
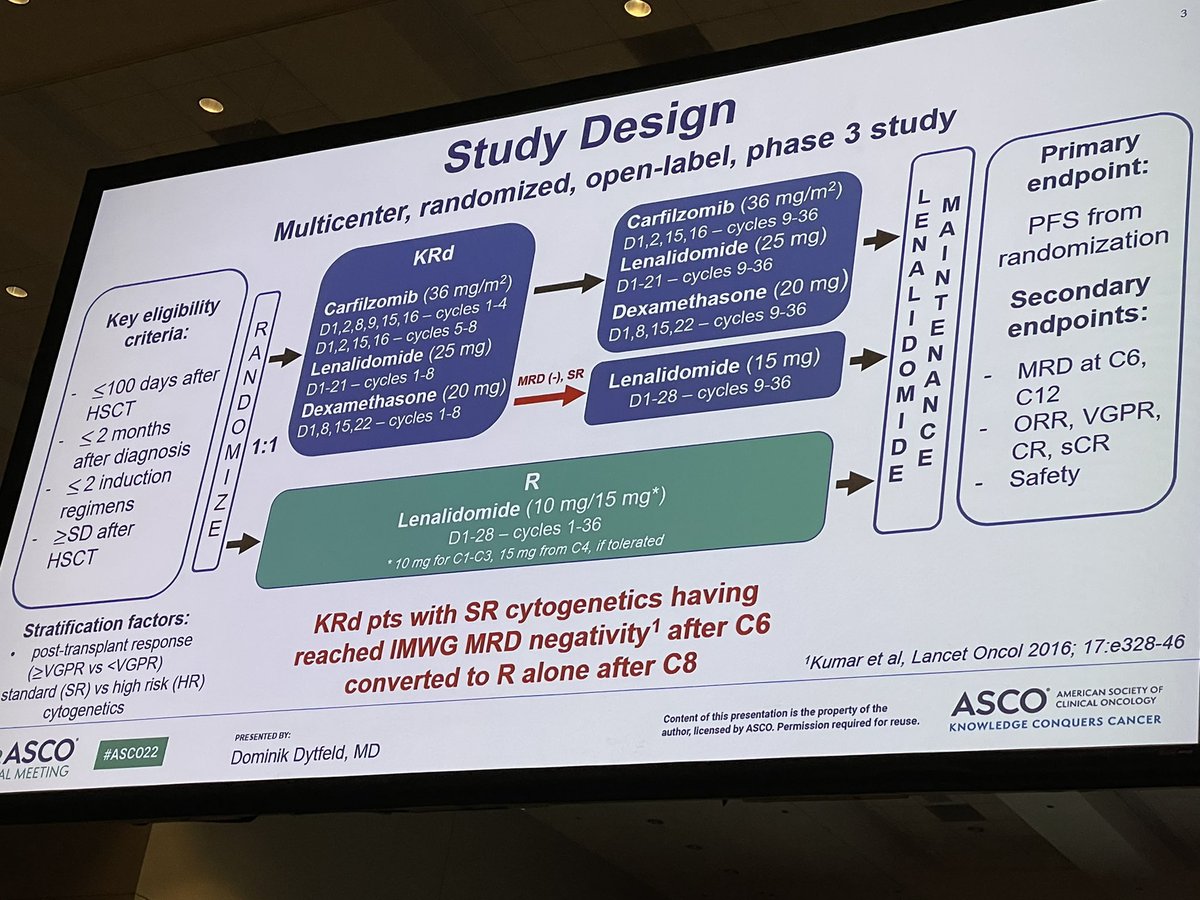
The ATLAS trial presented at #ASCO22
-Given design (3 drugs maint, and PFS as endpoint), answer was obvious.
-Low power to detect any survival difference
-No quality of life presented, suspect would be worse if properly measured in KRd arm
-Please don’t adopt in practice! #mmsm



-Given design (3 drugs maint, and PFS as endpoint), answer was obvious.
-Low power to detect any survival difference
-No quality of life presented, suspect would be worse if properly measured in KRd arm
-Please don’t adopt in practice! #mmsm



Other thoughts:
-induction suboptimal by US standards, suspect benefit would be even less if len was given. Remember- that len based consolidation helps if induction regimen did not contain len (emn02-h095), but does NOT help if induction regimen contains len (STAMINA trial)
-induction suboptimal by US standards, suspect benefit would be even less if len was given. Remember- that len based consolidation helps if induction regimen did not contain len (emn02-h095), but does NOT help if induction regimen contains len (STAMINA trial)

Presenter described treatment as well tolerated. There was a treatment related death in KRd arm. After randomization, 5 patient in len arm withdrew due to “patient decision/other” but 16 withdrew in KRd arm.
That’s informative censoring.And likely because KRd was tough to handle
That’s informative censoring.And likely because KRd was tough to handle
• • •
Missing some Tweet in this thread? You can try to
force a refresh









