1/ Ironic that in the latest "shake-down" of #NC physicians @BlueCrossNC starts out by saying that they are a "non-profit" seeking to drive down "the costs of delivering healthcare." Let's look at their CEO comp. in '20--$3.14M + 8 of their execs. received at least $1.33M in.....
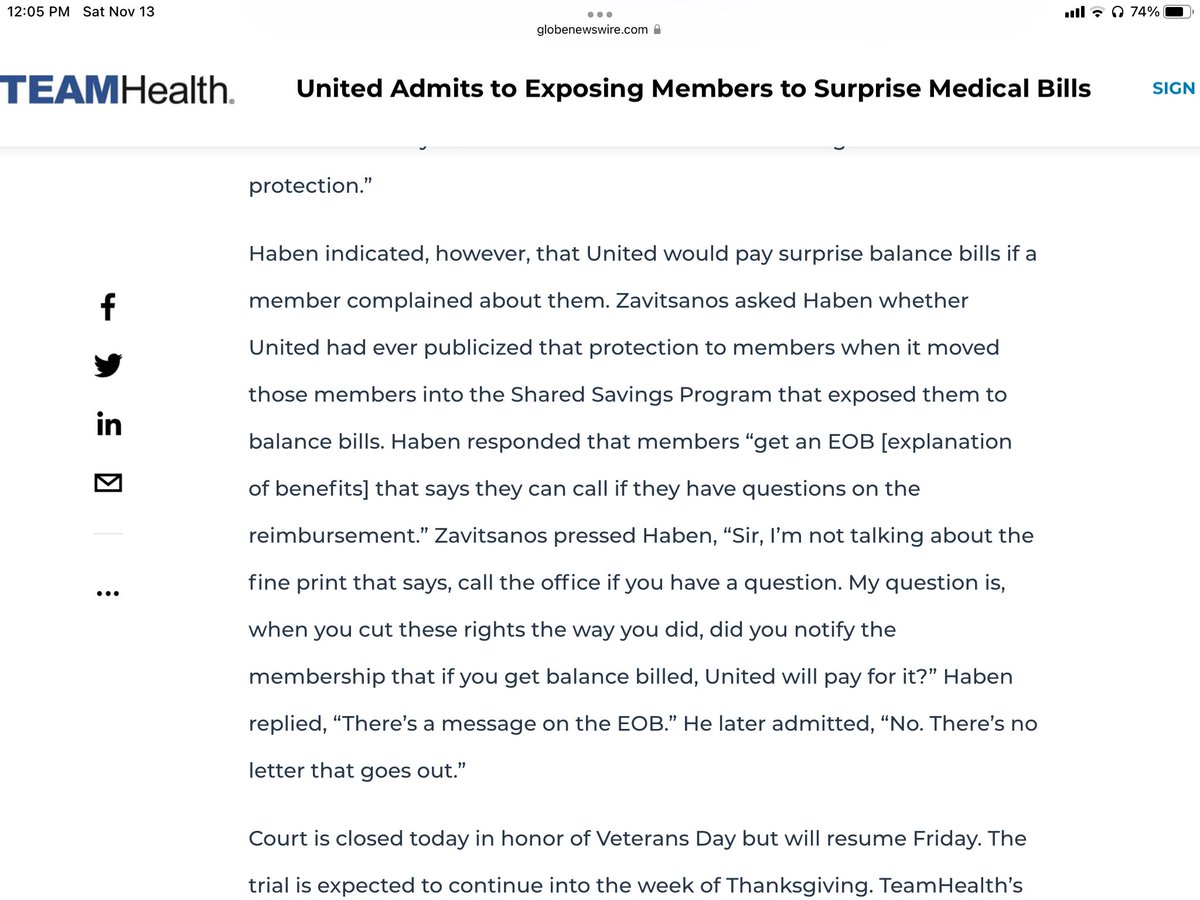
2/ compensation in '19; you may remember back in Nov. '21, citing to the #NoSurprisesAct, #NCBlue demanded that 54 hospital based groups immediately agree to contract rate reductions in the range of -5% to -30% or face contract termination--thought the letter was "fake news".....
3/ and it wasn't as an NC practice manager who knew the BCBSNC VP who signed the letter called him & said "is this for real?" Yes it was, said the VP; anyway the latest iteration of @BlueCrossNC w/ 60-70% of the commercial market using it's oligopoly power is cited below; for....
4/ anyone who thinks the #NSA is just about out of network rates--it is not & never has been--it's always been about driving all rates down & managing the median in network down. @ACEPNow @ASAGrassroots @RadiologyACR @AmerMedicalAssn @ahahospitals @texmed 



5/@drdanchoi @813JAFERD @amychomd @sonodoc99 @Valleus556 @ercoderguy @Reese_Tassey @fuzzymittens @MarilynHeineMD @TakeWeightOffMD @SunnyJhaMD @jencasmd @JenniTelesz @purviparikhmd @movinmeat @ERGoddessMD @NC_ACEP @GrassrootsEM @GAemergency @EDPMA @RichDuszak @reh3md
Source for salary information: journalnow.com/record-expense…
• • •
Missing some Tweet in this thread? You can try to
force a refresh