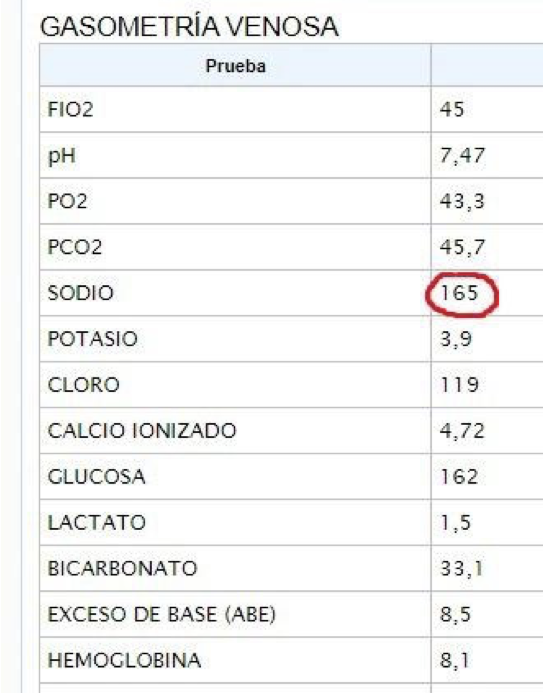
Young pt ➡️ 🏥 worsening shortness of breath
PMH: ESRD. Only 1 HD session/week. However, residual urine volume has now decreased substantially
On exam: BP 134/94, 2L O2,🧠✅, elevated JVP, decreased 🫁 sounds at bases, No murmurs, very mild edema. Functional left BC AVF
1/13

PMH: ESRD. Only 1 HD session/week. However, residual urine volume has now decreased substantially
On exam: BP 134/94, 2L O2,🧠✅, elevated JVP, decreased 🫁 sounds at bases, No murmurs, very mild edema. Functional left BC AVF
1/13


Careful examination of neck veins reveals no pulsations, even with pt sitting up 🤔
What could explain the absence of venous pulse? 2/13
What could explain the absence of venous pulse? 2/13
Answer is all of the above. JVP examination can be complicated in pts with ESRD.
In the absence of pulsations, I find #POCUS much helpful. Let's enhance our physical examination of congestion:
3/13



In the absence of pulsations, I find #POCUS much helpful. Let's enhance our physical examination of congestion:
3/13



#POCUS
#VExUS: Plethoric IVC, Hepatic Vein with significant flow reversal and Portal Vein with 100% pulsatility. (Intra-renal Doppler not done because of ESRD)
Also, PLAPS shows "spine sign" = Pleural Effusion
This is severe venous congestion!
(#VExUS refresher👇)
4/13
#VExUS: Plethoric IVC, Hepatic Vein with significant flow reversal and Portal Vein with 100% pulsatility. (Intra-renal Doppler not done because of ESRD)
Also, PLAPS shows "spine sign" = Pleural Effusion
This is severe venous congestion!
(#VExUS refresher👇)
4/13
Laboratory Data📊: BUN 104 mg/dl, K 6.2 meq/L, HCO3 16 meq/L, T Bili 0.5 mg/dl, ALT 1166 U/L, AST 697 U/L
What is the next step in management?
5/13
What is the next step in management?
5/13
🚨🚨🚨 This patient NEEDS further evaluation!
Venous congestion ≠ Hypervolemia
Venous congestion needs a differential diagnosis!!
DDx of severe congestion:
Left Heart Failure
PAH
High Output Heart Failure (AV Fistula)
Obstructive physiology
#Echofirst is a MUST
6/13
Venous congestion ≠ Hypervolemia
Venous congestion needs a differential diagnosis!!
DDx of severe congestion:
Left Heart Failure
PAH
High Output Heart Failure (AV Fistula)
Obstructive physiology
#Echofirst is a MUST
6/13
⬆️⬆️⬆️ LFTs suggest ischemic hepatitis.
Low cardiac output has to be ruled out!
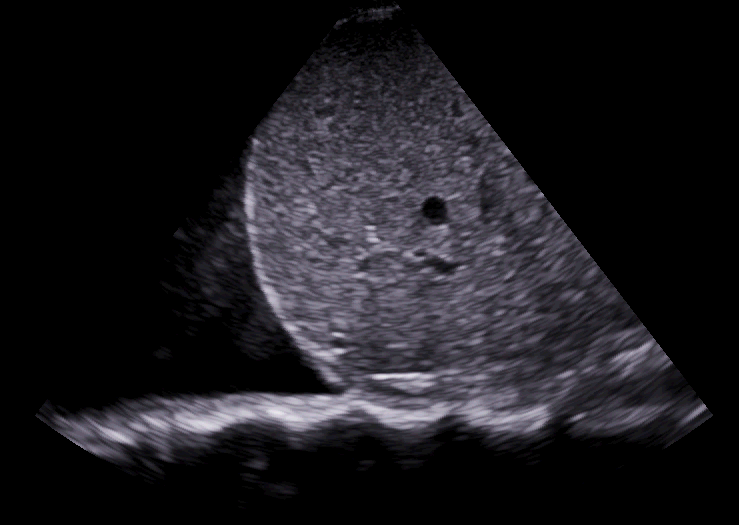
A quick look at the heart from a subxifoid window reveals a large pericardial effusion with RA collapse
Is this tamponade?
Pt has normal BP, CRT is 3 seconds, lactate is 2.9
7/13
Low cardiac output has to be ruled out!
A quick look at the heart from a subxifoid window reveals a large pericardial effusion with RA collapse
Is this tamponade?
Pt has normal BP, CRT is 3 seconds, lactate is 2.9
7/13
💡This degree of venous congestion is usually seen in severe PAH: I would expect RV failure and a very dilated RA
The combination of SEVERE venous congestion + Collapsed RA is highly suggestive of Tamponade Physiology
Advanced #POCUS skills are needed here!
#PLAx 👇
8/13
The combination of SEVERE venous congestion + Collapsed RA is highly suggestive of Tamponade Physiology
Advanced #POCUS skills are needed here!
#PLAx 👇
8/13
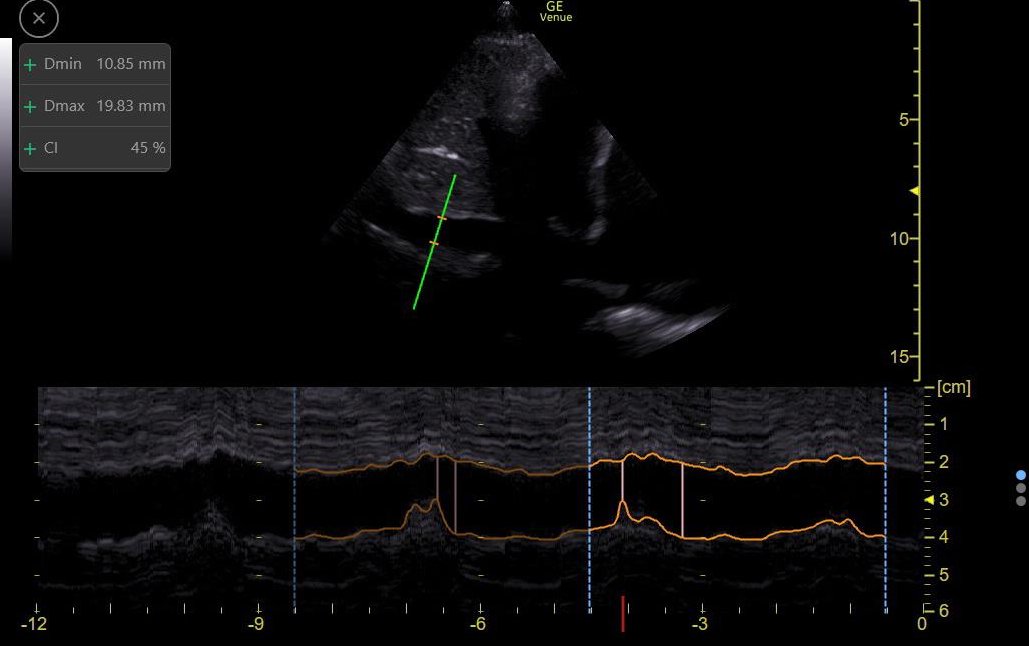
PLAx shows intermittent RV collapse,
It is sometimes hard to tell it this is happening in diastole (a sign of tamponade). So M-Mode through the Mitral Valve can help.
Here it shows clear diastolic collapse!
9/13
It is sometimes hard to tell it this is happening in diastole (a sign of tamponade). So M-Mode through the Mitral Valve can help.
Here it shows clear diastolic collapse!
9/13

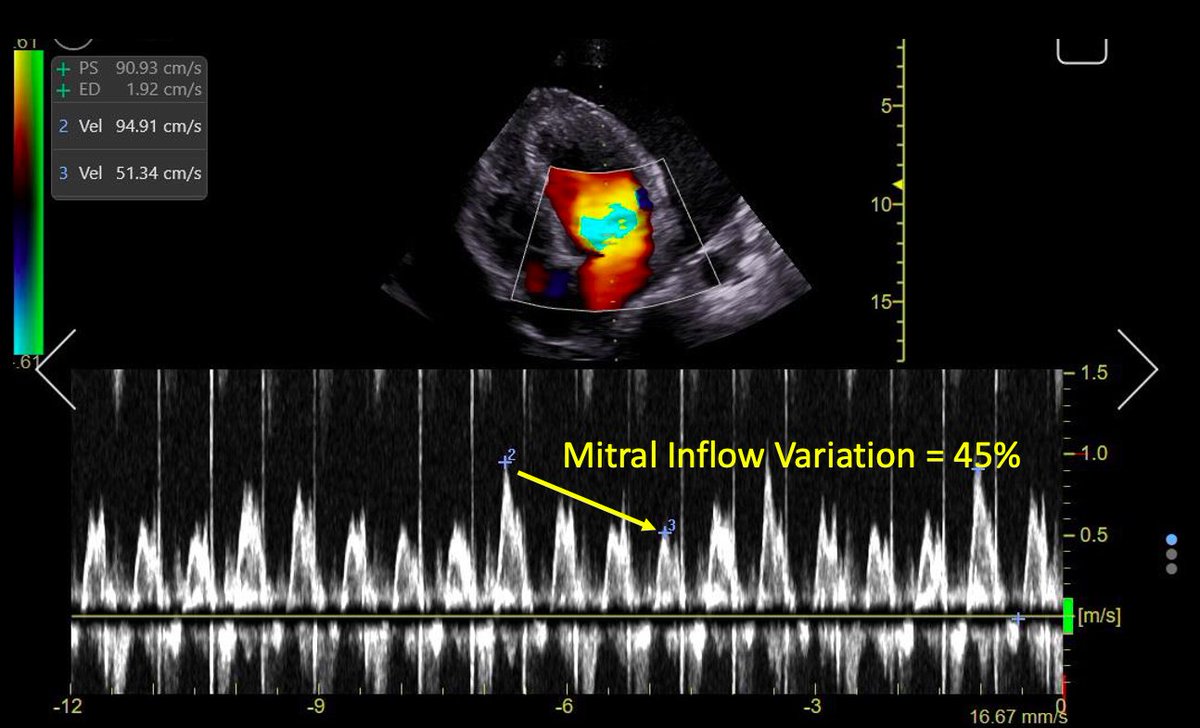
Another sign of tamponade is the equivalent of "pulsus paradoxus":
During inspiration, ⬆️ ventricular interdependence cases ⬇️ flow. So changes in flow with respiration are expected in tamponade
Trans-Mitral, Trans-Tricuspid and LVOT VTI: Significant variation!
10/13


During inspiration, ⬆️ ventricular interdependence cases ⬇️ flow. So changes in flow with respiration are expected in tamponade
Trans-Mitral, Trans-Tricuspid and LVOT VTI: Significant variation!
10/13


Tamponade Physiology is present!
Even with normal BP, the liver is suffering from significant ischemia (ALT 1166 U/L).
One could have been tempted to start ultrafiltration to decongest the liver. This has a high likelihood of precipitating cardiac arrest! 🚨
11/13
Even with normal BP, the liver is suffering from significant ischemia (ALT 1166 U/L).
One could have been tempted to start ultrafiltration to decongest the liver. This has a high likelihood of precipitating cardiac arrest! 🚨
11/13
Ultrafiltration was canceled and instead pericardiocentesis was performed!
After this procedure, no more signs of increased ventricular interdependence were present 👇
12/13


After this procedure, no more signs of increased ventricular interdependence were present 👇
12/13



Venous congestion resolved (#VExUS = 0) and LFTs normalized!
🔑Venous Congestion ≠ Hypervoemia
🔑Venous Congestion needs a DDx
🔑Tamponade causes congestion and increased ventricular interdependence
🔑Decreasing intravascular volume in pts with tamponade should be avoided
/End


🔑Venous Congestion ≠ Hypervoemia
🔑Venous Congestion needs a DDx
🔑Tamponade causes congestion and increased ventricular interdependence
🔑Decreasing intravascular volume in pts with tamponade should be avoided
/End


• • •
Missing some Tweet in this thread? You can try to
force a refresh