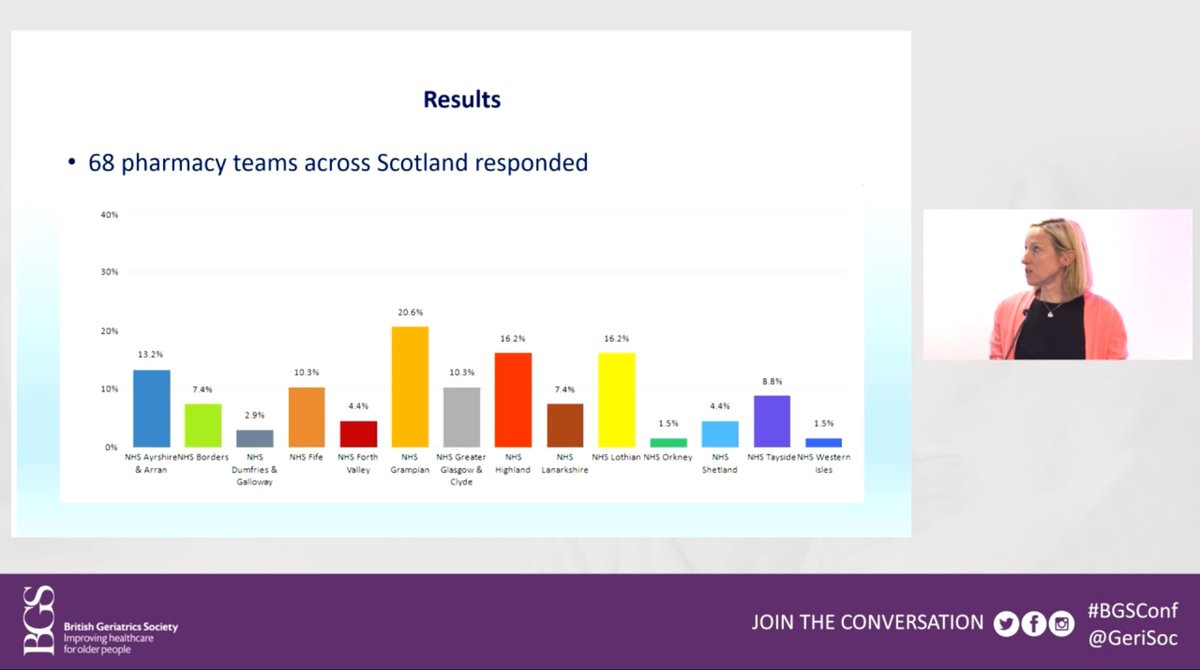
Some further slides from today’s #bgsconf, this time on Pharmacy support to care homes.
Spoiler: it is a bit variable!



Spoiler: it is a bit variable!



So what are the roles undertaken by Pharmacy teams in #CareHomes?
Lots of different things!
#bgsconf
Lots of different things!
#bgsconf

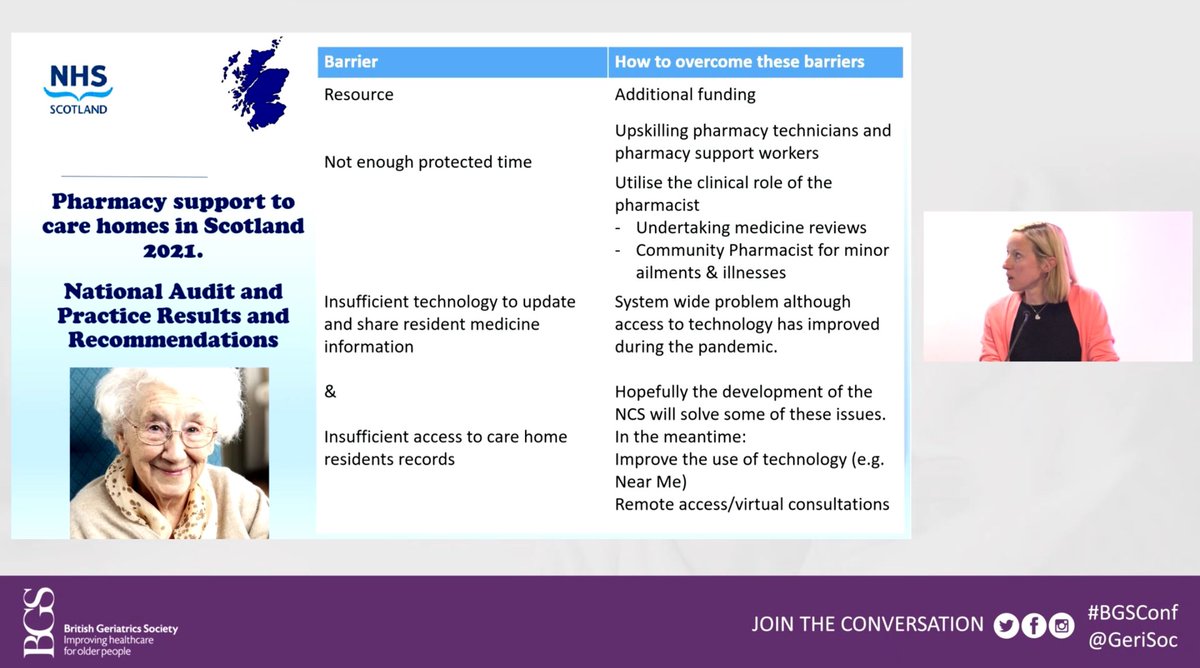
Changes related to #COVID19, some barriers to change, and what to do about them…
And finally some general recommendations.
All at this afternoon’s #bgsconf


And finally some general recommendations.
All at this afternoon’s #bgsconf


• • •
Missing some Tweet in this thread? You can try to
force a refresh