@TumorBoardTues @CaterinaSpo 1/16 #TumorBoardTuesday #BreastCancer #OncTwitter
52yo 👩🏻 post-menopausal, no sig comorbidities.
FH: 2 sisters with young onset BC.
Genetic testing: BRCA1+
🔪‘Bilat Mastectomy + left SLNB:
left IDC G3
ER 0%
PgR 0%
HER2 1+ (TNBC)
Ki67 95%
stage pT1c (17 mm) pN0
52yo 👩🏻 post-menopausal, no sig comorbidities.
FH: 2 sisters with young onset BC.
Genetic testing: BRCA1+
🔪‘Bilat Mastectomy + left SLNB:
left IDC G3
ER 0%
PgR 0%
HER2 1+ (TNBC)
Ki67 95%
stage pT1c (17 mm) pN0
@TumorBoardTues @CaterinaSpo 2/16 #TumorBoardTuesday
👩🏻 adjuvant TC ➡️ discontinued after 3rd cycle➡️poor tolerance & recurring FN
22 mo. later --> CT: Lt supraclavicular & multi mediastinal LN met, Rt pleural effusion
🔬LN bx: metastasis of TNBC (ER 0%, PgR 0%, HER2 1+, Ki67 81%). PD-L1 CPS: <10%.
👩🏻 adjuvant TC ➡️ discontinued after 3rd cycle➡️poor tolerance & recurring FN
22 mo. later --> CT: Lt supraclavicular & multi mediastinal LN met, Rt pleural effusion
🔬LN bx: metastasis of TNBC (ER 0%, PgR 0%, HER2 1+, Ki67 81%). PD-L1 CPS: <10%.
@TumorBoardTues @CaterinaSpo 3/16 #TumorBoardTuesday #BCSM
🤨 Which 1L systemic treatment would you choose for a patient with a gBRCA1m and metastatic recurrence of TNBC with the above 👆🏽 characteristics?
@ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab
🤨 Which 1L systemic treatment would you choose for a patient with a gBRCA1m and metastatic recurrence of TNBC with the above 👆🏽 characteristics?
@ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab
@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab 4/16 #TumorBoardTuesday #BreastCancer
After discussion about pros & cons of the available options, 🤝 patient agrees to pursue 1L treatment with a PARP-Inhibitor.
🤨 Which PARPi would you choose, given the available data and prior experience with adjuvant ChT?
After discussion about pros & cons of the available options, 🤝 patient agrees to pursue 1L treatment with a PARP-Inhibitor.
🤨 Which PARPi would you choose, given the available data and prior experience with adjuvant ChT?
@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab 5/16 #TumorBoardTuesday #BCSM
👨🏻🏫Mini tweetorial 1👩🏼🏫
✨BRCA+ TNBC
📍High rate of gBRCA mut in TNBC (10-20%)
📍BRCA mut carriers ➡️ lower age at diagnosis
📍PARPi act through synthetic lethality: ⬆️🧬 ss breaks converted to irreparable ds breaks in BRCA1/2-defective cells
👨🏻🏫Mini tweetorial 1👩🏼🏫
✨BRCA+ TNBC
📍High rate of gBRCA mut in TNBC (10-20%)
📍BRCA mut carriers ➡️ lower age at diagnosis
📍PARPi act through synthetic lethality: ⬆️🧬 ss breaks converted to irreparable ds breaks in BRCA1/2-defective cells

@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD 6/16 #TumorBoardTuesday
👨🏻🏫Mini tweetorial 2👩🏼🏫
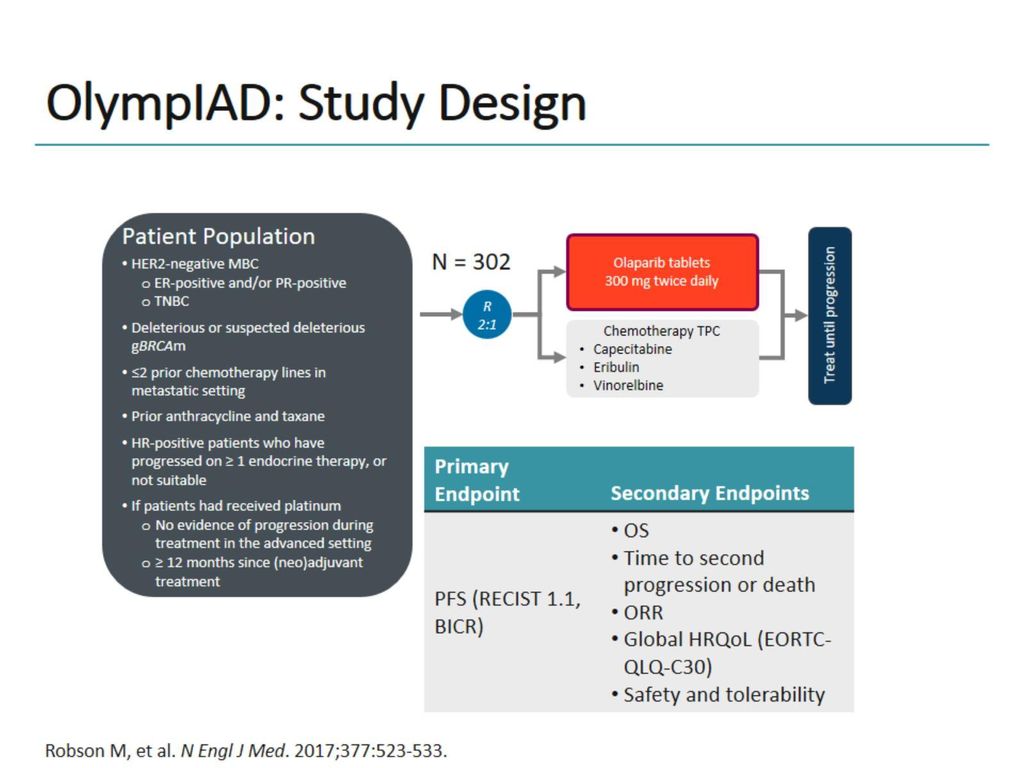
✨2017, OlympiAD✨
1st phase III trial to demonstrate 👍🏽 of PARPi Olaparib vs treatment of physician’s choice (TPC) in patients with gBRCAm & HER2-negative metastatic BrCa previously treated with Taxanes and Anthracyclines.
👨🏻🏫Mini tweetorial 2👩🏼🏫
✨2017, OlympiAD✨
1st phase III trial to demonstrate 👍🏽 of PARPi Olaparib vs treatment of physician’s choice (TPC) in patients with gBRCAm & HER2-negative metastatic BrCa previously treated with Taxanes and Anthracyclines.
@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD @BarbaraPistill2 @elmayermd @JaniceTNBCmets @MridulaGeorgeMD @dradityabardia @naborala 7/16 #TumorBoardTuesday #BreastCancer
👨🏻🏫Mini tweetorial 3👩🏼🏫
✨2017, OlympiA✨
📈 ORR: 59.9% in Olaparib group vs 28.8% in TPC group
📉 mPFS: 7.0 vs. 4.2 mo (HR 0.58, 95% CI 0.43 to 0.80; P<0.001)
nejm.org/doi/full/10.10…
👨🏻🏫Mini tweetorial 3👩🏼🏫
✨2017, OlympiA✨
📈 ORR: 59.9% in Olaparib group vs 28.8% in TPC group
📉 mPFS: 7.0 vs. 4.2 mo (HR 0.58, 95% CI 0.43 to 0.80; P<0.001)
nejm.org/doi/full/10.10…

@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD @BarbaraPistill2 @elmayermd @JaniceTNBCmets @MridulaGeorgeMD @dradityabardia @naborala @DrRBarroso @nicolobattisti @matteolambe @E_de_Azambuja @jhaveri_komal @BianchiniGP @aftimosp 8/16 #TumorBoardTuesday
👨🏻🏫Mini tweetorial 4👩🏼🏫
✨2018, EMBRACA✨
Parallel ph III trial shows significant efficacy of Talazoparib monotherapy vs TPS in similar population (patients with gBRCAm & HER2-negative metastatic BrCa previously treated with Taxanes or Anthracyclines)
👨🏻🏫Mini tweetorial 4👩🏼🏫
✨2018, EMBRACA✨
Parallel ph III trial shows significant efficacy of Talazoparib monotherapy vs TPS in similar population (patients with gBRCAm & HER2-negative metastatic BrCa previously treated with Taxanes or Anthracyclines)

@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD @BarbaraPistill2 @elmayermd @JaniceTNBCmets @MridulaGeorgeMD @dradityabardia @naborala @DrRBarroso @nicolobattisti @matteolambe @E_de_Azambuja @jhaveri_komal @BianchiniGP @aftimosp @lab_kok @hthrparsons @hoperugo 9/16 #TumorBoardTuesday #BCSM
👨🏻🏫Mini tweetorial 5👩🏼🏫
✨2018, EMBRACA✨
📈 ORR: 62.6% in Talazoparib group vs. 27.2% in TPC group
📉 mPFS: 8.6 vs. 5.6 mo (HR 0.54; 95% CI 0.41 to 0.71; P<0.001)
📚 nejm.org/doi/10.1056/NE…
👨🏻🏫Mini tweetorial 5👩🏼🏫
✨2018, EMBRACA✨
📈 ORR: 62.6% in Talazoparib group vs. 27.2% in TPC group
📉 mPFS: 8.6 vs. 5.6 mo (HR 0.54; 95% CI 0.41 to 0.71; P<0.001)
📚 nejm.org/doi/10.1056/NE…

@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD @BarbaraPistill2 @elmayermd @JaniceTNBCmets @MridulaGeorgeMD @dradityabardia @naborala @DrRBarroso @nicolobattisti @matteolambe @E_de_Azambuja @jhaveri_komal @BianchiniGP @aftimosp @lab_kok @hthrparsons @hoperugo @ADesaiMD @FrancescoSche20 @kevinpunie @adrianakahnmd @geoff_oxnard @drteplinsky @DrChoueiri @Carlos_Wagner1 10/16 #TumorBoardTuesday
👨🏻🏫Mini tweetorial 6👩🏼🏫
📌No sig OS benefit found in both trials
✨OlympiA: mOS Olaparib 19.3 mo; HR Olaparib vs TPC: 0.90 (95% CI 0.66–1.23; P = 0.513)
✨EMBRACA: mOS Talazoparib 19.3 mo; HR (OS) Talazo vs TPC: 0.848 (95% CI 0.670-1.073; P= 0.17)
👨🏻🏫Mini tweetorial 6👩🏼🏫
📌No sig OS benefit found in both trials
✨OlympiA: mOS Olaparib 19.3 mo; HR Olaparib vs TPC: 0.90 (95% CI 0.66–1.23; P = 0.513)
✨EMBRACA: mOS Talazoparib 19.3 mo; HR (OS) Talazo vs TPC: 0.848 (95% CI 0.670-1.073; P= 0.17)

@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD @BarbaraPistill2 @elmayermd @JaniceTNBCmets @MridulaGeorgeMD @dradityabardia @naborala @DrRBarroso @nicolobattisti @matteolambe @E_de_Azambuja @jhaveri_komal @BianchiniGP @aftimosp @lab_kok @hthrparsons @hoperugo @ADesaiMD @FrancescoSche20 @kevinpunie @adrianakahnmd @geoff_oxnard @drteplinsky @DrChoueiri @Carlos_Wagner1 @thenasheffect @SidYadavMD @Icro_Meattini @DrBonillaOnc 11/16 #TumorBoardTuesday #BCSM
👨🏻🏫Mini tweetorial 7👩🏼🏫
With current available data
✨Olaparib or Talazoparib✨
✅Usually relies on toxicity
✅Both PARPi show good safety
🫧mainly G1/G2 AEs
🫧PROs & QoL studies 👉🏽 significant improvements with PARPi vs ChT
👨🏻🏫Mini tweetorial 7👩🏼🏫
With current available data
✨Olaparib or Talazoparib✨
✅Usually relies on toxicity
✅Both PARPi show good safety
🫧mainly G1/G2 AEs
🫧PROs & QoL studies 👉🏽 significant improvements with PARPi vs ChT
@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD @BarbaraPistill2 @elmayermd @JaniceTNBCmets @MridulaGeorgeMD @dradityabardia @naborala @DrRBarroso @nicolobattisti @matteolambe @E_de_Azambuja @jhaveri_komal @BianchiniGP @aftimosp @lab_kok @hthrparsons @hoperugo @ADesaiMD @FrancescoSche20 @kevinpunie @adrianakahnmd @geoff_oxnard @drteplinsky @DrChoueiri @Carlos_Wagner1 @thenasheffect @SidYadavMD @Icro_Meattini @DrBonillaOnc 12/16 #TumorBoardTuesday
👨🏻🏫Mini tweetorial 8👩🏼🏫
✨Olaparib or Talazoparib✨
Most common AEs:
📌Olaparib
🤢 58.0%
🤮 32.2%
🩸anemia 40.0%
😴 fatigue 29.8%
🦴 neutropenia 27.3%
📌Talazoparib
🩸 54.9%
😴 51.4%
🤢 49.7%
🦴 neutropenia 36.0%
🤕headache 33.9%
👨🏻🏫Mini tweetorial 8👩🏼🏫
✨Olaparib or Talazoparib✨
Most common AEs:
📌Olaparib
🤢 58.0%
🤮 32.2%
🩸anemia 40.0%
😴 fatigue 29.8%
🦴 neutropenia 27.3%
📌Talazoparib
🩸 54.9%
😴 51.4%
🤢 49.7%
🦴 neutropenia 36.0%
🤕headache 33.9%
@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD @BarbaraPistill2 @elmayermd @JaniceTNBCmets @MridulaGeorgeMD @dradityabardia @naborala @DrRBarroso @nicolobattisti @matteolambe @E_de_Azambuja @jhaveri_komal @BianchiniGP @aftimosp @lab_kok @hthrparsons @hoperugo @ADesaiMD @FrancescoSche20 @kevinpunie @adrianakahnmd @geoff_oxnard @drteplinsky @DrChoueiri @Carlos_Wagner1 @thenasheffect @SidYadavMD @Icro_Meattini @DrBonillaOnc 13/16 #TumorBoardTuesday
Back to our case🔎
Patient started Olaparib 300mg BID
After 3 months 👉🏽 PR
-->Treatment currently ongoing!
Overall well tolerated:
G1 nausea prn antiemetics
G3 recurrent anemia 👍🏽 after dose ⬇️ reduction (1st level 250mg bid)
Back to our case🔎
Patient started Olaparib 300mg BID
After 3 months 👉🏽 PR
-->Treatment currently ongoing!
Overall well tolerated:
G1 nausea prn antiemetics
G3 recurrent anemia 👍🏽 after dose ⬇️ reduction (1st level 250mg bid)
@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD @BarbaraPistill2 @elmayermd @JaniceTNBCmets @MridulaGeorgeMD @dradityabardia @naborala @DrRBarroso @nicolobattisti @matteolambe @E_de_Azambuja @jhaveri_komal @BianchiniGP @aftimosp @lab_kok @hthrparsons @hoperugo @ADesaiMD @FrancescoSche20 @kevinpunie @adrianakahnmd @geoff_oxnard @drteplinsky @DrChoueiri @Carlos_Wagner1 @thenasheffect @SidYadavMD @Icro_Meattini @DrBonillaOnc 14/16 #TumorBoardTuesday
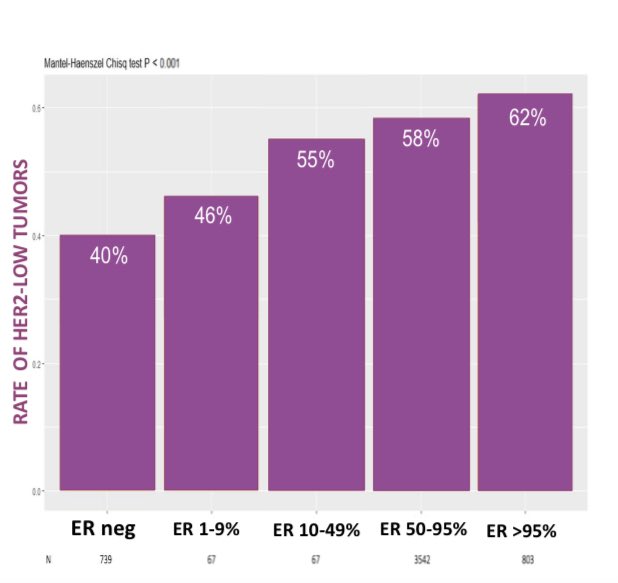
In case of PD, several options would be available, including chemo & saci.
💥T-DXd now also included in @NCCN guidelines for pts with pretreated HER2-low MBC
✨DB-04 👉🏽 relevant benefit in PFS & OS- but only 58 TNBC pts
nejm.org/doi/10.1056/NE…
In case of PD, several options would be available, including chemo & saci.
💥T-DXd now also included in @NCCN guidelines for pts with pretreated HER2-low MBC
✨DB-04 👉🏽 relevant benefit in PFS & OS- but only 58 TNBC pts
nejm.org/doi/10.1056/NE…
@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD @BarbaraPistill2 @elmayermd @JaniceTNBCmets @MridulaGeorgeMD @dradityabardia @naborala @DrRBarroso @nicolobattisti @matteolambe @E_de_Azambuja @jhaveri_komal @BianchiniGP @aftimosp @lab_kok @hthrparsons @hoperugo @ADesaiMD @FrancescoSche20 @kevinpunie @adrianakahnmd @geoff_oxnard @drteplinsky @DrChoueiri @Carlos_Wagner1 @thenasheffect @SidYadavMD @Icro_Meattini @DrBonillaOnc @NCCN 15/16 #TumorBoardTuesday
‘22 OlympiA: 👉🏽olaparib approval for adjuvant tx of gBRCAm HER2-neg high-risk EBC pretreated with (N)ACT.
🤨gBRCA1m pt presents with ⬆️ risk disease & receive adj olaparib x 1y, what tx would you indicate in 1L in case of met recurrence (TFI 18 mos)?
‘22 OlympiA: 👉🏽olaparib approval for adjuvant tx of gBRCAm HER2-neg high-risk EBC pretreated with (N)ACT.
🤨gBRCA1m pt presents with ⬆️ risk disease & receive adj olaparib x 1y, what tx would you indicate in 1L in case of met recurrence (TFI 18 mos)?
@TumorBoardTues @CaterinaSpo @ErikaHamilton9 @FilipaLynce @maryam_lustberg @SusanGKomen @HeekeMd @stolaney1 @barrosolab @DrReshmaMahtani @NicoleKuderer @darioT_ @prat_aleix @FilippoMontemu1 @JavierCortesMD @BarbaraPistill2 @elmayermd @JaniceTNBCmets @MridulaGeorgeMD @dradityabardia @naborala @DrRBarroso @nicolobattisti @matteolambe @E_de_Azambuja @jhaveri_komal @BianchiniGP @aftimosp @lab_kok @hthrparsons @hoperugo @ADesaiMD @FrancescoSche20 @kevinpunie @adrianakahnmd @geoff_oxnard @drteplinsky @DrChoueiri @Carlos_Wagner1 @thenasheffect @SidYadavMD @Icro_Meattini @DrBonillaOnc @NCCN 16/16 #TumorBoardTuesday
Data lacking
Recurrence timing after adjuvant Olaparib:
👉🏽long TFI ➡️ re-treatment with PARPi may be considered (Olaparib or Talazoparib)
👉🏽if recurrence ON therapy or WITHIN 1 YEAR from adjuvant Olaparib➡️new tx
nature.com/articles/s4157…
Data lacking
Recurrence timing after adjuvant Olaparib:
👉🏽long TFI ➡️ re-treatment with PARPi may be considered (Olaparib or Talazoparib)
👉🏽if recurrence ON therapy or WITHIN 1 YEAR from adjuvant Olaparib➡️new tx
nature.com/articles/s4157…
• • •
Missing some Tweet in this thread? You can try to
force a refresh