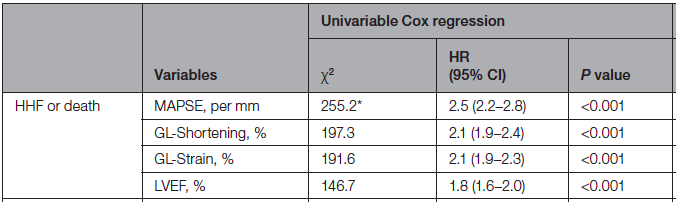
Do you routinely measure #MAPSE?
Did you know that MAPSE beats #GLS and #LVEF regarding prognosis?
A new multicenter collab study out, led by @KellmanPeter
Ref:
#WhyCMR 🫀🧲 #EchoFirst 🫀🔊
A thread 🧵. 1/n pubmed.gov/35132872

Did you know that MAPSE beats #GLS and #LVEF regarding prognosis?
A new multicenter collab study out, led by @KellmanPeter
Ref:
#WhyCMR 🫀🧲 #EchoFirst 🫀🔊
A thread 🧵. 1/n pubmed.gov/35132872

We know that GLS is a composite measure correlated w LVEF, LVEDV, LVESV, LV mass, infarction, non-ischemic scar, aortic stenosis, mitral regurg, ECV.
So, not surprisingly, GLS associates with poor prognosis.
Ref: Suppl Table 2
2/n pubmed.gov/32563637
So, not surprisingly, GLS associates with poor prognosis.
Ref: Suppl Table 2
2/n pubmed.gov/32563637
Notably, mitral annular plane systolic excursion #MAPSE has been measurable by #EchoFirst since 1986 by M-mode ().
3/n pubmed.gov/3464160

3/n pubmed.gov/3464160

#MAPSE (aka atrioventricular [AV] plane displacement) healthy normal values by #EchoFirst M-mode have been known since 1988 to be 🧓👴age-dependent with values around 16 mm ().
4/n pubmed.gov/3207068

4/n pubmed.gov/3207068

More recently (2019), similar findings were found using automated measurements of #MAPSE by anatomical M-mode (retrospective measurement from 2D images = no need for dedicated M-mode acquisition).
5/n pubmed.gov/31544286


5/n pubmed.gov/31544286


#MAPSE has been indexed to the length of the 🫀LV (MAPSE/LV length, called long-axis strain or global longitudinal shortening), and this has been shown to be prognostically equivalent to GLS and better than LVEF after infarction.
6/n pubmed.gov/31329854

6/n pubmed.gov/31329854

So, in our study we put an in-line AI automatic #WhyCMR MAPSE head-to-head against GLS, global longitudinal shortening, & LVEF for prognosis.
✅MAPSE wins🏆 out every time, whether for death💀, hospitalization🏥 for HF, or both.
7/n pubmed.gov/35132872

✅MAPSE wins🏆 out every time, whether for death💀, hospitalization🏥 for HF, or both.
7/n pubmed.gov/35132872
A convenient bonus/feature is that the AI MAPSE was more reproducible than manual🖐️experts, and measurements automatically pop up on the 🧲scanner at the time of #WhyCMR scanning near-instantaneously.
8/n


8/n

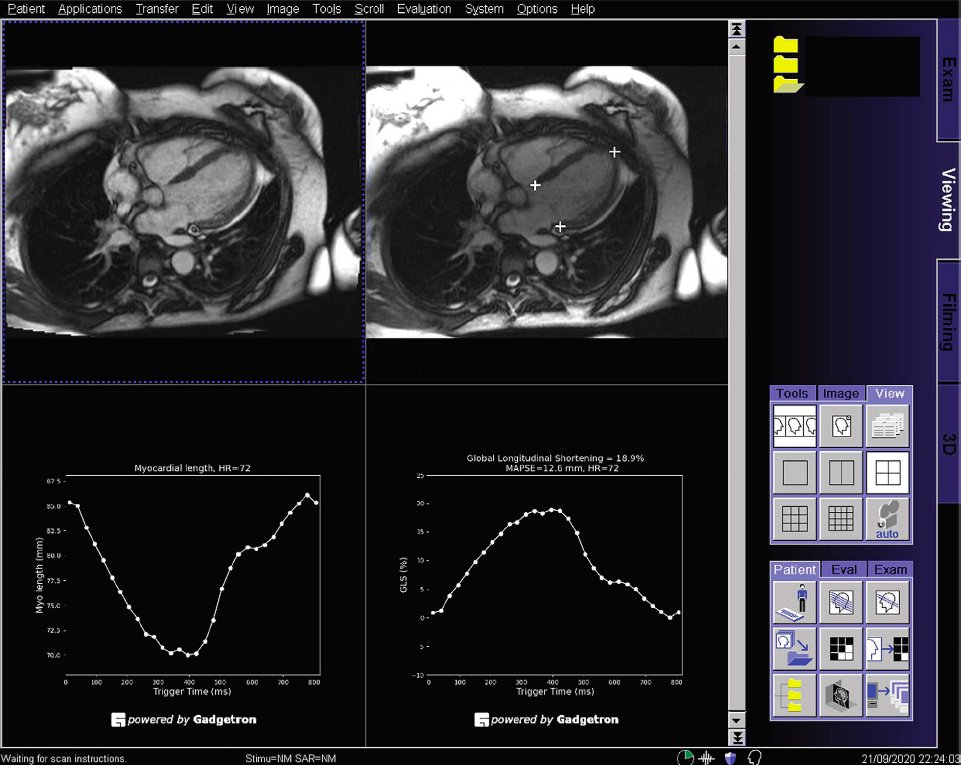
So, we're integrating MAPSE into our clinical #WhyCMR reports, because, the data tells us it's A Good Thing.
9/n
9/n
But more importantly, MAPSE by #EchoFirst and #WhyCMR have been shown to effectively give the same results.
10/n pubmed.gov/33550709

10/n pubmed.gov/33550709

So, since you can almost always measure MAPSE despite not seeing large swaths of the LV by #EchoFirst, imho MAPSE deserves some renewed attention in the #EchoFirst space, and has a justified place in the clinical echo report📩.
11/11gfycat.com/amplerealistic…
11/11gfycat.com/amplerealistic…
Thank you @StefanoNistri for pointing this out. GLS (and presumably MAPSE) can certainly be measured using dynamic CCTA 🫀⏺️ as well.
@JoaoLCavalcantepubmed.gov/34791101
@JoaoLCavalcantepubmed.gov/34791101
And MAPSE has even been estimated by gated planar 201-Tl scintigraphy 🫀☢️ back in 1986.
pubmed.gov/3464160


pubmed.gov/3464160


• • •
Missing some Tweet in this thread? You can try to
force a refresh












