inflammation of the pleura, as evidenced by pleural irregularity and small peripheral consolidations. And in theory, inflammatory cause is more likely to have "spared areas" of normal lung, seen as A lines.
Summarized here: features distinguishing B lines from cardiogenic pulmonary edema vs other causes
From: ccjm.org/content/88/6/3…
4/
From: ccjm.org/content/88/6/3…
4/
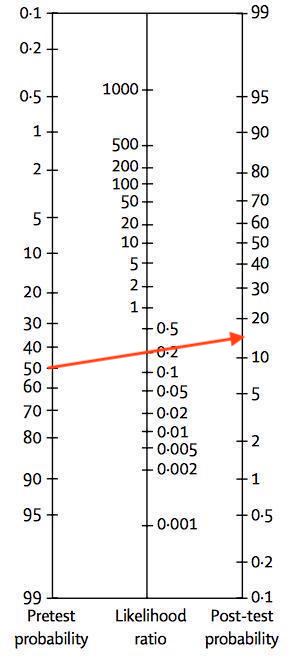
Additional resources on this include:
BLUE protocol (2008) includes a categorization of A/B, C, and B' for PNA: summary thread here
Table below from Copetti et al (2008) ncbi.nlm.nih.gov/pmc/articles/P…
5/
BLUE protocol (2008) includes a categorization of A/B, C, and B' for PNA: summary thread here
https://twitter.com/IMPOCUSFocus/status/1175013757120106496
Table below from Copetti et al (2008) ncbi.nlm.nih.gov/pmc/articles/P…
5/

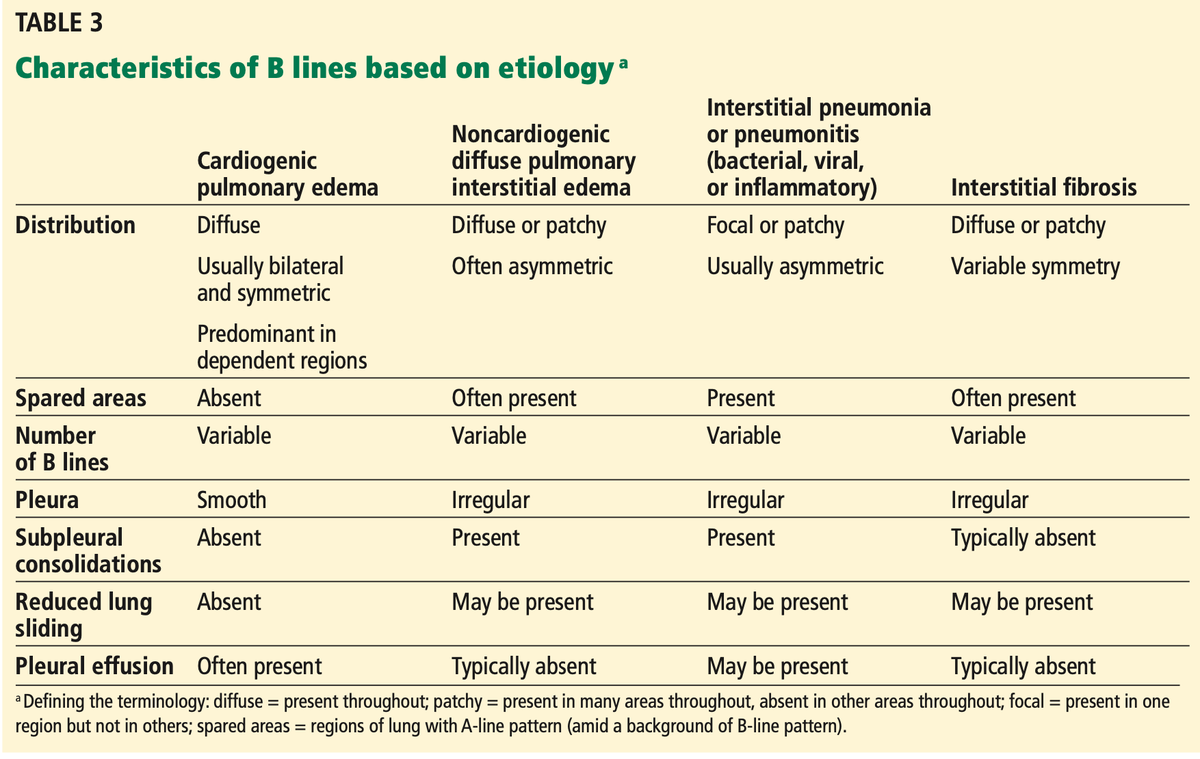
But, there is more to it when applying clinically. It always goes back to Bayesian reasoning, ie determining pre-test probability, applying #POCUS, and adjusting post-test prob.
Here is a table with "gestalt" clinical estimates of the effect of findings on post-test prob.
6/
Here is a table with "gestalt" clinical estimates of the effect of findings on post-test prob.
6/
We can do the same with cardiac findings (though trickier and less direct)
-L heart problem increases probability of elevated LAP and thus CPE
-R sided problem may weakly indirectly increase probability of CPE
-doesn't influence prob of PNA, other than providing alternative dx
7/
-L heart problem increases probability of elevated LAP and thus CPE
-R sided problem may weakly indirectly increase probability of CPE
-doesn't influence prob of PNA, other than providing alternative dx
7/

Back to the case. Lung images shown here
8/
8/
With just 1L here
9/
9/
We see B lines diffusely, with mostly regular pleura other than some hint of pleural irregularity in 3R but not much. And small bilateral pleural effusion. How does this influence post-test probability for cardiogenic pulmonary edema
10/
10/
How does this influence post-test probability for PNA?
11/
11/
Now cardiac images
(PSL, PSL w color, PSSPM, PSSMV)
12/
(PSL, PSL w color, PSSPM, PSSMV)
12/
More cardiac images
(A4c, A3c, SubX4c, IVC)
13/
(A4c, A3c, SubX4c, IVC)
13/
Moderately to severely reduced LV systolic function (new). Some suggestion of assymetric wall motion (won't go into more detail). IVC is < 2.0 cm with 100% collapse (though a short axis image would be a nice addition)
How does this affect prob of card. pulm edema
14/
How does this affect prob of card. pulm edema
14/
How do the cardiac images affect probability of PNA?
15/
15/
Thoughts on this at the time
Lung: favor card pulm edema (diffuse B lines and mostly regular pleura). Suggests against but doesn't exclude superimposed infection.
Cardiac: LV syst dysfunction increases prob of card pulm edema. Doesn't r/o PNA, but does provide alternative dx.
16/
Lung: favor card pulm edema (diffuse B lines and mostly regular pleura). Suggests against but doesn't exclude superimposed infection.
Cardiac: LV syst dysfunction increases prob of card pulm edema. Doesn't r/o PNA, but does provide alternative dx.
16/
It's worth mention of the IVC. Appearance suggested low RAP (as also evidenced by no LE edema or JVP elevation). RV also appeared normal. In this case, LV problem had not yet led to right sided failure.
Good thing we don't just give fluid for a collapsed IVC, right?
17/
Good thing we don't just give fluid for a collapsed IVC, right?
17/
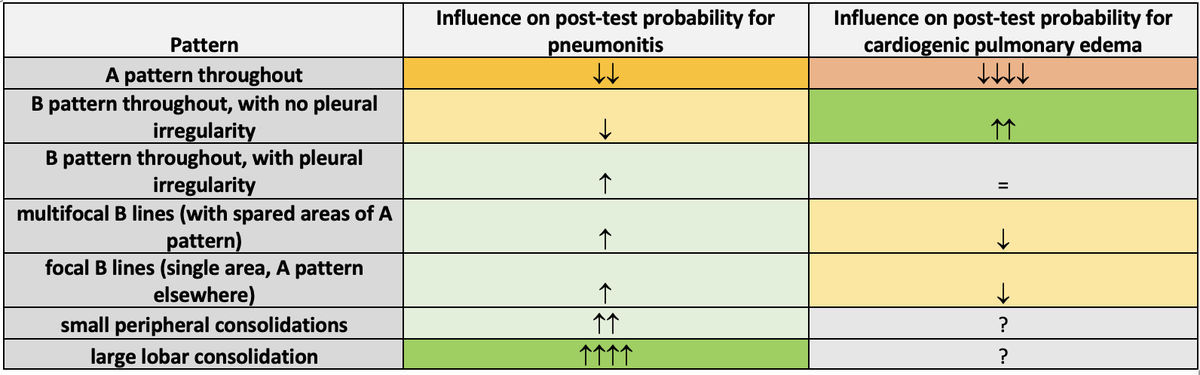
In summary, probability for cardiogenic pulmonary edema may have looked like this (before POCUS, LR+, after POCUS)
50% --> >95%
18/
50% --> >95%
18/

and for PNA (50% --> ~15%)
In this case, given the rest of the clinical picture, this was enough motivation to not use abx.
19/
In this case, given the rest of the clinical picture, this was enough motivation to not use abx.
19/
After POCUS, management immediately shifted focus to acute decompensated heart failure. And efforts to expedite cardiac workup increased.
20/
20/
W good clinical assessment, correct dx could be made w/o POCUS. But POCUS made dx easier, and can improve dx accuracy and expedite dx. Notably, findings here were relatively clear cut. Sometimes they are more subtle. Interested to hear thoughts from POCUS twitter!
21/
21/
@kyliebaker888 @iceman_ex @cameron_baston
@Manoj_Wickram @DRsonosRD @NephroP @ArgaizR @ria_dancel @hraza222 @ThinkingCC @Wilkinsonjonny
@katiewiskar @TaotePOCUS @easypocus @FioreSono @trobertson8 @IM_Crit_ @avinashaujayeb @Thind888 @KalagaraHari @udit_chaddha @icmteaching
@Manoj_Wickram @DRsonosRD @NephroP @ArgaizR @ria_dancel @hraza222 @ThinkingCC @Wilkinsonjonny
@katiewiskar @TaotePOCUS @easypocus @FioreSono @trobertson8 @IM_Crit_ @avinashaujayeb @Thind888 @KalagaraHari @udit_chaddha @icmteaching
• • •
Missing some Tweet in this thread? You can try to
force a refresh