🧵
Primary care follow-up for stroke patients carries many nuances and guideline recommendation updates. In this thread we outline one possible approach with 5️⃣ issues to be addressed.
#neurotwitter #stroke @OntarioCollege @ABFamDocs @CMA_Docs. cc: @draravindganesh
Primary care follow-up for stroke patients carries many nuances and guideline recommendation updates. In this thread we outline one possible approach with 5️⃣ issues to be addressed.
#neurotwitter #stroke @OntarioCollege @ABFamDocs @CMA_Docs. cc: @draravindganesh
Case:
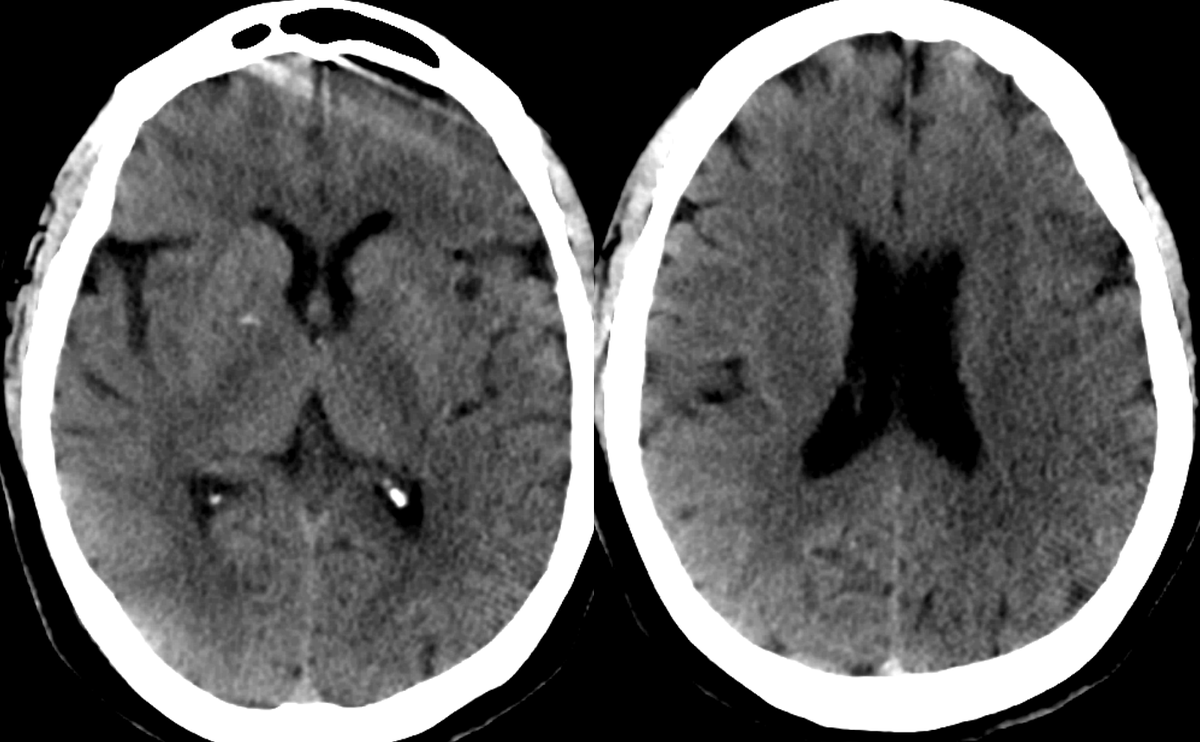
A 76F is admitted to stroke ward after suffering a L MCA stroke- undergoing thrombolysis & endovascular therapy. She makes an excellent functional recovery from her stroke and is discharged home with primary care follow up in 1-2 weeks, and specialist follow up in 3-months
A 76F is admitted to stroke ward after suffering a L MCA stroke- undergoing thrombolysis & endovascular therapy. She makes an excellent functional recovery from her stroke and is discharged home with primary care follow up in 1-2 weeks, and specialist follow up in 3-months
1⃣Review antithrombotic meds
DOACs are now preferred over warfarin for stroke prevention in Afib. Given their short 1/2 lives, compliance is extremely important as missed doses result in⬇️stroke protection. Reminders at each clinic visit is important and cost effective strategy
DOACs are now preferred over warfarin for stroke prevention in Afib. Given their short 1/2 lives, compliance is extremely important as missed doses result in⬇️stroke protection. Reminders at each clinic visit is important and cost effective strategy
2⃣ 🇨🇦guideline updates to secondary prevention optimization
More aggressive sBP target of < 130mmHg is recommended for subcortical (lacunar) strokes.
LDL target < 1.8mmol/L (rather than <2.0) in patients with symptomatic atherosclerosis which often requires add-on therapies...
More aggressive sBP target of < 130mmHg is recommended for subcortical (lacunar) strokes.
LDL target < 1.8mmol/L (rather than <2.0) in patients with symptomatic atherosclerosis which often requires add-on therapies...
if highest tolerated statin dose has not reached target. In patients with diabetes on standard oral meds not at < 7% A1c target, the addition of SGLT-2 inhibitor or GLP-1 receptor agonist is recommended. At each visit, discussion about lifestyle modification is encouraged.
3⃣ Have a guideline recommended perioperative plan for if and how long to hold antithrombotics
At each visit patients should be asked about upcoming procedures/surgeries with a plan in place regarding perioperatively dosing (see Thrombosis Canada website)...
At each visit patients should be asked about upcoming procedures/surgeries with a plan in place regarding perioperatively dosing (see Thrombosis Canada website)...
Specifically regarding dental procedures (minimal bleed risk procedure), the morning-of dose may be skipped to avoid peak anticoagulant effect during surgery with resumption 4-6 hours after procedure.
4⃣ Opportunistic screening for Afib
An update to the 2020 Canadian Stroke Best Practice Guidelines is to complete routine pulse checks or ECG at follow-up visits in individuals >65 years old after stroke.
An update to the 2020 Canadian Stroke Best Practice Guidelines is to complete routine pulse checks or ECG at follow-up visits in individuals >65 years old after stroke.
Frequent follow-up ECGs will likely result in clinically meaningful Afib detection. More invasive and prolonged cardiac monitoring may be indicated at the discretion of the stroke neurologist.
5⃣End of visit reminder when to call 🚑
Review FAST mnemonic—Face (facial droop), Arm (unilateral arm weakness), Speech (speech difficulty), & Time. Tremendous advances in acute stroke Rx (such as EVT) can reverse the effects of stroke if initiated very early after symptom onset
Review FAST mnemonic—Face (facial droop), Arm (unilateral arm weakness), Speech (speech difficulty), & Time. Tremendous advances in acute stroke Rx (such as EVT) can reverse the effects of stroke if initiated very early after symptom onset
Case cont'd:
In primary care follow-up our patient's statin was⬆️as they were tolerating without side effects the initial dose started in hospital, & indapamide 1.25mg was added to their perindopril 8mg for further BP optimization to persistently achieve a target of <130/80mmHg
In primary care follow-up our patient's statin was⬆️as they were tolerating without side effects the initial dose started in hospital, & indapamide 1.25mg was added to their perindopril 8mg for further BP optimization to persistently achieve a target of <130/80mmHg
• • •
Missing some Tweet in this thread? You can try to
force a refresh