
So recently I did a FOIA (Freedom of Information Act) request regarding CMS radiology (MRI) safety standards at outpatient imaging centers.
The results were disturbing...
The results were disturbing...
The 2008 MIPPA act sect. 135, (3) provides that the "Secretary [of HHS] shall establish procedures to ensure that the criteria used by an accreditation organization…"
...and "standards that require the supplier have procedures in place to ensure the safety of persons who furnish the technical component of advanced diagnostic imaging services and individuals to whom such services are furnished"
Said plainly, HHS Secretary (today, @secbacerra) is charged with establishing procedures for safety for advanced diagnostic imaging (ADI) modalities (CT, nucs, and MRI) reimbursed by CMS (Medicare / Medicaid), and setting safety standards for outpatient providers of ADI services.
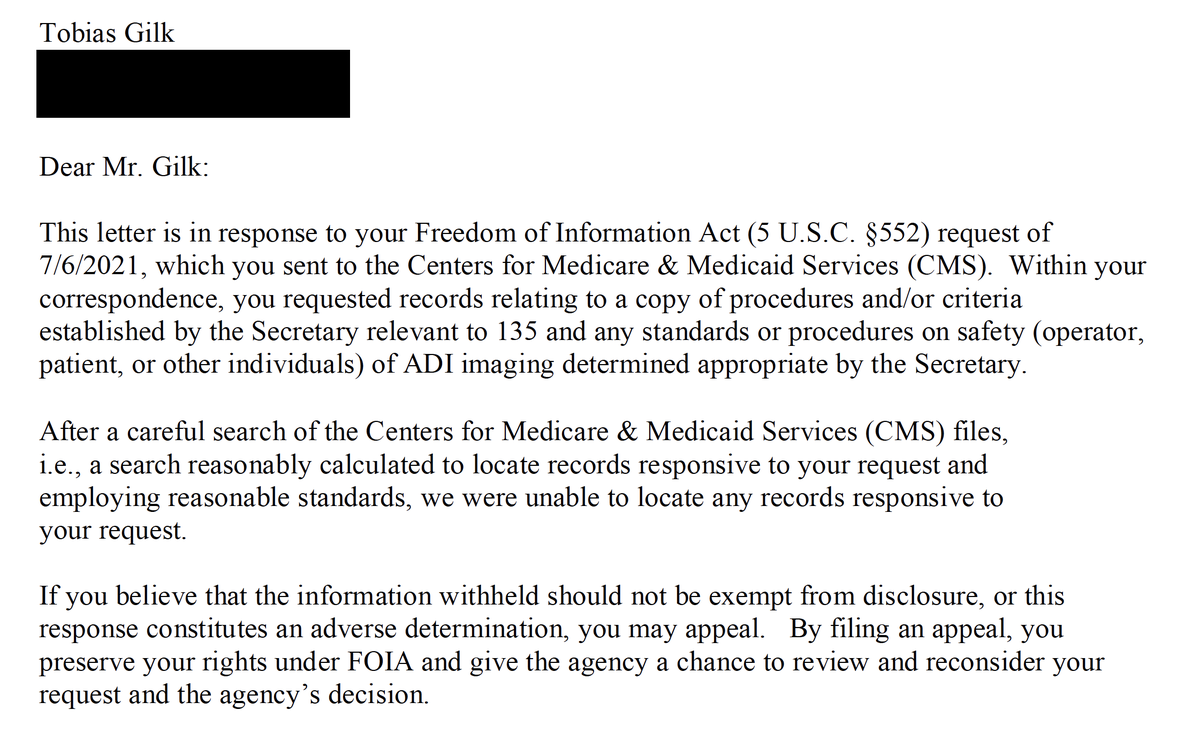
So this summer I submitted a FOIA request to CMS asking for those Secretary-established safety provisions. Very recently I received a response to my FOIA request...
"After a careful search of the Centers for Medicare & Medicaid Services (CMS) files, [snip], we were unable to locate any records responsive to your request." 
As I read this, despite that the MIPPA act *directs* the HHS Secretary ("shall", not "may") to establish minimum radiology safety criteria for providers and outpatient accrediting orgs, the HHS Secretary has *not* established any minimum safety criteria for ADI providers.
Specifically for #MRI (since we all know that's my particular interest), this means that the Secretary of HHS has no minimum #MRIsafety training or qualification requirements under MIPPA. No physical safety minimums (e.g., zones or 5 Gauss containment).
This is unsettling because on the *hospital* side, there are specific radiology safety "conditions of participation" that all hospital providers must meet.
Does @HHSGov / @CMSGov think that the radiation from a CT scanner is benign just because it's in an outpatient imaging center, whereas those hospital CT's are the only ones that produce dangerous radiation? Are O2 tanks less likely to fly at an outpatient-located MRI?
Are CMS beneficiaries who obtain ADI services from an outpatient imaging center less worthy of safety provisions or protections than the beneficiaries who get their services from a hospital?
I implore @HHSGov and @secbacerra / @xavierbecerra
to meet the obligation of the Secretary under 2008 MIPPA and establish ADI radiology provider and accreditation organization minimum safety standards as has been done for hospital providers / accrediting bodies.
to meet the obligation of the Secretary under 2008 MIPPA and establish ADI radiology provider and accreditation organization minimum safety standards as has been done for hospital providers / accrediting bodies.
Please unroll this @threadreaderapp
Pardon my twitter-handle typo... @SecBecerra
• • •
Missing some Tweet in this thread? You can try to
force a refresh





