1/ Why automated quality metrics may be the key to unlocking adoption of new polyp detection technologies for #colorectalcancer screening, a brief 🧵 
2/ A common refrain is that cost barriers have been the central reason for slow uptake of evidence-based polyp detection technologies (mucosal exposure caps, wide angle colo, & perhaps #AI). 




3/ I think that's not the whole story. This pattern also exposes the near absence of user-friendly, automated endoscopy quality analytics tools.
4/ Presently, when a GI team trials a polyp detection technology, in most cases the final purchase decision comes down to only two things: A) a 'back of the envelope' economic analysis and B) the 'gut' feeling of users after a few month trial re: whether the tech 'felt' helpful.
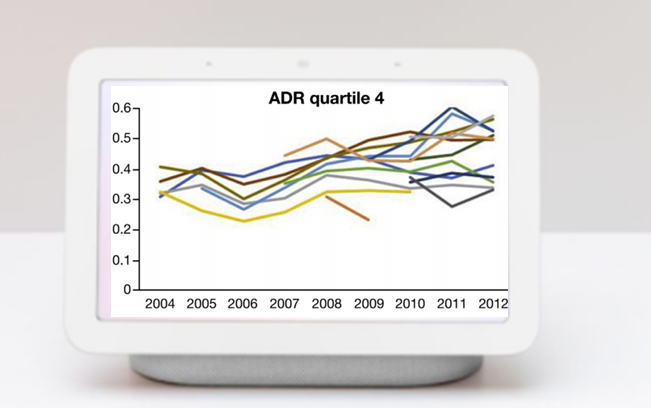
5/ This is not how critical decisions regarding quality improvement initiatives should be made and exposes a fundamental flaw and *key technology gap* in GI practice. For majority of U.S. GI groups, it's not yet possible to get automated, button-click analytics re: ADR and APC.
6/ Imagine running a sports team without live data re: athlete performance, & no way to tell from game to game whether strategic changes had altered player or team stats. NFL, NBA etc all already use cloud-based AI to generate a vast range of simple and complex performance data. 



7/ Most GI groups are stuck where sports were in the 1960s, with no *live* access to analytics. Data is often stuck in outdated EHRs and/or siloed between path, hospital, endo center etc. 

8/ @GoogleHealth and others have tried to begin chipping away at this data silo issue. Several rockstar GI colleagues across U.S. medical centers have solved these issues locally, often using #NLP as a tool, but the solutions have not yet been scalable.
9/ The 'dawn of AI' for GI can't really happen without the dawn of automated analytics. If we *can* solve this in a scalable way for gastroenterology, analytics tools will be rocket fuel for an unapparelled wave of innovation. 

• • •
Missing some Tweet in this thread? You can try to
force a refresh