New: Preliminary findings related to the severity and impact of the surge of #COVID19 cases associated with the introduction of the #omicron variant to NYC: on.nyc.gov/3zTIDYk
Some key findings 🧵⬇
Some key findings 🧵⬇
Omicron quickly became the most prevalent variant and led to a dramatic increase in reported cases. Whereas the delta variant became the dominant variant (from 0% prevalence to more than 90% prevalence) over a period of 20 weeks, omicron became the dominant variant in five weeks. 

When the omicron variant emerged in NYC, it led to a steep rise in the number of people who visited emergency departments with COVID-like illness. Shortly afterward, the daily number of hospitalizations increased too. 

Overall, a smaller proportion of patients diagnosed with COVID-19 since the omicron variant emerged in NYC have been hospitalized, but the total number of hospitalizations increased because of the very large number of reported cases. 

A similar pattern was also seen in Gauteng, South Africa, where approximately 5% of COVID-19 cases were hospitalized during the most recent wave associated with omicron, compared to 19% and 47% during the prior two waves in the region.
Rates of hospitalization have been dramatically higher among the unvaccinated. At the time of this report, over 73% of all New York City residents were fully vaccinated. 

The proportion of hospitalizations have been higher among older adults and Black/African American New Yorkers. 

Emergency department visits for COVID-like illness have gotten less severe compared to previous waves. The emergency severity index is a rating with scale from 1 (most urgent) to 5 (least urgent). 

The number of hospitalized patients increased dramatically due to omicron’s prevalence. As of Dec. 30, 2021, hospitalizations exceeded last winter’s surge and the number of patients in the ICU is approaching what was seen last winter. 

About half of all patients in NYC hospitals have COVID-19. Despite stable total numbers of hospitalized patients, staffing shortages have been felt widely during the omicron wave across the health care sector in NYC. Nearly all hospitals report some impact on operations. 

The number of COVID-19 patients in the ICU in NYC hospitals increased steadily as the number of cases rose. However, the proportion of patients in the ICU remains lower than in previous waves. Percentage-wise, fewer New Yorkers are in the ICU or require ventilator support. 

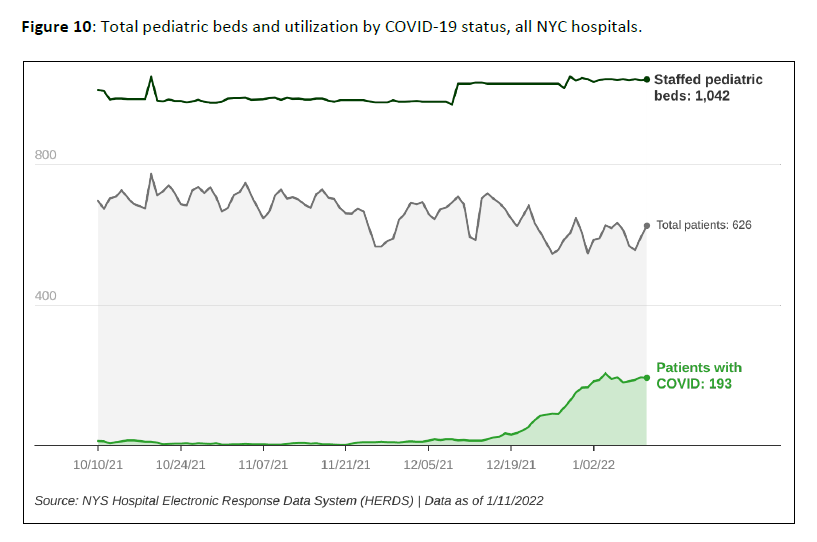
Total pediatric hospital census was stable to slightly lower during the omicron wave, though pediatric hospitalizations due to or with COVID-19 increased significantly. And unvaccinated kids 5-17 years old were over 4 times more likely to be hospitalized compared with all kids. 
Remember, there are things all New Yorkers can do to beat back omicron:
✅ Get vaccinated and get boosted
✅ Wear a high-quality mask
✅ Get tested
✅ Meet outdoors
✅ Avoid optional activities if at risk for severe illness
✅ Get vaccinated and get boosted
✅ Wear a high-quality mask
✅ Get tested
✅ Meet outdoors
✅ Avoid optional activities if at risk for severe illness
https://twitter.com/NYCHealthCommr/status/1476193033917849602
• • •
Missing some Tweet in this thread? You can try to
force a refresh






