
New data from @nychealthy on racial inequities during the omicron wave in NYC explores why dramatic inequities experienced by Black New Yorkers throughout the pandemic became worse during the most recent surge: on.nyc.gov/3C7PUVu
Key analyses and ACTIONS🧵⬇️
Key analyses and ACTIONS🧵⬇️
Structural racism is a key driver of health inequity. We use the framework of a “COVID-19 prevention cascade” to map out factors rooted in anti-Black racism and provide a roadmap for achieving racial equity in #COVID19 outcomes, for NYC and beyond. @nychealthcmo 

Since the start of the pandemic, Black & Latino New Yorkers and those in high-poverty neighborhoods have been less able to work from home. This led to increased COVID-19 exposure among these groups, though it does not fully explain the worsening inequities seen during omicron. 

Despite overall narrowing in racial vaccination gaps, we observed delays in primary series vaccination among Black New Yorkers and lower rates of booster doses among eligible Black New Yorkers by winter 2021 when the omicron surge began. 



We also observed longer delays to diagnosis among Black New Yorkers and residents of the least privileged census tracts, even before the omicron surge. This is driven in part by structural barriers such as decreased access to COVID-19 testing or time off work to seek testing. 

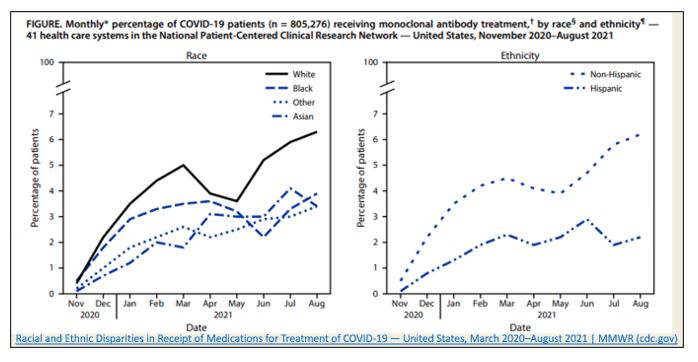
Inequities in access to outpatient COVID-19 treatment led to missed opportunities to prevent severe COVID-19 infection and hospitalization. Before omicron, national data showed that Black Americans were less likely than White Americans to receive monoclonal antibodies. @CDCMMWR 
These findings were a key reason that @nychealthy launched same-day, free home delivery of new oral antivirals, helping ensure equity in access and distribution.
https://twitter.com/NYCHealthCommr/status/1488184099416293383?s=20&t=_2T3BWULPSTkyjH0WLEInQ
Still, during the omicron wave, the COVID-19 hospitalization rate was more than two times greater among Black New Yorkers compared to White New Yorkers. Hospitalizations were also disproportionately higher in neighborhoods with a high percentage of Black residents. 



Even before the pandemic, anti-Black structural racism led to a four-year lower life expectancy among Black New Yorkers. This trend is due to a host of social, structural and downstream factors. 

While these analyses are essential to guiding anti-racism efforts, they are limited by available demographic data and require directly addressing in all public health surveillance and improvement programming from collection to analysis.
Targeted community engagement strategies contributed to closing racial equity gaps in
vaccination rates. Our vaccine equity strategy boosted vaccination rates in marginalized communities, in combination with NYC’s vaccine policies. nyc.gov/trie #PublicHealthCorps
vaccination rates. Our vaccine equity strategy boosted vaccination rates in marginalized communities, in combination with NYC’s vaccine policies. nyc.gov/trie #PublicHealthCorps
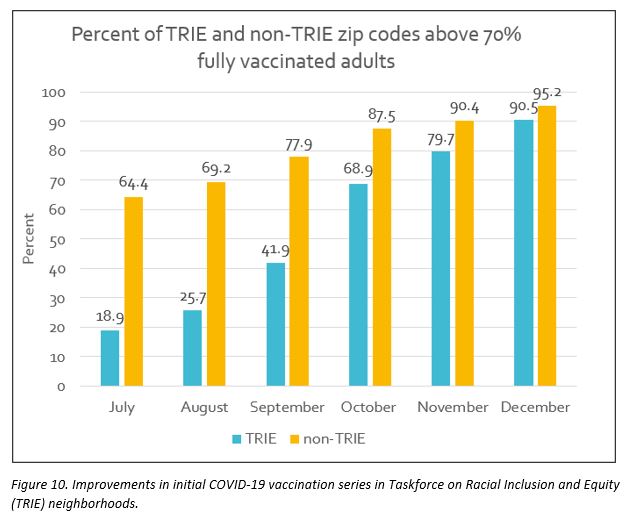
While more work is needed, this demonstrates the success and importance of community- and equity-based approaches. We call on our partners to take additional concrete actions under a shared vision of reducing racial inequities in the COVID-19 pandemic and beyond.
Race and place matter to health equity. Our ACTIONS encompass investment in priority neighborhoods; improved access to care, including vaccination and COVID-19 treatments; and community engagement with cultural humility. Read more on our path forward: on.nyc.gov/3C7PUVu
• • •
Missing some Tweet in this thread? You can try to
force a refresh








