
#IMPOCUS educational account sharing cases (fictionalized), ideas, EBM, and clinical integration. Not medical advice. Formerly PittIMPOCUS. #FOAMus.
2 subscribers
How to get URL link on X (Twitter) App



 For the sake of argument, let's assume for this case
For the sake of argument, let's assume for this case 

 2/
2/




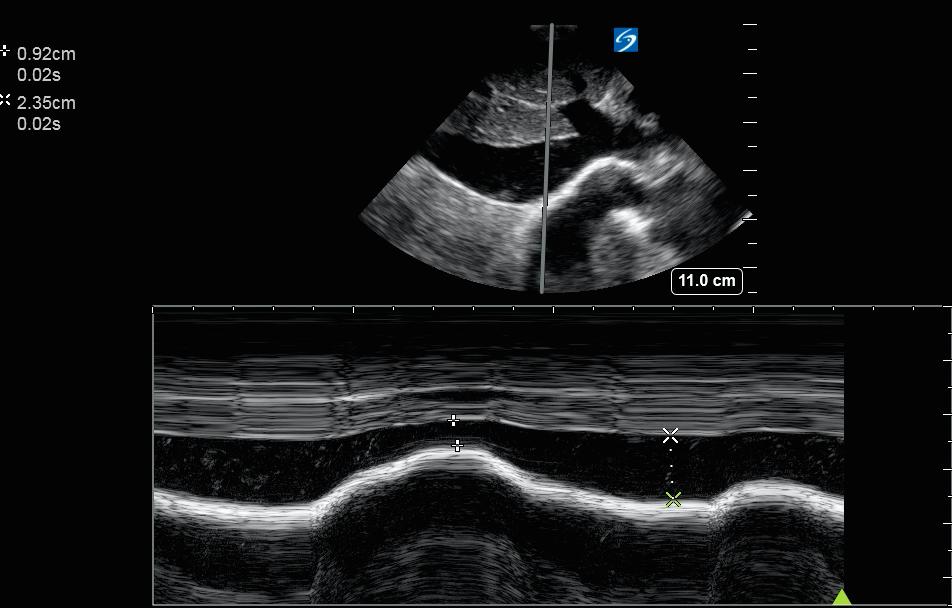
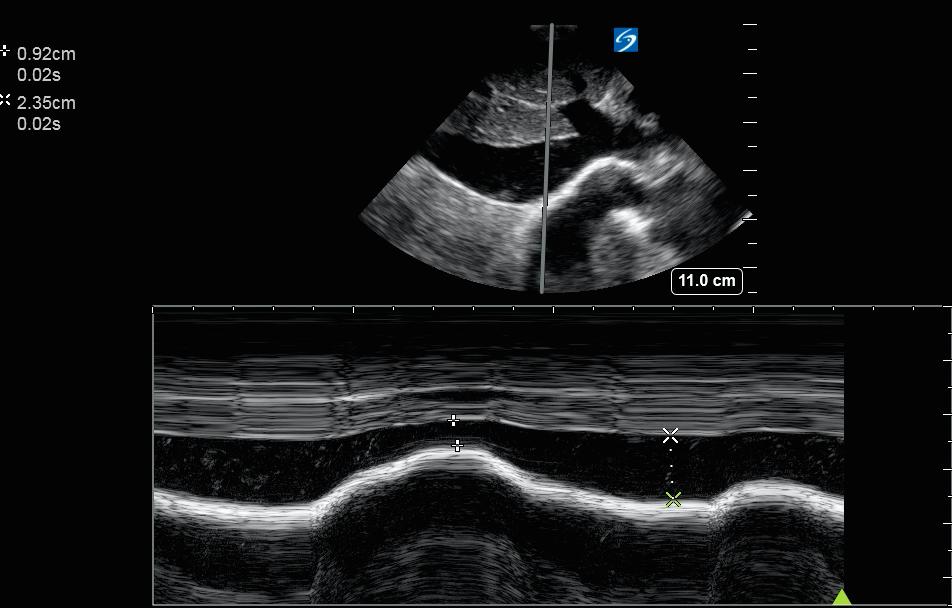
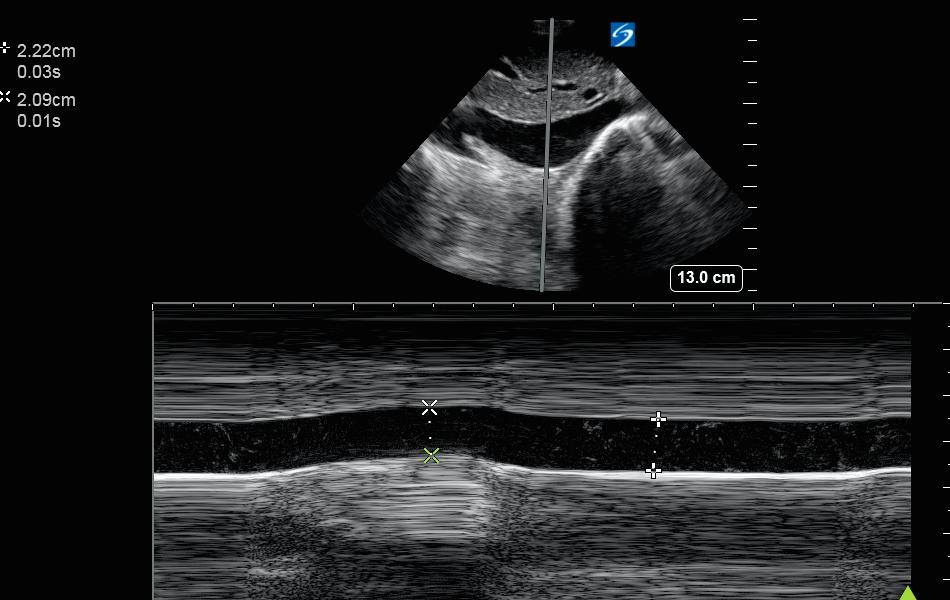 60 m with hx of COPD, HFpEF, admitted w LLL PNA s/p abx and 1 L LR. HR 118 BP 110/70. IVC US was performed as a piece of info in determining whether to administer more IVF.
60 m with hx of COPD, HFpEF, admitted w LLL PNA s/p abx and 1 L LR. HR 118 BP 110/70. IVC US was performed as a piece of info in determining whether to administer more IVF.

 2/Tagging POCUS friends/recent participants @SonoInternist @DRsonosRD @jelevenson @ria_dancel @msenussiMD @trobertson8 @G2Disrupt @IM_POCUS @buckeye_sanjay @benjikmathews @POCUS_Society @kyliebaker888 @CaseMcQuade @MedEdPGH @HeyDrNik @tweebui @UltrasoundJelly @5MinSono @awfujita
2/Tagging POCUS friends/recent participants @SonoInternist @DRsonosRD @jelevenson @ria_dancel @msenussiMD @trobertson8 @G2Disrupt @IM_POCUS @buckeye_sanjay @benjikmathews @POCUS_Society @kyliebaker888 @CaseMcQuade @MedEdPGH @HeyDrNik @tweebui @UltrasoundJelly @5MinSono @awfujita