Summary of oxygen delivery devices taught to me by Mayo RT
Source of oxygen
- Wall taps by bedside: 0–15L/min
- Home concentrator: 0–10L/min
Oxygen delivered at 100%, put through different devices at different rates to adjust the oxygen concentration that the patient inspires
Source of oxygen
- Wall taps by bedside: 0–15L/min
- Home concentrator: 0–10L/min
Oxygen delivered at 100%, put through different devices at different rates to adjust the oxygen concentration that the patient inspires
TLDR
- Low oxygen (<35%): nasal prongs
- Moderate oxygen (35-60%): venturi (high flow but mix with room air)
- High oxygen (>60%): non rebreather or HFNC
- PEEP needed (e.g., ADCHF, OSA): CPAP
- Hypercapnic: BiPAP
- Failure, unable to protect airway: mechanical ventilation
- Low oxygen (<35%): nasal prongs
- Moderate oxygen (35-60%): venturi (high flow but mix with room air)
- High oxygen (>60%): non rebreather or HFNC
- PEEP needed (e.g., ADCHF, OSA): CPAP
- Hypercapnic: BiPAP
- Failure, unable to protect airway: mechanical ventilation

0. Inogen (pulse-dose oxygen therapy); not used in hospital
- Delivers only during inspiration; not expiration
- Up to 4L but intermittent; much less oxygen as unlike continuous oxygen therapy which fills the oral cavity, naso/oropharyngeal with reservoir of oxygen, this does not
- Delivers only during inspiration; not expiration
- Up to 4L but intermittent; much less oxygen as unlike continuous oxygen therapy which fills the oral cavity, naso/oropharyngeal with reservoir of oxygen, this does not

1. Nasal cannula
* Deliver 24-45% oxygen; not precise (approx 4% per liter O2)
* Flow rate 1-6L/min (> 4L dry nose; uncomfortable)
* Used in non-acute situations or if only mildly hypoxic (e.g. saturations stable at 92% in a patient without lung disease)
* Deliver 24-45% oxygen; not precise (approx 4% per liter O2)
* Flow rate 1-6L/min (> 4L dry nose; uncomfortable)
* Used in non-acute situations or if only mildly hypoxic (e.g. saturations stable at 92% in a patient without lung disease)
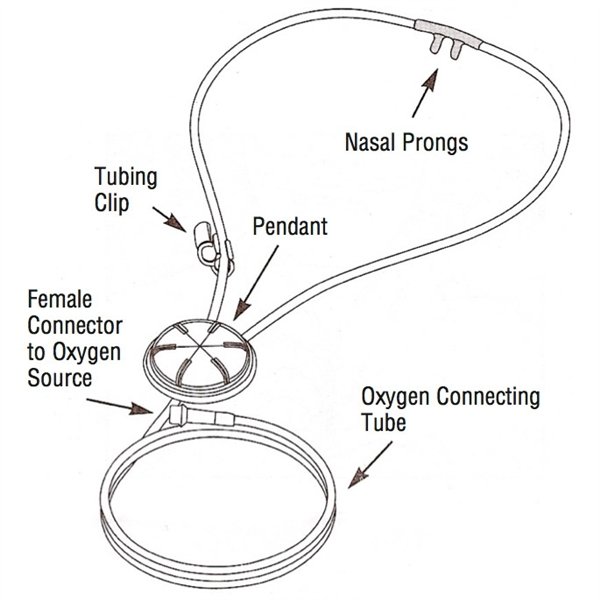
3a. Nasal pendant
- 2-15L/min
- FiO2 not precise
- Used if oxygen goals are not met by nasal cannula at <6 L/min
- 2-15L/min
- FiO2 not precise
- Used if oxygen goals are not met by nasal cannula at <6 L/min
3b. Simple facemask
- 5-15L (at least 5L to get rid of carbon dioxide)
- FiO2: depends on mask fit, minute ventilation, and flow
- Used if oxygen goals are not met by nasal cannula at <6 L/min
- 5-15L (at least 5L to get rid of carbon dioxide)
- FiO2: depends on mask fit, minute ventilation, and flow
- Used if oxygen goals are not met by nasal cannula at <6 L/min
3c. Venturi facemask
- Unlike simple and non-rebreather facemasks where you set the oxygen flow rate, you set FiO2 here (24%-60%)
- BLUE = 2-4L/min = 24% O2
- WHITE = 4-6L/min = 28% O2
- YELLOW = 8-10L/min = 35% O2
- RED = 10-12L/min = 40% O2
- GREEN = 12-15L/min = 60% O2
- Unlike simple and non-rebreather facemasks where you set the oxygen flow rate, you set FiO2 here (24%-60%)
- BLUE = 2-4L/min = 24% O2
- WHITE = 4-6L/min = 28% O2
- YELLOW = 8-10L/min = 35% O2
- RED = 10-12L/min = 40% O2
- GREEN = 12-15L/min = 60% O2

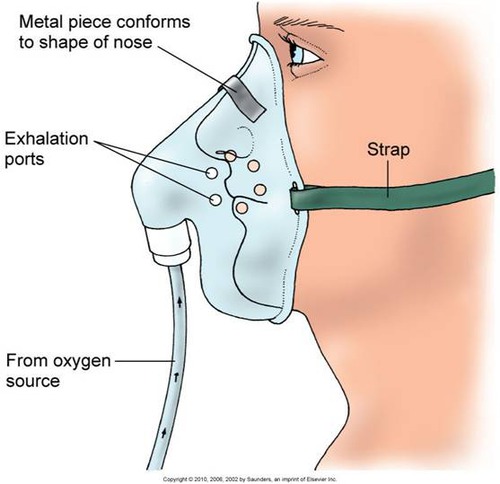
4. Nonrebreather
- Delivers 60-90% FiO2
- 10–15L flow rate (< 10L, CO2 retention)
- BAG MUST BE INFLATED or suffocate!!
- Severe hypoxemia: can place nonrebreather over nasal cannula
- Delivers 60-90% FiO2
- 10–15L flow rate (< 10L, CO2 retention)
- BAG MUST BE INFLATED or suffocate!!
- Severe hypoxemia: can place nonrebreather over nasal cannula

5. HFNC
- Max 60-80L/min flow rate
- Up to 100% oxygen
- Humidifier and warmth (comfort)
- 3–5 PEEP depending on flow
- Start
- 50 L/min
- Titrate FiO2 for sats
- Titrate down flow rate for comfort
- Max 60-80L/min flow rate
- Up to 100% oxygen
- Humidifier and warmth (comfort)
- 3–5 PEEP depending on flow
- Start
- 50 L/min
- Titrate FiO2 for sats
- Titrate down flow rate for comfort

6. NIPPV
- CPAP: keep airways open for oxygenation
- BiPAP: provides an inspiratory pressure (e.g., 12) and expiratory pressure (e.g., 5). EPAP = PEEP for oxygenation. Difference between IPAP - EPAP (ΔP) determines TV for ventilation (↑ΔP, ↑TV)
- AVAPS: set targeted TV
- CPAP: keep airways open for oxygenation
- BiPAP: provides an inspiratory pressure (e.g., 12) and expiratory pressure (e.g., 5). EPAP = PEEP for oxygenation. Difference between IPAP - EPAP (ΔP) determines TV for ventilation (↑ΔP, ↑TV)
- AVAPS: set targeted TV

7. Intubation
Indications
- Inadequate ventilation
- Refractory hypoxemia
- Inability to protect airway
AC/VC initial
1. TV: 4-6 mL/kg
2. PEEP: 5–8 (or PV tool)
3. FiO2 100% —> < 60%
4. RR 12-20
Pressures
- Driving < 15
- Peak < 40
- Plateau < 30
Indications
- Inadequate ventilation
- Refractory hypoxemia
- Inability to protect airway
AC/VC initial
1. TV: 4-6 mL/kg
2. PEEP: 5–8 (or PV tool)
3. FiO2 100% —> < 60%
4. RR 12-20
Pressures
- Driving < 15
- Peak < 40
- Plateau < 30

@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh