1/As my attending once said, “If I’ve seen it once, I’ve seen it…well once.”
A 🧵about an interesting case that I’ve seen once in 15 years and never again. #medtwitter #radres #FOAMed #FOAMrad #neurorad #Meded #Neurosurgery #HNrad
A 🧵about an interesting case that I’ve seen once in 15 years and never again. #medtwitter #radres #FOAMed #FOAMrad #neurorad #Meded #Neurosurgery #HNrad

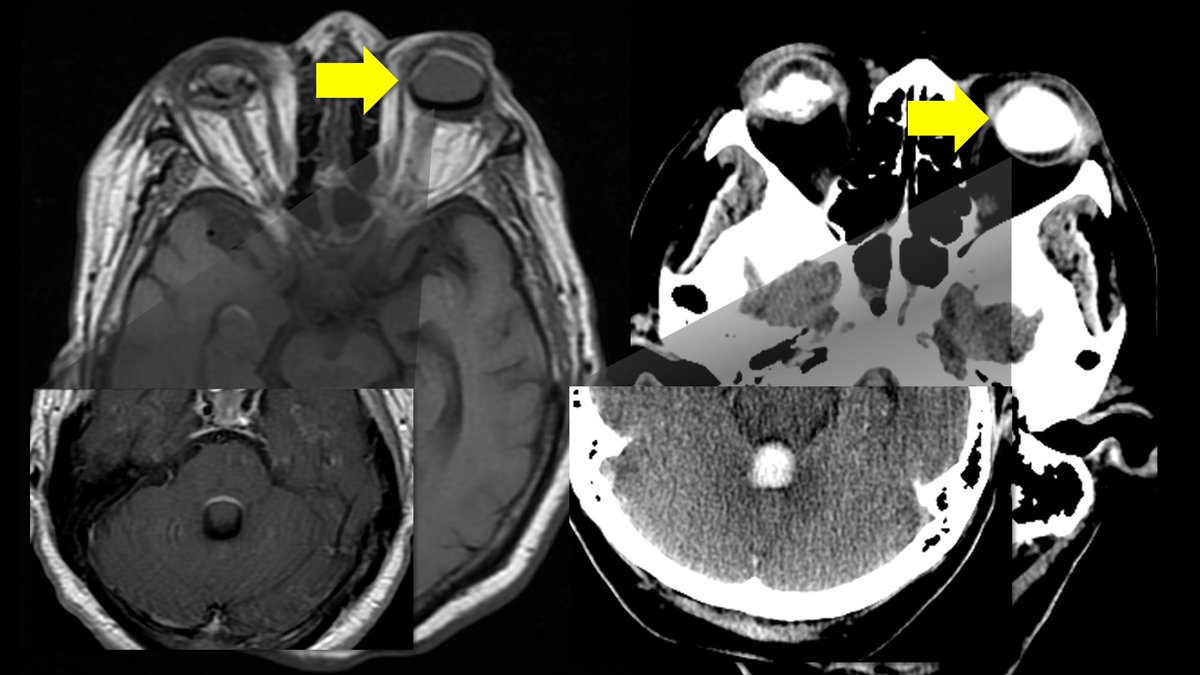
2/Pt with history only of diabetes came in with altered mental status. There were these super bright round balls in their ventricles. It looked like a snowman massacre happened, with big round snowballs in the ventricles 

3/On MRI, these had intrinsic T1 hyperintensity w/chemical shift artifact--they looked like boba tea pearls floating in the ventricles. Typically, we think of chemical shift w/fat--but these were not fat on the CT!! They did not enhance & otherwise, brain was unremarkable for age 

4/The answer is looking you right in the eye! This is intraventricular extension of silicone from a silicone retinopexy. Silicone dissections along the optic sheath into subarachnoid space & ventricles. It is typically asymptomatic. And now you've seen as many of these as me!😉 
• • •
Missing some Tweet in this thread? You can try to
force a refresh






















