
Dad | Professor of Medicine @TecdeMonterrey @incmnszmx | Honorary Visiting Professor, Mayo Clinic Florida, USA and Cleveland Clinic, USA
5 subscribers
How to get URL link on X (Twitter) App




 1⃣ Intra-Renal Doppler (IRVD) alterations are usually classified using morphological patterns (Continuous, Biphasic, Monophasic)
1⃣ Intra-Renal Doppler (IRVD) alterations are usually classified using morphological patterns (Continuous, Biphasic, Monophasic)

 BP is 155/63 (MAP 94), HR 77, O2 is 94 on O2 8 L/min.
BP is 155/63 (MAP 94), HR 77, O2 is 94 on O2 8 L/min. 
 Normal HV is a mirror image of normal CVP waveform.
Normal HV is a mirror image of normal CVP waveform.



 Now 3 kg above Dry Weight.
Now 3 kg above Dry Weight. 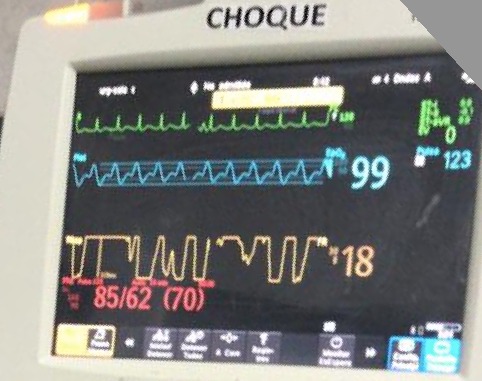
 Given DKA, giving additional fluids is tempting. But before we do this, its easy to do a quick assessment of fluid tolerance #POCUS
Given DKA, giving additional fluids is tempting. But before we do this, its easy to do a quick assessment of fluid tolerance #POCUS 





 Careful examination of neck veins reveals no pulsations, even with pt sitting up 🤔
Careful examination of neck veins reveals no pulsations, even with pt sitting up 🤔

 Cr 3.2, K 3.5, HCO3 25, Hb 8.9, WBC 26k, 95% PMN, Lactate 2.5
Cr 3.2, K 3.5, HCO3 25, Hb 8.9, WBC 26k, 95% PMN, Lactate 2.5 
 What I found remarkable was the diametrically opposed effects of manual AVF compression on JVP! 🤯
What I found remarkable was the diametrically opposed effects of manual AVF compression on JVP! 🤯

 #POCUS: Plethoric non collapsible IVC
#POCUS: Plethoric non collapsible IVC

 Which curve in the Kaplan Meier Curve above best fits this particular patient?
Which curve in the Kaplan Meier Curve above best fits this particular patient?




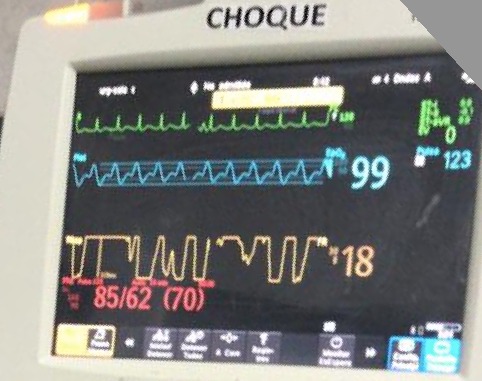
 #POCUS Very hyper-dynamic🫀 with increased contractility and no RV dysfunction.
#POCUS Very hyper-dynamic🫀 with increased contractility and no RV dysfunction. 

