📌 Tweetorial on “IgA Nephropathy: Approach to treatment” based on @goKDIGO webinar by Dr. Richard Lafayette
🔸First step in management of IgAN: Determine the risk of disease progression based on GFR, proteinuria, BP & kidney biopsy findings👇🏽
1/
🔸First step in management of IgAN: Determine the risk of disease progression based on GFR, proteinuria, BP & kidney biopsy findings👇🏽
1/

📌 Approach to treatment of IgAN based on @goKDIGO guidelines👇🏽
🔸This Rx algorithm is NOT applicable to IgA deposition with minimal change disease, IgAN with AKI, IgAN with RPGN, IgA vasculitis, IgA-dominant post-infections GN & secondary forms of IgAN👇🏽
2/
🔸This Rx algorithm is NOT applicable to IgA deposition with minimal change disease, IgAN with AKI, IgAN with RPGN, IgA vasculitis, IgA-dominant post-infections GN & secondary forms of IgAN👇🏽
2/

📌 IgAN: All patients should receive supportive care:
🔸 Optimal BP management
🔸 Maximally tolerated ACEi/ARB
🔸 Lifestyle modification
🔸 Reduction of cardiovascular
risk👇🏽
3/

🔸 Optimal BP management
🔸 Maximally tolerated ACEi/ARB
🔸 Lifestyle modification
🔸 Reduction of cardiovascular
risk👇🏽
3/


📌 IgAN: Persistent proteinuria of >1g/d following at least 3-months of optimal supportive care then👇🏽
🔸Consider enrollment in a clinical trial
🔸If enrollment in a clinical trial is not possible then consider other therapies based on GFR👇🏽
4/
🔸Consider enrollment in a clinical trial
🔸If enrollment in a clinical trial is not possible then consider other therapies based on GFR👇🏽
4/

📌 Persistent proteinuria >1g/d despite maximal supportive therapy for at least 3-months & GFR of >30 ml/min then corticosteroids can be considered ‼️ BUT the risk/benefit profile of corticosteroids should be individually assessed
5/
5/
📌 Risk evaluation for corticosteroids
🔸 Relative contraindications for corticosteroid use in IgAN are:
-Low GFR <30 ml/min
-DM
-Obesity
-Latent infection
-Secondary diseases causing IgAN
-Peptic ulcer dz
-Psychiatric illness
-Severe osteoporosis
6/
🔸 Relative contraindications for corticosteroid use in IgAN are:
-Low GFR <30 ml/min
-DM
-Obesity
-Latent infection
-Secondary diseases causing IgAN
-Peptic ulcer dz
-Psychiatric illness
-Severe osteoporosis
6/

📌 IgAN: If GFR is <30 ml/min and kidney biopsy findings are more in line with fibrosis than with inflammation then continue maximal supportive care. Risk benefit profile of corticosteroids may not be favorable in such patients
7/
7/

📌 Before reviewing data on corticosteroid use in IgAN there are some considerations for special populations
🔸 Japanese: consider tonsillectomy
🔸 Chinese: consider MMF (steroid sparing)
These recommendations are based on less robust data👇🏽
8/


🔸 Japanese: consider tonsillectomy
🔸 Chinese: consider MMF (steroid sparing)
These recommendations are based on less robust data👇🏽
8/



📌 Role of corticosteroid use in IgAN
🔸This meta-analysis in 2012 showed a trend towards benefits of corticosteroids in IgAN but quality of studies included in this analysis was low limiting the generalizability of these findings
pubmed.ncbi.nlm.nih.gov/22539830/
9/
🔸This meta-analysis in 2012 showed a trend towards benefits of corticosteroids in IgAN but quality of studies included in this analysis was low limiting the generalizability of these findings
pubmed.ncbi.nlm.nih.gov/22539830/
9/

📌 Role of corticosteroids in IgAN: 🔸 Retrospective analysis of VALIGA study in 2015, used propensity scores to compare IgAN patients who received corticosteroids vs who did not. Corticosteroids provided renal protection👇🏽
pubmed.ncbi.nlm.nih.gov/25677392/
10/
pubmed.ncbi.nlm.nih.gov/25677392/
10/

📌 These studies led to RCTs evaluating role of corticosteroids in IgAN
🔸 STOP-IgAN Trial: RCT
📍Corticosteroids did not impact rate of change in GFR compared to supportive care👇🏽
📍Corticosteroids ⬆️ risk of adverse events👇🏽
pubmed.ncbi.nlm.nih.gov/26630142/
11/


🔸 STOP-IgAN Trial: RCT
📍Corticosteroids did not impact rate of change in GFR compared to supportive care👇🏽
📍Corticosteroids ⬆️ risk of adverse events👇🏽
pubmed.ncbi.nlm.nih.gov/26630142/
11/



📌 STOP-IgAN cohort was followed for over 5 years and there was no difference in kidney outcomes in the two groups that received corticosteroids vs supportive care👇🏽
12/
12/

📌 Then came the TESTING Trial: RCT comparing corticosteroids vs supportive care
pubmed.ncbi.nlm.nih.gov/28763548/
‼️Study was stopped by the data & safety monitoring committee due to serious adverse events in corticosteroid arm👇🏽
13/
pubmed.ncbi.nlm.nih.gov/28763548/
‼️Study was stopped by the data & safety monitoring committee due to serious adverse events in corticosteroid arm👇🏽
13/

📌 But by the time TESTING Trial was stopped there was data suggesting benefit in kidney outcomes in the corticosteroid arm
🔸This led to modification in study protocol: ⬇️ dose of steroids + pneumocystis prophylaxis —> TESTING low dose study👇🏽
14/
🔸This led to modification in study protocol: ⬇️ dose of steroids + pneumocystis prophylaxis —> TESTING low dose study👇🏽
14/

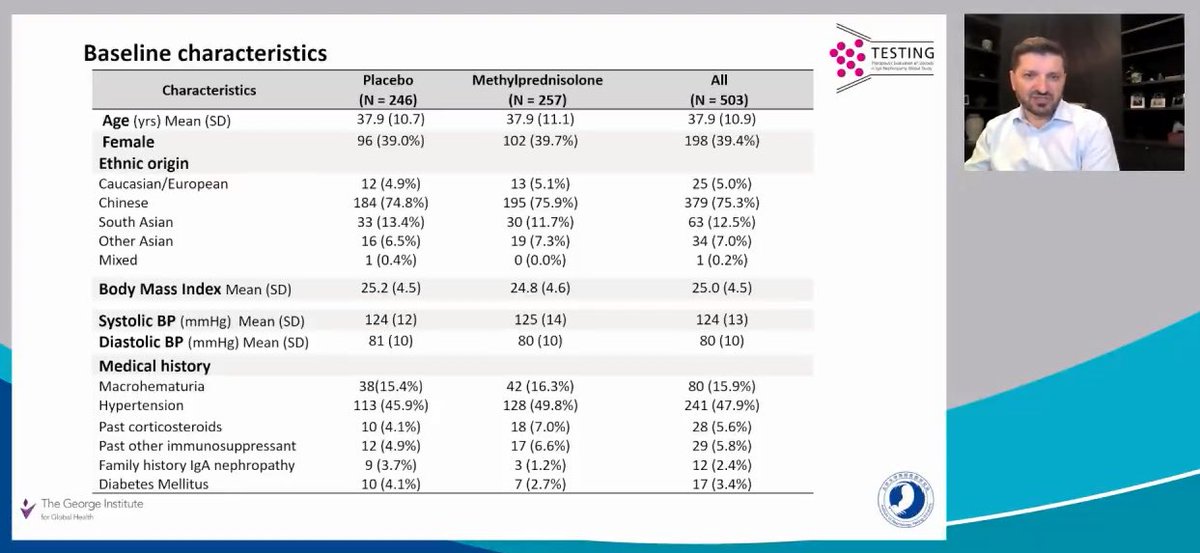
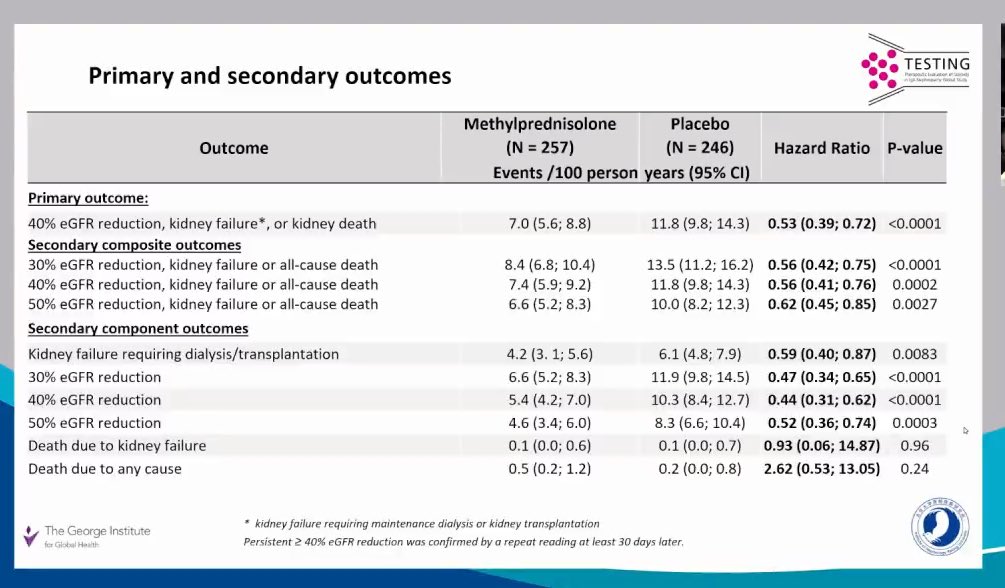
📌 TESTING Low dose study: published in 2022
pubmed.ncbi.nlm.nih.gov/35579642/
🔸Fewer kidney events (⬇️ in GFR, kidney failure, death due to kidney disease) occurred with corticosteroid use
15/

pubmed.ncbi.nlm.nih.gov/35579642/
🔸Fewer kidney events (⬇️ in GFR, kidney failure, death due to kidney disease) occurred with corticosteroid use
15/


📌 TESTING Trial
🔸No difference in efficacy between high dose vs low dose corticosteroids
🔸 Serious adverse events more common with corticosteroids vs placebo
🔸 More adverse events in high dose vs low dose corticosteroids
16/

🔸No difference in efficacy between high dose vs low dose corticosteroids
🔸 Serious adverse events more common with corticosteroids vs placebo
🔸 More adverse events in high dose vs low dose corticosteroids
16/


📌 Reduction in proteinuria occurred in both high dose & low dose corticosteroid groups
🔸 But proteinuria reduction persisted for 2 years & then dissipated
🔸 GFR improvement occurred early with steroid use & then remained parallel to placebo arm
17/
🔸 But proteinuria reduction persisted for 2 years & then dissipated
🔸 GFR improvement occurred early with steroid use & then remained parallel to placebo arm
17/

📌 TESTING Trial showed that low dose corticosteroids in IgAN result in more benefit than harm compared to high dose corticosteroids
‼️ BUT adverse events still occurred in the low dose corticosteroid group
18/
‼️ BUT adverse events still occurred in the low dose corticosteroid group
18/

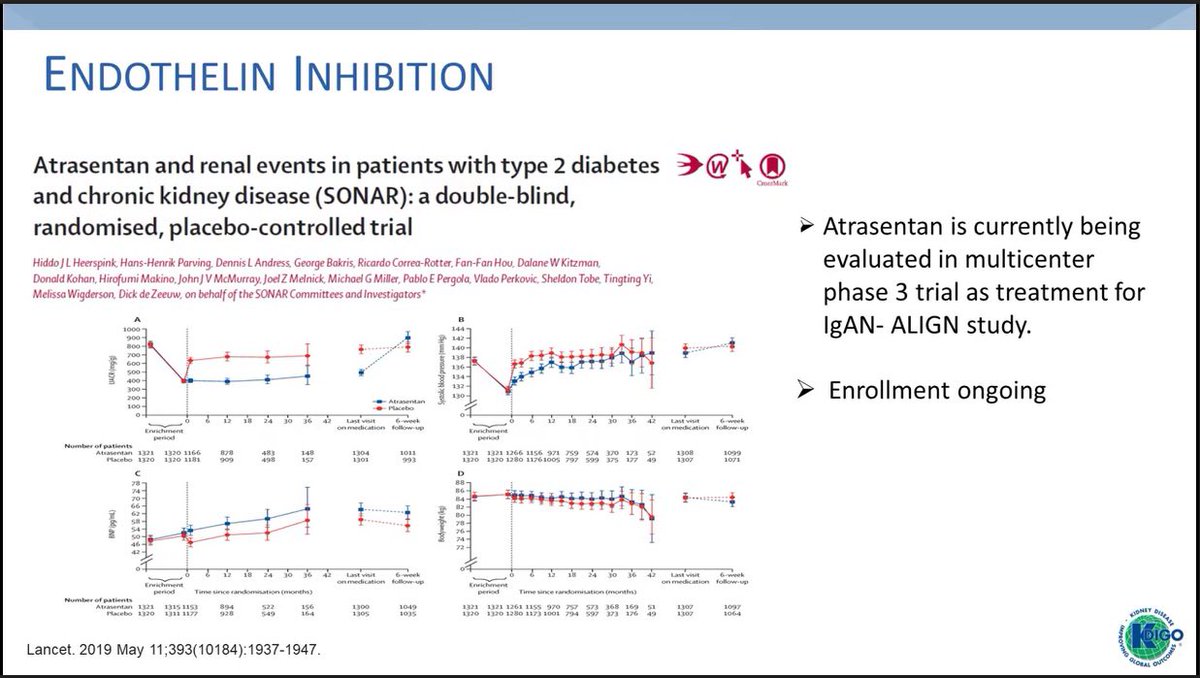
📌 There is a need for better therapeutic options for IgAN
🔸Emerging therapies:
📍Non-immunosuppressive therapies: SGLT2i, Endothelin receptor antagonist, Dual endothelin & angiotensin receptor blockade👇🏽
19/



🔸Emerging therapies:
📍Non-immunosuppressive therapies: SGLT2i, Endothelin receptor antagonist, Dual endothelin & angiotensin receptor blockade👇🏽
19/



📌 Emerging therapies
🔸Immune-modulating therapies:
📍 Targeted-release corticosteroid: Budenoside can reduce systemic exposure to corticosteroids & reduce steroid-related side effects
-NEFIGAN Study: phase 2
-NEFIGARD Study: phase 3
20/



🔸Immune-modulating therapies:
📍 Targeted-release corticosteroid: Budenoside can reduce systemic exposure to corticosteroids & reduce steroid-related side effects
-NEFIGAN Study: phase 2
-NEFIGARD Study: phase 3
20/




📌 Emerging therapies
🔸Targeted therapies based on IgAN pathogenesis:
📍Complement blockade
📍Anti B cell therapy
🔸Several on-going studies may identify efficacious & safe therapeutic options for treatment of IgAN
21/



🔸Targeted therapies based on IgAN pathogenesis:
📍Complement blockade
📍Anti B cell therapy
🔸Several on-going studies may identify efficacious & safe therapeutic options for treatment of IgAN
21/




📌Summary: IgAN Treatment
🔸Determine risk of disease progression (proteinuria,GFR, BP)
🔸Use maximal RAASi
🔸Steroids can be beneficial in pts. at high risk for disease progression but risk/benefit assessment is warranted before steroid initiation
End/

🔸Determine risk of disease progression (proteinuria,GFR, BP)
🔸Use maximal RAASi
🔸Steroids can be beneficial in pts. at high risk for disease progression but risk/benefit assessment is warranted before steroid initiation
End/


• • •
Missing some Tweet in this thread? You can try to
force a refresh