1/ Would you want your employees, your customers, your partners, and government regulators to hear what you tell investors?
It's not done! Different audiences will understand and react to the same thing very differently
I'm going to take that risk today, show you my deck 😱🙏
It's not done! Different audiences will understand and react to the same thing very differently
I'm going to take that risk today, show you my deck 😱🙏

2/ I'm going to walk through what I presented and said yesterday at the big healthcare investor meeting #JPMHC22
In a normal year, to hear the coveted private company presentations you'd have to be there, investors and executives crammed into small rooms
camera crews outside
In a normal year, to hear the coveted private company presentations you'd have to be there, investors and executives crammed into small rooms
camera crews outside

3/ What's the problem we're solving?
In the US, we wait until someone has a stroke or heart attack, and will then spare no expense
But we control blood pressure 63% of the time
All the "action" is at the bottom of the waterfall
That's a trillion dollars a year of suffering
In the US, we wait until someone has a stroke or heart attack, and will then spare no expense
But we control blood pressure 63% of the time
All the "action" is at the bottom of the waterfall
That's a trillion dollars a year of suffering

4/ As a public health person, this is not just a financial problem, it's a moral catastrophe
When I was @nycHealthy, @DrTomFrieden asked "How can healthcare save the most lives?"
We couldn't even find an attempt to answer the freaking question in the literature-we did the study

When I was @nycHealthy, @DrTomFrieden asked "How can healthcare save the most lives?"
We couldn't even find an attempt to answer the freaking question in the literature-we did the study


5/ Why?
In 2008, we thought that there were 3 problems that had to be solved simultaneously- payment that rewards prevention, information systems oriented to prevention, and practice workflows.
I spent over 10 years focused on the last 2 (reader, it didn't work)

In 2008, we thought that there were 3 problems that had to be solved simultaneously- payment that rewards prevention, information systems oriented to prevention, and practice workflows.
I spent over 10 years focused on the last 2 (reader, it didn't work)


6/ w co-founder @matkendall (& now @ONC_HealthIT Dir. @mickytripathi1) we homed in on moving doctors from paper to electronic health records, adding population health into those (document/billing) systems, and on the hand-on support they would need to convert practice workflows 



7/ It didn't work
During my time at @ONC_HealthIT EHR adoption skyrocketed, but blood pressure control didn't budge.
Hearing this @POLITICOPulse podcast recorded w @ddiamond after I left government, I'm struck by how disillusioned I sound.
politico.com/story/2016/05/…
During my time at @ONC_HealthIT EHR adoption skyrocketed, but blood pressure control didn't budge.
Hearing this @POLITICOPulse podcast recorded w @ddiamond after I left government, I'm struck by how disillusioned I sound.
politico.com/story/2016/05/…
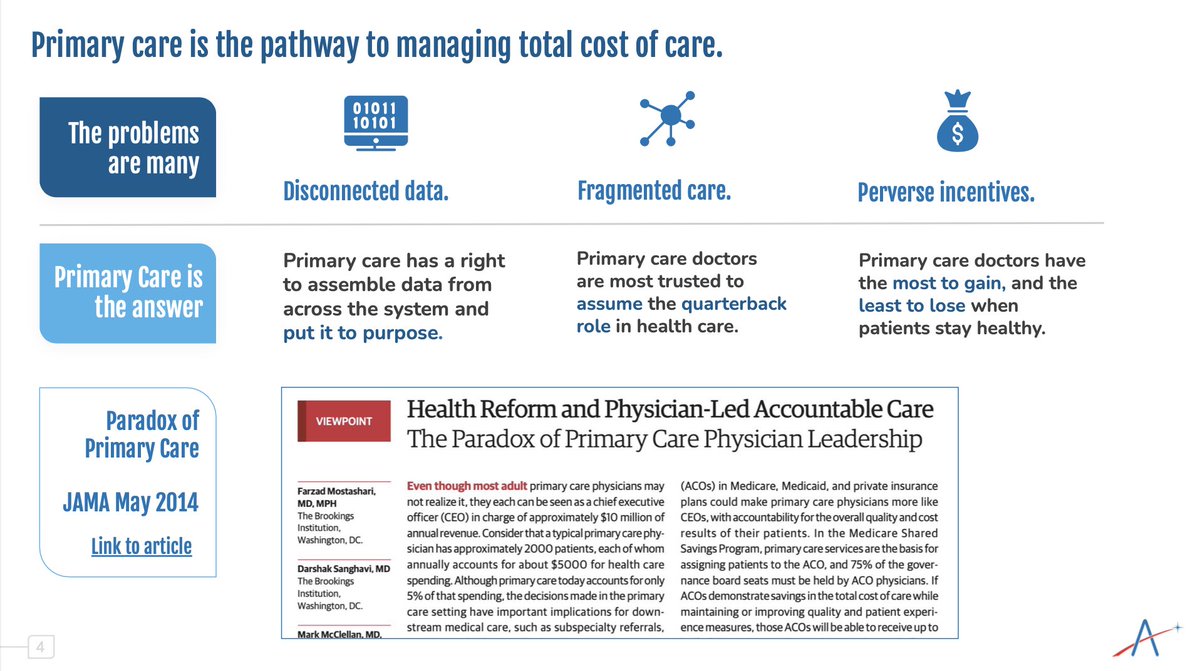
8/ I was looking for some window in American healthcare where preventing a stroke would be more profitable than treating it.
"Accountable Care Organizations" could be it, but I was convinced that physician-led ACOs-and primary care-were the answer, not hospitals & health systems
"Accountable Care Organizations" could be it, but I was convinced that physician-led ACOs-and primary care-were the answer, not hospitals & health systems
9/ 10 yrs later, it is now, ironically, conventional wisdom that " "Risk-taking primary care" and "Physician Enablement" are a once-a-generation business opportunity.
We have many "fellow travelers" in this space (FFS is the competition) but we have carved a particular path
We have many "fellow travelers" in this space (FFS is the competition) but we have carved a particular path

10/ Each of these strategic decisions were made deliberately, to maximize the societal reach and scale we could have
Each connects to the others
We would serve exiting practices, with as much of their panel as possible, and stay true to our north star
Not focusing on MA was 🗝️
Each connects to the others
We would serve exiting practices, with as much of their panel as possible, and stay true to our north star
Not focusing on MA was 🗝️
11/ I learned from @Venrock @BRobertsVC that the power behind @AledadeACO is the creation of incentive alignment
We all prosper if costs go down, the right way.
That's it. That's all of it.
We don't try to make money through (zero-sum) FFS negotiations b/w plans and practices
We all prosper if costs go down, the right way.
That's it. That's all of it.
We don't try to make money through (zero-sum) FFS negotiations b/w plans and practices

12/ And to make it easy for practices to join us, we wouldn't charge them (or payers) for technology or coaching or contracts or capital reserves
We aren't "vendors" we're partners
We give them what they need at scale, which means outstanding economics for them (and for payers)
We aren't "vendors" we're partners
We give them what they need at scale, which means outstanding economics for them (and for payers)

13/ Shedding value means that you make the flywheel spin faster
We also have an awesome virtuous cycle at play:
The more practices we have the easier to get global risk contracts w plans (you need minimum size)
The more contracts, the easier to sign practices
Around🔄Around
We also have an awesome virtuous cycle at play:
The more practices we have the easier to get global risk contracts w plans (you need minimum size)
The more contracts, the easier to sign practices
Around🔄Around

14/ When I was just starting Aledade, I used to do a parlor trick.
"Assume you can get 100 primary care docs together
..and they each care for 2,000 patients
...and each patient accounts for $5,000 a year in medical costs
How much spend do they influence?"
(math)
"Assume you can get 100 primary care docs together
..and they each care for 2,000 patients
...and each patient accounts for $5,000 a year in medical costs
How much spend do they influence?"
(math)
15/ that's right (even if it seems like a crazy number of zeros)
100 PCPs can be a billion dollar business.
If they actually believe that they can manage the total cost and quality of care for their patients
PCPs have been neglected for so long, making that mental leap is hard
100 PCPs can be a billion dollar business.
If they actually believe that they can manage the total cost and quality of care for their patients
PCPs have been neglected for so long, making that mental leap is hard

16/ But HOW??
It can seem overwhelming, so we shrink it down to what every PCP can agree is just good primary care.
All the results we've accomplished have been based on these Core4™️ advanced primary care practice competencies.
(and yes, we're incubating several Core More)
It can seem overwhelming, so we shrink it down to what every PCP can agree is just good primary care.
All the results we've accomplished have been based on these Core4™️ advanced primary care practice competencies.
(and yes, we're incubating several Core More)

17/ And yes, building cloud-based software that can be the Operating System for practices' population health work has been key to making these competencies scale
Each data source adds unique value
Actionable Insights >> Data
Workflow is everything
Outcomes are what matters
Each data source adds unique value
Actionable Insights >> Data
Workflow is everything
Outcomes are what matters

18/ We are the best engine for accumulating "the opportunity to make a difference" (lives under management) but where we are truly differentiated is in supporting practice behavior change, even (especially) if they don't work for us.
The science and art of aligning 💙,🧠, and🛣️
The science and art of aligning 💙,🧠, and🛣️

19/ We launched 100 practices across 5 very different states in 2016- our "reference cohort"
Year after year, they have widened the gap between themselves and their peers in outcomes that matter
More primary care visits
👉 fewer ER visits
👉 fewer hospital admits
👉 lower cost
Year after year, they have widened the gap between themselves and their peers in outcomes that matter
More primary care visits
👉 fewer ER visits
👉 fewer hospital admits
👉 lower cost

20/ The Medicare Shared Savings Program has been the most transparent value-based program, saving billions of dollars, even if (excluding Aledade) average savings have been ~2% of total cost of care vs benchmark
Aledade practice cohorts keep getting better, faster 📈
Aledade practice cohorts keep getting better, faster 📈

21/ This is how the money works for a mature cohort
We have a budget (benchmark), say $1.5B
Claim payments are deducted
Whats left (10%=$150M) is value we've created
The plan keeps $45M
Our practice partner get $53M
After paying for direct costs ~$47M "platform contribution"
We have a budget (benchmark), say $1.5B
Claim payments are deducted
Whats left (10%=$150M) is value we've created
The plan keeps $45M
Our practice partner get $53M
After paying for direct costs ~$47M "platform contribution"

22/ That gross margin goes towards the cost of practice outreach, and building our technology and data platform, plus the regulatory, and legal and finance and all the other overhead expenses.
For years, that was paid for by our investors. But we're now profitable.. and growing
For years, that was paid for by our investors. But we're now profitable.. and growing

23/ We can now invest more and more into the most important part of our mission- improving care, reducing suffering, and reducing costs.
Which brings us to the big news yesterday... our acquisition of an amazing company- Iris Healthcare
A perfect mission and culture fit
Which brings us to the big news yesterday... our acquisition of an amazing company- Iris Healthcare
A perfect mission and culture fit

24/ We worked with them for over 3 years to provide comprehensive advance care planning for the most complex patients in our practices.
They spent hours with patients and their families, explored very difficult scenarios, documented, and followed up
The results were terrific 👇
They spent hours with patients and their families, explored very difficult scenarios, documented, and followed up
The results were terrific 👇

25/ There may be more opportunities like Iris
There are many terrific "point solutions" that tackle a thorny problem well but face challenges in targeting the right patients, engaging them, and getting paid for the value they create, in fee for service, #BetterTogether w Aledade
There are many terrific "point solutions" that tackle a thorny problem well but face challenges in targeting the right patients, engaging them, and getting paid for the value they create, in fee for service, #BetterTogether w Aledade

26/ It's not often that you find the intersection of
a really huge problem
a disruptive wave that scrambles the status quo
a "product" that really works- at scale
a platform that can be built on
and an incredible team that will not quit.
That defines an "interesting company"
a really huge problem
a disruptive wave that scrambles the status quo
a "product" that really works- at scale
a platform that can be built on
and an incredible team that will not quit.
That defines an "interesting company"

27/ I am so grateful for 2 things:
An alignment between business and mission that makes it possible for our company to speak with the same authentic voice to our practices, business partners, policymakers, employees, and investors.
The incredible team at @AledadeACO (join us!)
An alignment between business and mission that makes it possible for our company to speak with the same authentic voice to our practices, business partners, policymakers, employees, and investors.
The incredible team at @AledadeACO (join us!)

• • •
Missing some Tweet in this thread? You can try to
force a refresh