@ASPCardio Statement led by @DBelardoMD & myself w/ @ErinMichos @RonBlankstein @rblument1 @kcferdmd @KCKlatt @pnatarajanmd @DrOstfeld @KoushikReddyMD @deirdre_tobias @KevinH_PhD Practical Evidence-Based Approaches to Nutritional Modifications to ⬇️ #ASCVD
bit.ly/3tRD0XP
bit.ly/3tRD0XP

Recommendations to ⬇️ #ASCVD with Nutrition:
1. Primary and Secondary Prevention of ASCVD: A diet consisting predominantly of fruits, vegetables, legumes, nuts, seeds, plant protein & fatty fish is optimal for the prevention of ASCVD
🥕🥬🥦🫑🥒🍅🧅🧄🥔🐟🍉🍒🍏🍊🍇🍋🍎🌶️🍈🍐🌿🌱
1. Primary and Secondary Prevention of ASCVD: A diet consisting predominantly of fruits, vegetables, legumes, nuts, seeds, plant protein & fatty fish is optimal for the prevention of ASCVD
🥕🥬🥦🫑🥒🍅🧅🧄🥔🐟🍉🍒🍏🍊🍇🍋🍎🌶️🍈🍐🌿🌱
2. Hyperlipidemia: Replacing saturated fat with polyunsaturated and monounsaturated fat, reducing dietary cholesterol intake, and increasing intake of fiber rich foods, can all lead to a ⬇️ in LDL-C and apoB.
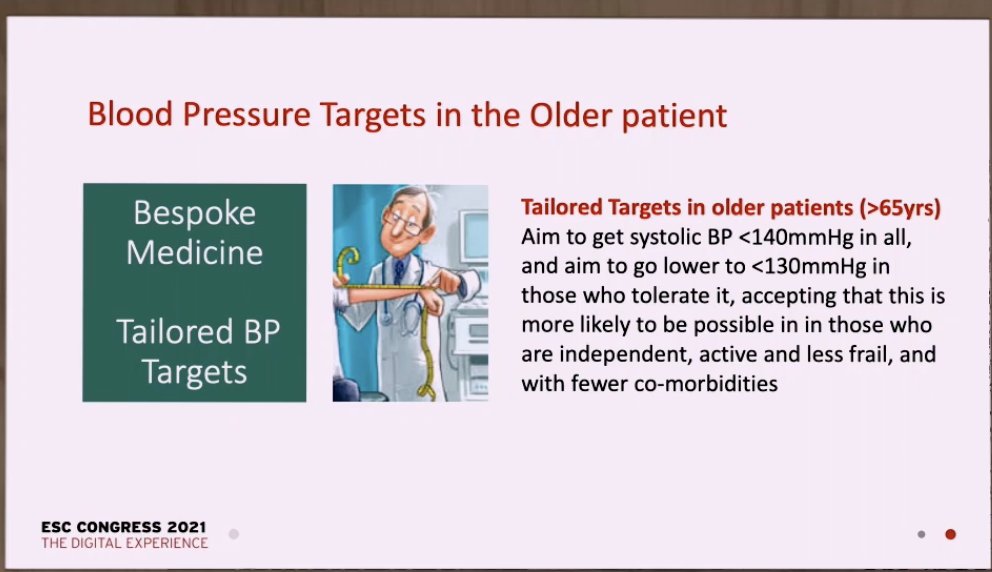
3. Hypertension: Eating a low sodium DASH dietary pattern, rich in dietary potassium from fruits and vegetables, is recommended for the prevention and treatment of hypertension.
@kcferdmd @BakrisGeorge @NHLBI_Translate @AnastasiaSMihai @jbrianbyrd @ASPCardio
@kcferdmd @BakrisGeorge @NHLBI_Translate @AnastasiaSMihai @jbrianbyrd @ASPCardio
4. Type 2 Diabetes: Preventing weight gain and obesity is pivotal for diabetes prevention. Thus, effective strategies for weight loss and management are likely beneficial for mitigating diabetes progression
bit.ly/3tRD0XP
bit.ly/3tRD0XP
5. Obesity: The importance of diet for prevention of weight gain and obesity is well demonstrated, with poor nutritional habits playing a role in gradual midlife weight gain.
@bjcohenmd @EugeniaGianos @DrEugeneYang @KTamirisaMD @DrNasrien @khurramn1 @AnumSaeedMD @netta_doc
@bjcohenmd @EugeniaGianos @DrEugeneYang @KTamirisaMD @DrNasrien @khurramn1 @AnumSaeedMD @netta_doc
6. Vitamin Supplementation: Vitamin supplementation is not routinely recommended for the prevention of ASCVD; supplementation should be individualized and recommended in those where it is necessary to meet nutrient requirements or as otherwise medically indicated.
7. Children: Primary prevention of ASCVD should begin as early as possible, emphasizing small changes in eating behaviors to promote nutrient-dense dietary patterns to establish nutrition-related goals that are focused, feasible, and measurable.
Dr. Renee Rodriguez-TY!
Dr. Renee Rodriguez-TY!
8. Older Adults: Nutrition therapy can have substantial benefits for individuals across the life span, including older adults with existing disease burden. Dietary recommendations to reduce cardiovascular risk should be counseled, tailored to the patient
9. Social Determinants of Health: Healthcare providers should evaluate patients for inequities in food access and socioeconomic resources, while providing culturally relevant nutrition resources when appropriate.
10. Multidisciplinary approach: Medical nutrition therapy, in collaboration with registered dietitians, results in greater improvements in cardiovascular disease risk factors and referral should be encouraged. @KCKlatt @deirdre_tobias @RonBlankstein
bit.ly/3tRD0XP
bit.ly/3tRD0XP
• • •
Missing some Tweet in this thread? You can try to
force a refresh