Eurgh, I've been putting this off, because I know it's going to be grim.
Yesterday @CareQualityComm published four reports into care provided by @ASDspectrumASD in Cornwall.
All four found to be inadequate.
In this thread I'll cover some of what was found.
1/
Yesterday @CareQualityComm published four reports into care provided by @ASDspectrumASD in Cornwall.
All four found to be inadequate.
In this thread I'll cover some of what was found.
1/

Silverdale in Redruth inspected 5 May 2022 api.cqc.org.uk/public/v1/repo…
Silverdale is a residential care home providing personal care for up to four people with learning disabilities.
At the time of our inspection the service was supporting one person.
2/
Silverdale is a residential care home providing personal care for up to four people with learning disabilities.
At the time of our inspection the service was supporting one person.
2/

The service is a detached two-story property with a front garden. It is located in Redruth, Cornwall within walking distance of shops and other local facilities.
[From here my comments are in brackets, all other text is lifted from CQC report]
3/
[From here my comments are in brackets, all other text is lifted from CQC report]
3/
The service was not able to demonstrate how they were meeting the underpinning principles of Right support, right care, right culture.
[They're supporting one person]
The design and culture of the service did not maximise the person's choice, control and independence.
4/
[They're supporting one person]
The design and culture of the service did not maximise the person's choice, control and independence.
4/
Staff were planning to support the person to change the furnishings in their flat, to better reflect their tastes; but had not been able to because they could not access their own bank account.
[Always future plans]
5/
[Always future plans]
5/
The care model did not always focus on the person's strengths or identify clear paths to achieving their aspirations and goals.
The person's control over their own lives was limited which meant they did not consistently have a fulfilling and meaningful everyday life.
6/
The person's control over their own lives was limited which meant they did not consistently have a fulfilling and meaningful everyday life.
6/
The person's capacity had not always been assessed before staff made a decision on their behalf.
Staff had not all received the right training to help ensure restrictive practices were only used by staff if there was no alternative.
7/
Staff had not all received the right training to help ensure restrictive practices were only used by staff if there was no alternative.
7/
Plans to guide staff on how to support the person who experienced periods of distress were not all up to date.
Safety checks of the service had not all been completed as required.
8/
Safety checks of the service had not all been completed as required.
8/
Significant risks to the person had not been assessed and therefore control measures to protect them from abuse and poor care were not all in place.
9/
9/
The person was doing more than at the previous inspection, but this was still affected by limited access to their finances and staffing.
The service did not have enough appropriately skilled staff to meet their needs.
10/
The service did not have enough appropriately skilled staff to meet their needs.
10/
The person did not always receive support that met their needs and aspirations, focused on their quality of life and followed best practice.
The person was able to communicate with staff and understand information given to them.
11/
The person was able to communicate with staff and understand information given to them.
11/
The ethos and values in the service did not always meet best practice.
This meant the person did not always experience an inclusive and empowered life.
Staff did not always have a good understanding of best practice models of care.
12/
This meant the person did not always experience an inclusive and empowered life.
Staff did not always have a good understanding of best practice models of care.
12/
The service was based on restrictions and a punitive approach to the person's behaviour.
[Imagine. You're alone in this 4 bed house, with staff who don't know how to best support you, and you're subject to restrictions. Like a prison really]
13/
[Imagine. You're alone in this 4 bed house, with staff who don't know how to best support you, and you're subject to restrictions. Like a prison really]
13/
There was not enough management time or support by the provider to enable real development or improvement in the service.
The provider had failed to minimise the risk of a closed culture forming at the service.
14/
The provider had failed to minimise the risk of a closed culture forming at the service.
14/
The culture created in the service meant the person was not always treated as an equal.
The staff team had not been designed in a way that met the person's preferences.
Various professionals were involved in monitoring the person's care.
[Like a lab rat]
15/
The staff team had not been designed in a way that met the person's preferences.
Various professionals were involved in monitoring the person's care.
[Like a lab rat]
15/
The person was not supported to have maximum choice and control of their lives and staff did not always support them in the least restrictive way possible and in their best interests
16/
16/
The policies and systems in the service did not effectively support staff to maximise the person's choice and control.
[Despite this being one of many services that this organisation run]
17/
[Despite this being one of many services that this organisation run]
17/
The last rating for this service was requires improvement overall (published 20 August 2021), but was rated inadequate in well led.
As a result, we required the provider to report to us on a monthly basis on staffing levels, details of any gaps in staff training and...
18/
As a result, we required the provider to report to us on a monthly basis on staffing levels, details of any gaps in staff training and...
18/
...experience and the number of hours the manager was unable to complete management tasks because they were required to support the person living in the service.
We also required them to detail how they had assessed their staffing capacity for the following month.
19/
We also required them to detail how they had assessed their staffing capacity for the following month.
19/
We received these reports on a monthly basis.
At this inspection we found the provider remained in breach of regulations.
This is the third time the service will have been rated below 'good'.
[Just shut it down. Please]
20/
At this inspection we found the provider remained in breach of regulations.
This is the third time the service will have been rated below 'good'.
[Just shut it down. Please]
20/
At our last inspection we recommended the provider sought advice from a reputable source on how to support staff and ensure they understand and follow agreed guidelines.
21/
21/
At this inspection we found some guidelines were out of date; however, staff understood and were following up to date, agreed ways of working.
This inspection was carried out to follow up on action we told the provider to take at the last inspection.
22/
This inspection was carried out to follow up on action we told the provider to take at the last inspection.
22/
We have identified breaches in relation to person-centred care, the safety of the service provided, safeguarding the person from abuse, and the recruitment processes.
We also identified a breach relating to the requirement on the provider to notify us of certain events.
23/
We also identified a breach relating to the requirement on the provider to notify us of certain events.
23/
We identified continued breaches in relation to the governance of the service and staffing.
The overall rating for this service is 'Inadequate' and the service remains in 'special measures'.
24/
The overall rating for this service is 'Inadequate' and the service remains in 'special measures'.
24/
At the time of our inspection there was not a registered manager in post.
A manager who was registered to manage a different service run by the same provider was overseeing the service.
This inspection was unannounced.
25/
A manager who was registered to manage a different service run by the same provider was overseeing the service.
This inspection was unannounced.
25/
Following the site visit, we continued to request and review records. These included the person's care plan and information about how they spent their time...
We wrote two letters to the provider requesting they provide us with the person's records.
26/
We wrote two letters to the provider requesting they provide us with the person's records.
26/
[Safe - inadequate]
The person was not protected from improper care or an overly restrictive environment.
They had several restrictions placed on them but there was no clearly planned way to review or reduce these in line with good practice.
27/
The person was not protected from improper care or an overly restrictive environment.
They had several restrictions placed on them but there was no clearly planned way to review or reduce these in line with good practice.
27/
A record was in place to review restrictive practices, but it was not up to date. Some restrictions in place were not listed in the record, and others that were no longer applicable were still listed.
[Lifelong sentence once something gets written down]
28/
[Lifelong sentence once something gets written down]
28/
The record had not been used for the provider's intended purpose to prompt a review of the restrictions on the person to help ensure these were the least restrictive.
29/
29/
Staff felt some of the restrictions the person faced were no longer needed but a column entitled, 'action taken to reduce or remove restrictions' was blank for all of the restrictions listed.
[A heavily restrained and constrained non-life based on a past self]
30/
[A heavily restrained and constrained non-life based on a past self]
30/
The record had not been used to identify other restrictions that could have been reviewed to find a less restrictive option.
Staff discussed a person's locked wardrobe with us.
31/
Staff discussed a person's locked wardrobe with us.
31/
This did not appear to be the least restrictive option available for the reason given, but this had not been identified or reviewed by the provider.
[Such total apathy]
32/
[Such total apathy]
32/
The acting deputy manager told us the person now asked staff to lock their wardrobe at certain times of day.
This indicated the person had become institutionalised and used to a restrictive environment.
[Institutions, in the community. This is not a life]
33/
This indicated the person had become institutionalised and used to a restrictive environment.
[Institutions, in the community. This is not a life]
33/
Due to an ongoing, but inactive health condition, the person's access to the communal kitchen had been restricted.
This created a restrictive environment that was not adequately recorded or reviewed to ensure it was the least restrictive option on the person's movements.
34/
This created a restrictive environment that was not adequately recorded or reviewed to ensure it was the least restrictive option on the person's movements.
34/
The person's records, including their care plan still reflected the higher level of restriction, which included physical restraint, which staff said was no longer used.
[And what about agency staff? How do they respond? If it's written in someone's care plan?]
35/
[And what about agency staff? How do they respond? If it's written in someone's care plan?]
35/
This meant staff reading these records could understand that physical restraint was an option in certain circumstances rather than use less restrictive options.
36/
36/
This was of particular concern because the provider relied heavily on agency staff to support people; one of whom had not had training in how to physically restrain people safely.
[It's like I'm psychic... or anyone paying attention could predict that problem]
37/
[It's like I'm psychic... or anyone paying attention could predict that problem]
37/
The provider was responsible for the person's finances.
They had mismanaged this responsibility and therefore had not protected the person from the risk of financial abuse.
38/
They had mismanaged this responsibility and therefore had not protected the person from the risk of financial abuse.
38/
Staff who had been signatories to support the person to withdraw their money from the bank had left and no longer worked for the provider.
This meant the person could not access their money.
39/
This meant the person could not access their money.
39/
As a result, for nearly a year, they had needed to borrow money from the provider instead.
This had put them in debt to the provider.
The provider had not taken sufficient action to ensure this was resolved promptly for the person so they could access their own monies.
40/
This had put them in debt to the provider.
The provider had not taken sufficient action to ensure this was resolved promptly for the person so they could access their own monies.
40/
We requested evidence from the provider showing the trail of the person's money from when it was paid by Department of Work and Pensions (DWP), to when it was paid into the person's personal account to assess whether the person's account was credited with the full amounts.
41/
41/
We were not provided with all the information we requested.
The information shared raised concerns about the safety and adequacy of the provider's system in ensuring the person got the correct amount at the intervals it was paid by the DWP.
[Grotesque, in plain sight]
42/
The information shared raised concerns about the safety and adequacy of the provider's system in ensuring the person got the correct amount at the intervals it was paid by the DWP.
[Grotesque, in plain sight]
42/
The person had a vehicle available at the service to use.
We requested information about how this vehicle was paid for but this was not provided.
The provider shared the costs involved in the vehicle.
43/
We requested information about how this vehicle was paid for but this was not provided.
The provider shared the costs involved in the vehicle.
43/
These showed amounts for leasing the vehicle and for a tracking device used by the provider.
No further information was supplied about who met these charges or who they were paid to.
44/
No further information was supplied about who met these charges or who they were paid to.
44/
The information shared showed there was a charge for a vehicle that was not the vehicle available to them at the service.
It was difficult to identify whether the person's money had been managed safely in the service.
[This is outrageous. Financial abuse in plain sight]
45/
It was difficult to identify whether the person's money had been managed safely in the service.
[This is outrageous. Financial abuse in plain sight]
45/
At times, the person had been supported to borrow money from staff's personal money or from the service's food allowance.
Staff had not recorded these transactions clearly, which made accounting for where and how the person's money had been spent, difficult.
46/
Staff had not recorded these transactions clearly, which made accounting for where and how the person's money had been spent, difficult.
46/
Staff were responsible for supporting the person to manage their money in the service.
They had been charging the person for two staff member's bus fares when they went out but were not sure if this was the correct procedure.
47/
They had been charging the person for two staff member's bus fares when they went out but were not sure if this was the correct procedure.
47/
We requested evidence from the provider showing safe oversight and management of the person's money.
The provider did not supply all of the information requested.
[Presumably because they can't provide what they don't have]
48/
The provider did not supply all of the information requested.
[Presumably because they can't provide what they don't have]
48/
Due to a change in the national benefit system, part of the person's benefits had stopped being paid in October 2019 to be replaced with a new benefit.
The provider had not taken sufficient action to ensure the person received this benefit.
49/
The provider had not taken sufficient action to ensure the person received this benefit.
49/
Staff had completed training in safeguarding; however, an allegation of abuse raised by the person had not been reported to CQC or the local safeguarding authority as required.
We shared these concerns with the local safeguarding authority.
50/
We shared these concerns with the local safeguarding authority.
50/
This was a breach of Regulation 13 (Safeguarding service users from abuse and improper treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
51/
51/
At our last inspection we found the provider had failed to ensure staff were adequately trained and skilled to keep people safe.
This formed part of an ongoing breach of Regulation 18 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
52/
This formed part of an ongoing breach of Regulation 18 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
52/
At this inspection we found the service was still in breach of the regulation.
Two staff members had not completed all training required by the provider, to understand how to support the person if they used their behaviour as a form of communication.
53/
Two staff members had not completed all training required by the provider, to understand how to support the person if they used their behaviour as a form of communication.
53/
One of these staff members worked alone as the only member of staff awake through the night and the other staff member worked long hours at the service most weeks, which increased the need for them to be competent in using the correct approaches.
[The risk to this person]
54/
[The risk to this person]
54/
The lack of training meant the provider had not protected the person from the risk of improper use of restraint if it was needed, or ensured staff were adequately trained in person centred approaches that focused on the least restrictive options.
55/
55/
The manager overseeing the service told us the staff member was not trained because of the pandemic. They told us they had requested these staff receive the training as soon as possible.
[Reckon the pandemic will be given as reasoning to CQC for decades to come]
56/
[Reckon the pandemic will be given as reasoning to CQC for decades to come]
56/
This is a continued breach of Regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
[I've got to go feed the dog, will return in a while, if I can face it]
57/tbc
[I've got to go feed the dog, will return in a while, if I can face it]
57/tbc
Risks had not always been assessed adequately.
The service was not designed to have staff living on site, nor was it usual practice.
However, three staff members who worked for the provider were living in the service.
Two of them worked at the service but one did not.
58/
The service was not designed to have staff living on site, nor was it usual practice.
However, three staff members who worked for the provider were living in the service.
Two of them worked at the service but one did not.
58/
They had access to communal areas of the house as well as access to the area of the service where the person's private flat was.
[Whaaaaaaaaat. This is outrageous. This person's home, as digs for out of area agency staff]
59/
[Whaaaaaaaaat. This is outrageous. This person's home, as digs for out of area agency staff]
59/
The impact this might have on, or the potential risks this created for the person living at the service, had not been assessed adequately.
[I am rarely shocked reading @CareQualityComm reports, but this one is appalling]
60/
[I am rarely shocked reading @CareQualityComm reports, but this one is appalling]
60/
A risk assessment had been completed but it did not assess the impact on the person's wellbeing and the significant risk of a closed culture developing.
[Can you imagine living on your own. Staff move in. The same staff who provide you support. You can never escape them]
61/
[Can you imagine living on your own. Staff move in. The same staff who provide you support. You can never escape them]
61/
It did not include detail of how the provider had assured themselves the three staff were safe to live with a vulnerable adult.
Two staff members were providing the majority of support hours to the person.
This meant they were working an unsafe number of hours.
62/
Two staff members were providing the majority of support hours to the person.
This meant they were working an unsafe number of hours.
62/
A risk assessment that was regularly reviewed, stated they would work a maximum of 84 hours a week with one full day off per week (that is no day, sleeping or waking night shift); however both staff members had exceeded this amount in March and April 2022.
[So dangerous]
63/
[So dangerous]
63/
One staff member had worked 22 out of 24 days between the 28 March and 20 April 2022.
This was mostly 14 hour shifts during the day but also included 'sleep in' shifts and shifts when they were required to be awake all night.
64/
This was mostly 14 hour shifts during the day but also included 'sleep in' shifts and shifts when they were required to be awake all night.
64/
The second staff member also regularly worked more than 6 days in a row without a full day off.
Between the 17 March and 14 April 2022, they worked 28 days with only one full day off.
[These are almost certainly the same staff who haven't been provided adequate training]
65/
Between the 17 March and 14 April 2022, they worked 28 days with only one full day off.
[These are almost certainly the same staff who haven't been provided adequate training]
65/
Working these excessive hours with limited opportunities for rest exposed both the staff member and the person they supported to significant risk of harm.
66/
66/
The risk assessment noted a risk to the agency workers of working long hours and having no break from the service, but did not assess the risk to person of being supported by staff who worked long hours and didn't have a regular opportunity to have a break from the service.
67/
67/
The staff members were employed at the service via a staffing agency.
They were working for the provider long term, living in the service and completing long hours each week...
68/
They were working for the provider long term, living in the service and completing long hours each week...
68/
...however, the provider had not taken all steps to assure themselves the staff were safe to work and live with vulnerable adults.
[It's almost like the people don't really count.
So care-less]
69/
[It's almost like the people don't really count.
So care-less]
69/
Checks to ensure the service met relevant health and safety standards had not been completed consistently, or prompt action taken when faults occurred.
Regular testing of the fire alarm had been raised as a concern in 2018.
70/
Regular testing of the fire alarm had been raised as a concern in 2018.
70/
Some improvements had been made but a check of records in October 2021 showed it was still not being tested frequently enough.
An audit in February 2022 also highlighted that alarm tests were not regularly carried out and documented.
[Performative scrutiny]
71/
An audit in February 2022 also highlighted that alarm tests were not regularly carried out and documented.
[Performative scrutiny]
71/
At the inspection the frequency had increased but this was still not in line with the provider's policy.
A record showing testing of emergency lighting in the service showed the emergency light in the dining room wasn't working on 16 October 2021.
72/
A record showing testing of emergency lighting in the service showed the emergency light in the dining room wasn't working on 16 October 2021.
72/
An entry on 16 November 2021 reported, 'a few' lights weren't working.
The record did not show all lights working consistently until 4 February 2022.
This demonstrated that environmental risks were not addressed in a timely fashion to keep people safe.
73/
The record did not show all lights working consistently until 4 February 2022.
This demonstrated that environmental risks were not addressed in a timely fashion to keep people safe.
73/
Action had not been taken when water temperatures fell outside the limits stated in the provider's guidance on the relevant record.
This showed the provider was not ensuring staff were acting promptly to protect people from the risk of harm.
74/
This showed the provider was not ensuring staff were acting promptly to protect people from the risk of harm.
74/
This is a breach of Regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
75/
75/
At our last inspection we found an ongoing breach of regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014, due to the service being short staffed.
76/
76/
At this inspection we found the service was still understaffed.
The person's commissioned number of support hours were met in the unsafe manner described above.
Further, the provider had not deployed sufficient staff to meet the person's preferences.
[One person]
77/
The person's commissioned number of support hours were met in the unsafe manner described above.
Further, the provider had not deployed sufficient staff to meet the person's preferences.
[One person]
77/
Staff had identified the person benefited from being supported by a range of staff, rather than seeing the same staff all the time.
Due to staff shortages, the staff rota could not be designed to suit these preferences
78/
Due to staff shortages, the staff rota could not be designed to suit these preferences
78/
The service was short of two full time and two part time staff, so the majority of shifts were filled by the same two staff members.
The manager overseeing the service used staff from other services when gaps in the rota needed to be filled to help meet this preference.
79/
The manager overseeing the service used staff from other services when gaps in the rota needed to be filled to help meet this preference.
79/
However, overall the rota showed that the person's preference for variety was not taken seriously or plans put in place to help ensure it was consistently met.
[Not taken seriously. Your own support. Your own home. Your own life. Nah, it's all about the provider]
80/
[Not taken seriously. Your own support. Your own home. Your own life. Nah, it's all about the provider]
80/
The person had their own vehicle to use but there was a lack of staff who were able to drive it.
A staff member and a professional described this as a shortfall at the service.
81/
A staff member and a professional described this as a shortfall at the service.
81/
The person enjoyed travelling by public transport, but the lack of drivers meant that when the person wanted or needed to use their vehicle, this was not always possible.
82/
82/
This is a continued breach of Regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
83/
83/
Approaches to staff recruitment did not demonstrate a strong focus on quality.
The recruitment information that was supplied showed that some checks had been completed after one staff member started working at the service.
84/
The recruitment information that was supplied showed that some checks had been completed after one staff member started working at the service.
84/
The provider had relied on a staffing agency to complete recruitment checks for some staff.
The employment agency had not sought a full employment history, as required by the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
85/
The employment agency had not sought a full employment history, as required by the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
85/
The provider had not queried or acted on this omission.
[The provider hasn't really taken their duties and responsibilities very seriously at all have they?]
86/
[The provider hasn't really taken their duties and responsibilities very seriously at all have they?]
86/
A staff member who lived at the location but worked at another of the provider's services had a DBS check that did not show the same place of birth as their passport and was not completed by the staffing agency.
The provider had not queried or acted upon this concern.
87/
The provider had not queried or acted upon this concern.
87/
This is a breach of Regulation 19 (Fit and proper persons employed) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
88/
88/
The manager overseeing the service and the acting deputy took action where possible to improve aspects of the service when things went wrong.
89/
89/
However, the lack of management time in the service meant it was difficult for them to ensure they were identifying all areas where things had gone wrong.
They also had limited time to check lessons had been learned and improvements implemented effectively.
90/
They also had limited time to check lessons had been learned and improvements implemented effectively.
90/
Records showed that deep cleaning tasks had not been completed as frequently as allocated.
Some weekly tasks had not been recorded as completed since March 2022.
The manager overseeing the service was aware of this.
91/
Some weekly tasks had not been recorded as completed since March 2022.
The manager overseeing the service was aware of this.
91/
They and the acting deputy manager were putting steps in place to ensure this was rectified.
[Always putting in place, always future plans, meanwhile people exist in these sub-standard non-lives]
92/
[Always putting in place, always future plans, meanwhile people exist in these sub-standard non-lives]
92/
[Effective - requires improvement]
Strategies used to support the person to feel or remain calm did not reflect best practice.
The person had a reward chart in place.
[Like puppy training... except this is an adult, in their own home. Reward charts]
93/
Strategies used to support the person to feel or remain calm did not reflect best practice.
The person had a reward chart in place.
[Like puppy training... except this is an adult, in their own home. Reward charts]
93/
Guidance stated, if [person] 'behaved' well all week, [they] would get a reward.
It also explained, "If [person] gets 3 crosses in the week they don't get a good [person] reward, which is usually on a Saturday."
[NOOOOOO]
94/
It also explained, "If [person] gets 3 crosses in the week they don't get a good [person] reward, which is usually on a Saturday."
[NOOOOOO]
94/
This was a punitive approach which is not in line with best practice.
Staff and professionals told us they thought the person benefited from the approach, but it had not been reviewed to establish whether this was still the best option for them.
95/
Staff and professionals told us they thought the person benefited from the approach, but it had not been reviewed to establish whether this was still the best option for them.
95/
This is part of a breach of Regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
96/
96/
The person was at risk of weight loss but also of high cholesterol, there was no guidance for staff about how to ensure the person's diet helped reduce both these risks.
Following a GP visit in 2019, staff had been asked to monitor the amount of fatty foods the person ate.
97/
Following a GP visit in 2019, staff had been asked to monitor the amount of fatty foods the person ate.
97/
Staff recorded what the person ate but there was no evidence of monitoring the food's nutritional value.
This formed part of a breach of Regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
98/
This formed part of a breach of Regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
98/
Staff told us they thought the environment was suitable for the person but needed updating.
One staff member told us, "[Person] needs new things in there. They could do with making it brighter and more homely, it's a bit dowdy."
99/
One staff member told us, "[Person] needs new things in there. They could do with making it brighter and more homely, it's a bit dowdy."
99/
Due to ongoing problems accessing the person's money, no further action had been taken to improve the environment.
The person had a shed in the garden which they used to relax in. They had decorated it according to their tastes.
100/
The person had a shed in the garden which they used to relax in. They had decorated it according to their tastes.
100/
The provider had not ensured staff had completed all relevant training.
Only one staff member had completed training in person centred care and equality and diversity.
This contributed to the poor culture of the service.
101/
Only one staff member had completed training in person centred care and equality and diversity.
This contributed to the poor culture of the service.
101/
Staff from a nearby service supported the person at times, there was no evidence they had been inducted into the service or the person's needs.
102/
102/
We were told agency staff had completed shadow shifts with the person when they first started but there was no record of these either.
Following inspection, the manager overseeing the service told us they would ensure these records were in place in the future.
[Future]
103/
Following inspection, the manager overseeing the service told us they would ensure these records were in place in the future.
[Future]
103/
The acting deputy manager told us they were providing staff with a specific policy each week which they then discussed to help ensure understanding.
They had also started providing staff with regular one to one supervision sessions.
[Basics]
104/
They had also started providing staff with regular one to one supervision sessions.
[Basics]
104/
Person was unable to understand and consent to content of their care plan.
A best interests decision had been made in conjunction with people who knew person well, that involving them in reviews of their care wld create undue stress.
[But their preferences were ignored]
105/
A best interests decision had been made in conjunction with people who knew person well, that involving them in reviews of their care wld create undue stress.
[But their preferences were ignored]
105/
[Caring - requires improvement]
Language used in the person's records was not always appropriate for the person's age.
For example, one record described how to react if the person was 'naughty' or 'good.'
[An adult]
106/
Language used in the person's records was not always appropriate for the person's age.
For example, one record described how to react if the person was 'naughty' or 'good.'
[An adult]
106/
Staff often described the person as having been 'good' or 'well behaved' in their records.
In addition, they did not describe activities in a way that suggested the person was an equal but instead suggested an imbalance of power in favour of staff and the service.
107/
In addition, they did not describe activities in a way that suggested the person was an equal but instead suggested an imbalance of power in favour of staff and the service.
107/
For example, daily records included,
"[Person] asked staff for a cigarette and was taken to his shade [outside]" and "[Staff] walked [person] to Darren's Chippy".
[Taken to... walked to... is the person a dog or a human?]
108/
"[Person] asked staff for a cigarette and was taken to his shade [outside]" and "[Staff] walked [person] to Darren's Chippy".
[Taken to... walked to... is the person a dog or a human?]
108/
Staff encouraged the person to be involved in household tasks, which helped maintain their independence; however, there was no clear aim or guidance for staff to follow to increase the person's skills or independence.
109/
109/
This meant it was difficult for them to increase their skills and independence.
A staff member who did not work at the service was living there.
They had access to the same communal areas as the person.
110/
A staff member who did not work at the service was living there.
They had access to the same communal areas as the person.
110/
They had worked with the person before and so understood their needs; however, due to their proximity to the person, it was possible they could become aware of changes to the person's needs or preferences.
111/
111/
This had not been assessed as a risk to the person's privacy or confidential information.
[This is all so not ok]
112/
[This is all so not ok]
112/
[Responsive - requires improvement]
At our last inspection we recommended the provider sought advice from a reputable source on how to support staff and ensure they understand and follow agreed guidelines.
113/
At our last inspection we recommended the provider sought advice from a reputable source on how to support staff and ensure they understand and follow agreed guidelines.
113/
At this inspection we found some guidelines were out of date; however, staff were aware of and following up to date, agreed ways of working.
The provider's approach to staffing had not enabled the service to operate in a way that met the person's preferences.
114/
The provider's approach to staffing had not enabled the service to operate in a way that met the person's preferences.
114/
Staff had identified the person benefitted from being supported by a variety of staff.
They had found creative ways to provide this at times and improve the person's wellbeing, but were unable to consistently provide variety.
115/
They had found creative ways to provide this at times and improve the person's wellbeing, but were unable to consistently provide variety.
115/
Due to a lack of management and provider oversight, records about the person's needs and wishes had not all been kept up to date.
The person's care plan did not reflect best practice.
116/
The person's care plan did not reflect best practice.
116/
It was not strengths-based and there was little information about person's future goals and aspirations, or evidence of skills teaching.
This is a breach of Regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
117/
This is a breach of Regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
117/
At our last inspection we found the provider had failed to ensure enough staff were available to enable people to engage with activities and access the community.
This was part of a continued breach of Regulation 18 of the Health and Social Care Act 2008
118/
This was part of a continued breach of Regulation 18 of the Health and Social Care Act 2008
118/
At this inspection we found some improvements but failings by the provider were still impacting on the person's quality of life.
Staffing impacted on the how the person spent their time.
119/
Staffing impacted on the how the person spent their time.
119/
A record describing what options the person should be given each day stated,
'If [person] goes out for the day he is given a choice of two places, depending on drivers, money and handover times etc.'
[Wow]
120/
'If [person] goes out for the day he is given a choice of two places, depending on drivers, money and handover times etc.'
[Wow]
120/
What the person could do and how they could spend their time had been limited as staff could not access the person's bank account on their behalf.
Instead, they were borrowing money from the provider.
121/
Instead, they were borrowing money from the provider.
121/
They had been supported by staff to create a list of things they would like to do but staff had not been given clear guidance about the person's income and therefore how much they could spend.
122/
122/
As a result, the person was not given enough money as staff limited their access because they were cautious about getting the person into debt.
Therefore, the provider had not supported them to meet all their wishes for how they spent their time.
123/
Therefore, the provider had not supported them to meet all their wishes for how they spent their time.
123/
This is a breach of Regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
124/
124/
[Well-led - inadequate]
Failings by the provider meant the design and culture of the service did not meet best practice and was not consistently achieving good outcomes for the person.
125/
Failings by the provider meant the design and culture of the service did not meet best practice and was not consistently achieving good outcomes for the person.
125/
The provider had failed to ensure the person had ongoing access to their money.
This had impacted on how they could spend their time and their ability to achieve their wishes.
126/
This had impacted on how they could spend their time and their ability to achieve their wishes.
126/
The provider had not acted as a strong advocate for the person to ensure they were receiving the benefits they were entitled to.
The way staff spoke about and treated the person demonstrated an infantilising culture within the service.
127/
The way staff spoke about and treated the person demonstrated an infantilising culture within the service.
127/
For example, when the person had not become anxious during the day, staff gave them 'good [person] ticks'.
Staff reported the person would then get
"A weekly treat. Maybe to go in the bigger garden and play with the things out there; or have a movie day and treats."
128/
Staff reported the person would then get
"A weekly treat. Maybe to go in the bigger garden and play with the things out there; or have a movie day and treats."
128/
This did not show they were treating the person as an adult.
These failings contributed to a breach of Regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
129/
These failings contributed to a breach of Regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
129/
At our last inspection, we found the provider's systems and processes for ensuring compliance with the regulations were ineffective and action plans developed in response to previous breaches had proven inadequate to provide adequate staffing at Silverdale.
130/
130/
This was a breach of regulation 17 (Good governance) of The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
At this inspection we found the same concerns.
131/
At this inspection we found the same concerns.
131/
There was limited evidence of the provider's motivation to continually drive improvement at Silverdale.
Despite the last inspection report raising concerns in August 2022 [2021?], no provider level audit was completed of the service until February 2022.
132/
Despite the last inspection report raising concerns in August 2022 [2021?], no provider level audit was completed of the service until February 2022.
132/
This was a basic audit and had not produced a detailed action plan to help guide the manager overseeing the service about how to improve care delivery.
[Pointless performative scrutiny, with no intention to it]
133/
[Pointless performative scrutiny, with no intention to it]
133/
Our last report stated the service and provider exhibited many of the risk factors and warning signs associated with closed cultures.
Risk factors included people's high level of dependence, their complete reliance on staff for their basic needs and access to community.
134/
Risk factors included people's high level of dependence, their complete reliance on staff for their basic needs and access to community.
134/
The warning signs included but were not limited to, staff working excessively long hours, consistent staff shortages and the lack of effective oversight by the provider.
135/
135/
At this inspection we found the provider had failed to take the concerns seriously or reduce the risk to the person.
The service was still short staffed and was relying on two staff to fill most of the hours on the rota.
[Total apathy]
136/
The service was still short staffed and was relying on two staff to fill most of the hours on the rota.
[Total apathy]
136/
At times these staff had worked 98 hours per week and completed sleep in shifts in addition.
This left the person at high risk of being impacted negatively by a closed culture within the service.
137/
This left the person at high risk of being impacted negatively by a closed culture within the service.
137/
The manager overseeing the service was aware of this risk and had recorded that further recruitment was needed; however the provider had not assessed the risk or taken action to mitigate it.
138/
138/
A professional raised concerns that problems with staff not being able to support the person to access their bank account had happened before.
This showed insufficient learning and safeguards had been put in place to stop it happening again.
139/
This showed insufficient learning and safeguards had been put in place to stop it happening again.
139/
Areas of the service where the manager overseeing the service and the acting deputy manager had tried to implement improvements, had not always been sustained as they did not have the capacity to complete regular checks.
140/
140/
For example, they had requested staff improve completion of a daily staff communication and handover book.
However, it had only been completed on two mornings in the first five days of May 2022.
[Culture of complete apathy]
141/
However, it had only been completed on two mornings in the first five days of May 2022.
[Culture of complete apathy]
141/
The commission has completed a programme of inspections of all Spectrum services, including Silverdale, since May 2021.
At the majority of these inspections we identified staffing and oversight concerns.
142/
At the majority of these inspections we identified staffing and oversight concerns.
142/
This is a continued breach of Regulation 17 (Good governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
143/
143/
The provider had not ensured there was adequate leadership or oversight of the service.
Professionals raised concerns about the inconsistency in leadership at the service.
144/
Professionals raised concerns about the inconsistency in leadership at the service.
144/
They told us there had been frequent changes which meant that agreed tasks had not always been followed through.
145/
145/
They reported that the consistency of the staff team and management at the service was better but that they did not have confidence it had been completely rectified or would be maintained in the long term.
146/
146/
The manager who was overseeing the service was also the registered manager of another service, and due to short staffing was sometimes required to work on shift, at Silverdale or at the service where they were registered, this included sleep in shifts and waking nights.
147/
147/
This meant their time operating as a manager at Silverdale was limited.
Professionals told us they thought the manager overseeing the service was stressed and overwhelmed by this workload.
[This is so unsustainable]
148/
Professionals told us they thought the manager overseeing the service was stressed and overwhelmed by this workload.
[This is so unsustainable]
148/
The acting deputy had just stepped into the role and was keen to make changes but had little experience of management roles and responsibilities.
They were learning the role from the manager overseeing the service.
149/
They were learning the role from the manager overseeing the service.
149/
However, they also spent time on shift, so their time together was limited.
A staff member told us they thought the acting deputy manager needed more support.
150/
A staff member told us they thought the acting deputy manager needed more support.
150/
The provider's processes and procedures had not ensured the required improvements at the service were identified or acted on.
The manager overseeing the service had not received sufficient support from the provider to ensure the service improved.
151/
The manager overseeing the service had not received sufficient support from the provider to ensure the service improved.
151/
They had received no action plan and no regular meetings to discuss improvements required.
The manager overseeing the service and acting deputy manager were aware of some of the areas of the service needing action but had not had the time or support to make improvements.
152/
The manager overseeing the service and acting deputy manager were aware of some of the areas of the service needing action but had not had the time or support to make improvements.
152/
As a result, several records relating to the person and the service were out of date.
Records did not always reflect the person's current needs and relevant monitoring and checks of the service had not all been consistently completed.
153/
Records did not always reflect the person's current needs and relevant monitoring and checks of the service had not all been consistently completed.
153/
An effective system had not been established to prevent abuse.
The lack of management time in the service meant important tasks, like reporting allegations of abuse, had been overlooked.
154/
The lack of management time in the service meant important tasks, like reporting allegations of abuse, had been overlooked.
154/
The provider had not taken adequate action to ensure the person was safeguarded from the risk of financial abuse.
155/
155/
They were responsible for the management and oversight of the person's finances but had not taken sufficient action to ensure the person had ongoing access to the correct benefits, or their bank account.
156/
156/
They had not taken prompt action to reinstate the person's access to these when problems arose.
The provider had not understood or fulfilled their responsibilities to ensure staff who worked and lived in the service, were safe to do so.
157/
The provider had not understood or fulfilled their responsibilities to ensure staff who worked and lived in the service, were safe to do so.
157/
This is a continued breach of Regulation 17 (Good governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
158/
158/
The service had not raised a safeguarding alert to the local authority safeguarding team or notified the CQC that the person was at risk of financial abuse and/or mismanagement.
159/
159/
They had not raised a safeguarding alert following an allegation the person made against a staff member.
The failure to submit necessary notification to the commission is a breach of Regulation 18 (Notification of other incidents) of the CQC (Registration) Regulations 2009
160/
The failure to submit necessary notification to the commission is a breach of Regulation 18 (Notification of other incidents) of the CQC (Registration) Regulations 2009
160/
We requested information from the provider to assure us of the safety of their systems around managing the person's finances.
These were not all provided.
161/
These were not all provided.
161/
There was no evidence that staff or the provider had helped the person understand the difficulties accessing their money and benefits; or the impact that it was having on their financial status.
162/
162/
This contributes to the continued breach of Regulation 17 (Good governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
163/
163/
[That's all for Silverdale. There's no enforcement action listed but I'm sure it will be updated in due course. I'll try to keep you posted.
Will get to the other reports over the weekend. Will continue them on this thread, but I need a break now]
164/tbc
Will get to the other reports over the weekend. Will continue them on this thread, but I need a break now]
164/tbc
Trelawney House api.cqc.org.uk/public/v1/repo…
Trelawney House is a residential care home providing personal care for up to six people with a learning disability and/or autistic people.
Five people were living in the service at the time of this inspection.
165/
Trelawney House is a residential care home providing personal care for up to six people with a learning disability and/or autistic people.
Five people were living in the service at the time of this inspection.
165/

It is part of the Spectrum (Devon and Cornwall Autistic Community Trust) group, a provider with 15 other similar services for adults across Cornwall.
166/
166/
Trelawney House is in a rural location. The nearest town is Helston which is approximately four miles away without public transport links.
People, relatives and staff all reported improvements in the service's performance since the last inspection.
167/
People, relatives and staff all reported improvements in the service's performance since the last inspection.
167/
The service was not able to demonstrate how they were meeting some of the underpinning principles of the statutory guidance Right Support, Right Care, Right Culture.
168/
168/
The service remained short staffed and low staffing levels continued to restrict people's freedoms and choices.
The provider had not safely managed risks in relation to the quality of care provided by tired staff.
169/
The provider had not safely managed risks in relation to the quality of care provided by tired staff.
169/
Staffing numbers on shift each day had improved and there were no incidents where staffing numbers had been unsafe in the month prior to our inspection.
170/
170/
However, people's needs in relation to staffing were not fully met and reduced staffing levels continued to restrict freedoms and choices.
The provider had not ensured all necessary recruitment checks had been completed for agency staff working in the service.
171/
The provider had not ensured all necessary recruitment checks had been completed for agency staff working in the service.
171/
We identified issues in relation to the use of personal protective equipment by some staff who were not wearing masks, this was reported to the manager and resolved.
172/
172/
Improvements had been made to some aspects of the service's environment and soiled carpeting had been replaced.
[How grim does this place sound like it was on the last inspection]
173/
[How grim does this place sound like it was on the last inspection]
173/
However, faulty emergency lighting had not been promptly repaired, a number of double glassed window required replacement and an area of damp was present in one person's bedroom.
174/
174/
People were now protected from abuse at Trelawney House and no one was locked in their own rooms during this inspection.
[Eurgh, seriously, I can't face going back to the last report but its on the @CareQualityComm website if you'd like to]
175/
[Eurgh, seriously, I can't face going back to the last report but its on the @CareQualityComm website if you'd like to]
175/
People told us they now felt safe in the service and no one had alleged incidents of abuse occurring in the service since the last inspection.
The new manager understood how to report safeguarding concerns.
176/
The new manager understood how to report safeguarding concerns.
176/
People's care plans were lengthy, and protocols used by staff did not consistently reflect guidance contained in care plans.
This was raised with the manager on the first day and resolved by the second visit to the service during this inspection.
177/
This was raised with the manager on the first day and resolved by the second visit to the service during this inspection.
177/
Issues in relation to the noise levels in the service during the day and at night had improved.
People were more relaxed in the home and were now able to rest.
This had impacted positively on their wellbeing.
178/
People were more relaxed in the home and were now able to rest.
This had impacted positively on their wellbeing.
178/
The person who had become withdrawn as a result of high noise levels were now comfortable accessing the service's communal areas.
People now had more control of their lives and this had positively impacted on their wellbeing.
179/
People now had more control of their lives and this had positively impacted on their wellbeing.
179/
Access to the community had improved and people were now regularly supported to engage in a variety of activities they enjoyed.
Risks in relation to people's mobility were now managed appropriately. A person whose mobility was declining had moved into a ground floor flat.
180/
Risks in relation to people's mobility were now managed appropriately. A person whose mobility was declining had moved into a ground floor flat.
180/
They were now able to access the service's communal areas and their bedroom independently when they wished.
Appropriate support was provided to ensure the person's dignity was protected while accessing vehicles.
181/
Appropriate support was provided to ensure the person's dignity was protected while accessing vehicles.
181/
People were appropriately supported at mealtime and staff had the skills they needed to meet people needs. Medicines were managed safely.
However, we have made a recommendation in relation to systems for administering as required medications.
182/
However, we have made a recommendation in relation to systems for administering as required medications.
182/
The culture of the service had significantly improved.
Staff were well motivated and focused on supporting and enabling people to have choice and control over their lives.
183/
Staff were well motivated and focused on supporting and enabling people to have choice and control over their lives.
183/
The manager was open and honest throughout the inspection and information request was provided promptly.
184/
184/
People were not always supported to have maximum choice and control of their lives and the service had not fully complied with reporting conditions made under the Deprivation of Liberty Safeguards.
185/
185/
MCA assessments and best interest decisions remained generic rather than decision specific.
There was no registered manager in post.
A new manager had been recruited since the last inspection.
186/
There was no registered manager in post.
A new manager had been recruited since the last inspection.
186/
Staff and relatives were highly complementary of the manager's approach and professionals told us communication with the service had improved.
187/
187/
The provider's quality assurance systems had failed to ensure the service complied with the regulations.
The manager had reintroduced the use of paper based daily care records as the provider's digital recording system was ineffective.
188/
The manager had reintroduced the use of paper based daily care records as the provider's digital recording system was ineffective.
188/
Incident recording had improved, and the manager had reviewed incident records to identify possible areas of learning or improvement.
189/
189/
Senior staff had begun additional training to support people to communicate effectively.
Staff were now able to communicate effectively with people which enabled people to have more control over their lives.
190/
Staff were now able to communicate effectively with people which enabled people to have more control over their lives.
190/
The last rating for this service was Inadequate (published 16 December 2021) and there were breaches of regulation.
At this inspection we found some improvements had been made. However, the service's rating remains inadequate.
191/
At this inspection we found some improvements had been made. However, the service's rating remains inadequate.
191/
A number on ongoing breaches of the regulations were identified at the inspection.
We have identified breaches in relation to need for consent, premises and equipment, governance, staffing and fit and proper persons employed at this inspection.
192/
We have identified breaches in relation to need for consent, premises and equipment, governance, staffing and fit and proper persons employed at this inspection.
192/
[Safe - inadequate]
At this inspection we found the provider did not have robust systems in place to ensure all staff deployed in the service were suitable for employment in the care sector.
193/
At this inspection we found the provider did not have robust systems in place to ensure all staff deployed in the service were suitable for employment in the care sector.
193/
Following the last inspection, the commission made a safeguarding alert about an incident of alleged abused involving a member of agency staff.
194/
194/
Other bodies attempted to investigate this matter but were unable to establish the identity of the alleged abuser employed by the agency. This information had been shared with the provider prior to this inspection.
195/
195/
We requested the recruitment information for all five members of agency staff working at Trelawney House.
Information provided lacked full employment histories and included references from previous employers where dates did not match available staff employment histories.
196/
Information provided lacked full employment histories and included references from previous employers where dates did not match available staff employment histories.
196/
In addition, Disclosure and Barring Service (DBS) checks had not been completed by the agency for four of the five staff currently working at and living in the grounds of Trelawney House.
[Living in the grounds of... again]
197/
[Living in the grounds of... again]
197/
The Agencies recruitment procedures were unsafe and the provider had not learnt from the previous incident involving unsafe recruitment practices.
The provider had failed to ensure all staff working in the service were fit and proper persons.
198/
The provider had failed to ensure all staff working in the service were fit and proper persons.
198/
This meant the provider was in breach of the requirements of Regulation 19 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
199/
199/
At our last inspection we found there were insufficient staff available to meet people's support needs.
This was a breach of the requirements of Regulation 18 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
200/
This was a breach of the requirements of Regulation 18 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
200/
At this inspection although staffing level had improved there were still not enough staff available to fully meet people's support needs.
This meant the service remained in breach of the regulations.
201/
This meant the service remained in breach of the regulations.
201/
The provider continued to experience significant challenges in relation to recruitment.
In response to ongoing staff shortages, pay had been increased and previously withdrawn benefits reintroduced with the aim of making the provider more attractive to prospective staff.
202/
In response to ongoing staff shortages, pay had been increased and previously withdrawn benefits reintroduced with the aim of making the provider more attractive to prospective staff.
202/
However, this had so far been ineffective. Relatives said, "They don't seem to be recruiting any permanent staff".
[Who would want to work for this provider. A quick visit to @CareQualityComm website shows you the state they're in. Why would you? There's no leadership]
203/
[Who would want to work for this provider. A quick visit to @CareQualityComm website shows you the state they're in. Why would you? There's no leadership]
203/
At the time of our last inspection the provider had identified that a minimum of five staff were required to ensure the safety of people living in Trelawney house.
204/
204/
Since that inspection one person had moved out and at this inspection the provider's minimum safe staffing levels were four staff during the day and one waking and two sleeping staff at night.
205/
205/
We reviewed staffing levels in the month prior to our inspection and found the service had not operated below these minimum safe staffing levels. However, they regularly fell below the levels identified as necessary to support people to live full and meaningful lives.
206/
206/
[How is this statement even possible. I don't get it.
Surely the safe staffing levels *are* the staffing levels required for people to have full and meaningful lives...
otherwise safe staffing = containment, which is not a life]
207/
Surely the safe staffing levels *are* the staffing levels required for people to have full and meaningful lives...
otherwise safe staffing = containment, which is not a life]
207/
The provider had identified that six staff members were required each day to enable people to engage with activities and access the community when they wished.
Records showed these planned levels of support were infrequently provided.
[This is not a life]
208/
Records showed these planned levels of support were infrequently provided.
[This is not a life]
208/
One person normally attended a day centre on weekdays, and this meant increased staffing levels were needed to meet people's needs at the weekend.
However, rotas and staff allocations showed the service tended to have less staff available at the weekend.
209/
However, rotas and staff allocations showed the service tended to have less staff available at the weekend.
209/
This meant people's choices and freedoms in relation to activities were more likely to be restricted at these times.
[What are the lives of the people in Trelawney House like this weekend? What activities are they getting up to? What choices do they have?]
210/
[What are the lives of the people in Trelawney House like this weekend? What activities are they getting up to? What choices do they have?]
210/
Staff told us,
"We say it should be six [Staff] in the morning and five in the afternoon as [person's name] staff member comes over when [they are at the day centre], when not at the Day centre we need seven but we are not there with that".
211/
"We say it should be six [Staff] in the morning and five in the afternoon as [person's name] staff member comes over when [they are at the day centre], when not at the Day centre we need seven but we are not there with that".
211/
The manager recognised further increases in staffing levels were necessary to fully meet people's support needs and enable them to access the community whenever they wished.
212/
212/
The manager's comments included, "Staffing is better, not perfect. I could still do with some more, it is very difficult to recruit to this house because of where it is."
[Which shouldn't really surprise anyone, because it's in the middle of nowhere]
213/
[Which shouldn't really surprise anyone, because it's in the middle of nowhere]
213/
Although people were receiving more hours of care the provider had not deployed staff to do so in a safe way.
Agency staff working at Trelawney House were working excessive hours each week.
[Course they were, cos there's nothing else to do out there]
214/
Agency staff working at Trelawney House were working excessive hours each week.
[Course they were, cos there's nothing else to do out there]
214/
Rotas showed these staff were routinely completing six 14 hour shifts each week with one day off.
Where staff intended to work more than 70 hours a week a risk assessment had been completed by the manager.
[Performative scrutiny - meaningless risk assessments]
215/
Where staff intended to work more than 70 hours a week a risk assessment had been completed by the manager.
[Performative scrutiny - meaningless risk assessments]
215/
These risk assessments did not recognise the potential impact of long working hours on the quality of care provided by individual members of staff.
[How can they not; how can a risk assessment into staff working excessive hours not recognise that?]
216/
[How can they not; how can a risk assessment into staff working excessive hours not recognise that?]
216/
Staff recognised long working hours could impact on the quality of support they provided and told us "Tiredness can make you complacent."
Following feedback changes were made to these risk assessments to recognise the potential impact on care quality of long working hours.
217/
Following feedback changes were made to these risk assessments to recognise the potential impact on care quality of long working hours.
217/
However, we were not provided with any evidence of a plan to enable agency working hours to be reduced to reasonable levels.
The provider had failed to ensure sufficient numbers of suitably experienced staff were deployed to meet people's recognised needs.
218/
The provider had failed to ensure sufficient numbers of suitably experienced staff were deployed to meet people's recognised needs.
218/
This meant the provider was in breach of the requirements of Regulation 18 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
219/
219/
Spectrum has become dependent on one staffing agency to enable it to attempt to meet people's needs at Trelawney House.
Five agency staff were based at Trelawney House at the time of this inspection to cover the ten full time vacancies at the service.
220/
Five agency staff were based at Trelawney House at the time of this inspection to cover the ten full time vacancies at the service.
220/
Staff told us, "The agency staff kept us afloat and are now quite long term."
At our last inspection we found the provider's systems and processes to protect people from abuse were not operated effectively.
When abuse occurred, this had not been reported or investigated.
221/
At our last inspection we found the provider's systems and processes to protect people from abuse were not operated effectively.
When abuse occurred, this had not been reported or investigated.
221/
In addition, during the previous inspection we identified one person was regularly locked in their own room without support from staff.
This was a breach of regulation 13 (Safeguarding service users from abuse and improper treatment) of the Health and Social Care Act 2008
222/
This was a breach of regulation 13 (Safeguarding service users from abuse and improper treatment) of the Health and Social Care Act 2008
222/
This inspection we found people had not been abused and staff and the manager understood how to raise safety concerns.
People were able to freely move around the service and no one was locked in their room. This meant the service was no longer in breach of this regulation.
223/
People were able to freely move around the service and no one was locked in their room. This meant the service was no longer in breach of this regulation.
223/
Staff and the new manager had a good understanding of the local authorities safeguarding procedures and knew to how raise safety concerns.
224/
224/
The manager was able to make safeguarding alerts independently and had appropriately informed the commission of safety incidents that had occurred.
There were appropriate systems in the service to ensure monies held in the service were appropriately managed.
225/
There were appropriate systems in the service to ensure monies held in the service were appropriately managed.
225/
At the time of the inspection Spectrum were acting as appointee for a number of people and had responsibility for managing all aspects of these people's finances.
[Which we've read in the inspection report before, Silverdale, was ripe for financial abuse]
226/
[Which we've read in the inspection report before, Silverdale, was ripe for financial abuse]
226/
These responsibilities were subsequently taken on by Cornwall Council.
This meant people's finances were overseen by an independent body which further protected people from any risk of financial abuse.
227/
This meant people's finances were overseen by an independent body which further protected people from any risk of financial abuse.
227/
At the last inspection risks in relation to one person's mobility had not been appropriately managed.
This was a breach of regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
228/
This was a breach of regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
228/
At this inspection this situation had improved and the person whose mobility had declined had moved into a room on the ground floor.
The service was no longer in breach of this regulation.
[How did it even need pointing out mind?]
229/
The service was no longer in breach of this regulation.
[How did it even need pointing out mind?]
229/
Staff followed processes to assess and provide the support people needed to take their medicines.
However, staff did not use body maps or topical medicines records to record how and where to apply creams or other external medicines.
230/
However, staff did not use body maps or topical medicines records to record how and where to apply creams or other external medicines.
230/
There was limited information for staff to make consistent decisions about when to give 'when required' medicines or to evaluate and record the outcome of taking a 'when required' medicine.
231/
231/
We recommend the provider should ensure that the process for administering 'when required' medicines meets the requirements in @NICEComms guideline 'SC1 – managing medicines in care homes.'
232/
232/
At last inspection the provider did not have robust systems in place to ensure incidents were recorded and learning identified.
This contributed to the breach of regulation 17 (Good governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
233/
This contributed to the breach of regulation 17 (Good governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
233/
At this inspection we found incidents had been documented and reviewed by the manger to identify any areas of possible improvement.
This meant the service was no longer in breach of this part of the regulations.
However, they remain in breach of regulation 17 overall.
234/
This meant the service was no longer in breach of this part of the regulations.
However, they remain in breach of regulation 17 overall.
234/
[Effective - requires improvement]
At our last inspection the provider had failed to comply with two people's DoLS conditions.
In addition, mental capacity assessments were of a generalised nature and not decision specific.
235/
At our last inspection the provider had failed to comply with two people's DoLS conditions.
In addition, mental capacity assessments were of a generalised nature and not decision specific.
235/
This unnecessarily restricted people's freedoms and was a breach of regulation 11 (consent) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
236/
236/
At this inspection the provider had again failed to fully comply with one person's DoLS reporting conditions and mental capacity assessments remained generalised.
This meant the service remains in breach of the requirements of this regulation.
237/
This meant the service remains in breach of the requirements of this regulation.
237/
At this inspection, we found no evidence the provider was providing care in breach of conditions associated with people's DoLS authorisations.
This was a significant improvement since the last inspection.
238/
This was a significant improvement since the last inspection.
238/
However, the provider had failed to comply with reporting conditions associated with one person DoLS authorisation.
The service had failed to document each day, information about the person's engagement and participation in community activities.
239/
The service had failed to document each day, information about the person's engagement and participation in community activities.
239/
Some information had been submitted to the authorising authority in response to the condition, but the information provided was insufficiently detailed.
240/
240/
At this inspection we again found that the provider's procedures for assessing people's capacity were not used in relation to specific decisions.
Instead, assessments had been completed in relation to overarching processes.
241/
Instead, assessments had been completed in relation to overarching processes.
241/
For example, the person's capacity to consent to the overall care plan had been assessed as opposed to in relation to the individual restrictions and controls contained within the care plan.
242/
242/
A standard template had been used to document these processes and the information recorded was also generalised, high level and lacked clear evidence of attempts to involve and support the person to participate in decision making.
243/
243/
This blanket approach to assessing people's ability to make specific decisions was contrary to the underlying principles of the MCA.
The provider had again failed to comply with DoLS conditions and to assess people's capacity in relation to specific decisions.
244/
The provider had again failed to comply with DoLS conditions and to assess people's capacity in relation to specific decisions.
244/
This was a continued breach of the requirements of regulation 11 (consent) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
245/
245/
At our last two inspection we found that carpets were soiled and that the premises had not been kept clean.
This was a breach of regulation 15 of the Health and Social Care Act 2008 (Regulated Activities) Regulations
2014
246/
This was a breach of regulation 15 of the Health and Social Care Act 2008 (Regulated Activities) Regulations
2014
246/
At this inspection the soiled carpets had been replaced and cleanliness had improved.
However, we noted a number of additional issues in relation to maintenance of the environment, including damp in one person's bedroom, failed double glazing, faulty emergency lighting...
247/
However, we noted a number of additional issues in relation to maintenance of the environment, including damp in one person's bedroom, failed double glazing, faulty emergency lighting...
247/
...and unsuitable noisy flooring on stairs.
This meant the service remains in breach of regulation 15.
Documents available in the service identified that noise levels could impact on people's wellbeing.
248/
This meant the service remains in breach of regulation 15.
Documents available in the service identified that noise levels could impact on people's wellbeing.
248/
The stairs in the service had laminate floor coverings and were very loud when walked upon.
This may impact on people's ability to sleep or relax.
Staff told us, "We need a carpet on the stairs, it's a creaky old house".
[A creaky old house]
249/
This may impact on people's ability to sleep or relax.
Staff told us, "We need a carpet on the stairs, it's a creaky old house".
[A creaky old house]
249/
The service emergency lighting was faulty, seven different emergency lights were non-operational.
These faults had first been identified in February 2022 but not resolved by the time of this inspection.
[Inspection is in May, 3 months tolerating inadequate]
250/
These faults had first been identified in February 2022 but not resolved by the time of this inspection.
[Inspection is in May, 3 months tolerating inadequate]
250/
In addition, necessary fire alarm zoning maps were not displayed next to the service's fire board.
A large number of double-glazed windows in peoples' rooms and in communal spaces were blown and thus difficult to see through.
251/
A large number of double-glazed windows in peoples' rooms and in communal spaces were blown and thus difficult to see through.
251/
In one person's bedroom there was a significant area of damp. These issues had been identified by audits but not resolved.
[Such apathy, such carelessness, such indifference]
252/
[Such apathy, such carelessness, such indifference]
252/
Necessary periodic testing of the service's electrical circuits had not been completed.
The provider had failed to appropriately maintain the service and adapt it to people's recognised needs.
253/
The provider had failed to appropriately maintain the service and adapt it to people's recognised needs.
253/
This was a continued breach of regulation 15 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
254/
254/
At our last inspection training had not been regularly updated to ensure staff had the skills necessary to meet people's needs.
This was a breach of regulation 18 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
255/
This was a breach of regulation 18 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
255/
At this inspection records showed staff had completed additional training to provide them with the skills necessary to meet people needs.
256/
256/
At our last inspection we found staff had not supported people to eat and drink in accordance with their recognised care needs.
This was a breach of regulation 14 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
257/
This was a breach of regulation 14 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
257/
At this inspection we found people's hydration and nutritional needs were being met. Necessary support was provided at mealtimes and the service was no longer in breach of this regulation.
258/
258/
At our last inspection one person had become withdrawn and did not eat their lunch because of a lack of support from staff.
At this inspection this person was effectively supported by staff at mealtimes and ate well.
259/
At this inspection this person was effectively supported by staff at mealtimes and ate well.
259/
[Caring - good]
At the last inspection we found noise levels at night prevented people from having adequate sleep, people's dignity had not always been respected and the high turnover of staff meant people's needs were not fully understood.
260/
At the last inspection we found noise levels at night prevented people from having adequate sleep, people's dignity had not always been respected and the high turnover of staff meant people's needs were not fully understood.
260/
This was a breach of regulation 9 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
261/
261/
At this inspection we found noise levels at night had reduced, people were treated with dignity and that, although staffing turnover remained an issue, staff now had a better understanding of people's individual needs.
262/
262/
This meant the service was no longer in breach of regulation 9.
People and relatives consistently reported people were now better able to rest at night.
One person told us, "I had a good night's sleep" and staff said, "People are sleeping better."
263/
People and relatives consistently reported people were now better able to rest at night.
One person told us, "I had a good night's sleep" and staff said, "People are sleeping better."
263/
People were comfortable and relaxed in their home.
We observed numerous positive, caring and supportive interaction between people and their support staff. People told us, "[The staff] are lovely", "The staff are good" and "All the staff now are good. They have patience".
264/
We observed numerous positive, caring and supportive interaction between people and their support staff. People told us, "[The staff] are lovely", "The staff are good" and "All the staff now are good. They have patience".
264/
People were free to move around the service and were able to spend time on their own if they wished.
The atmosphere on both inspection days was positive and relaxed.
265/
The atmosphere on both inspection days was positive and relaxed.
265/
People were now routinely involved in planning activities and deciding how to spend their time.
On both inspection days people had planned to go out at various times in the day for shopping trips and to access local leisure facilities.
266/
On both inspection days people had planned to go out at various times in the day for shopping trips and to access local leisure facilities.
266/
One person had planned to visit a local tourist attraction on the second day of our inspection.
A second person, hearing the planning for this trip decided they would also like to go, and this was arranged.
267/
A second person, hearing the planning for this trip decided they would also like to go, and this was arranged.
267/
Staff described the positive impact this increased control over their lives had on people's wellbeing.
[Part of me is delighted to read this, another is absolutely horrified that this needed pointing out. How much misery were people enduring before]
268/
[Part of me is delighted to read this, another is absolutely horrified that this needed pointing out. How much misery were people enduring before]
268/
One staff member told us,
"We now let [person's name] pick, [they] are more easy going, it has completely changed the person, so much happier. [The person] gets out and about and loves walks now."
269/
"We now let [person's name] pick, [they] are more easy going, it has completely changed the person, so much happier. [The person] gets out and about and loves walks now."
269/
A second staff member said in relation to another person, "[The person] can do what [they] like, it is a big change"
270/
270/
[Responsive - requires improvement]
At our last inspection we found specific guidance in relation to one person's mobility needs and vehicles had not been followed.
This impacted on their wellbeing and was a breach of regulation 9 of the Health and Social Care Act 2008
271/
At our last inspection we found specific guidance in relation to one person's mobility needs and vehicles had not been followed.
This impacted on their wellbeing and was a breach of regulation 9 of the Health and Social Care Act 2008
271/
At this inspection this person was appropriately supported to access the service's vehicle with dignity.
This meant the service was no longer in breach of this regulation.
272/
This meant the service was no longer in breach of this regulation.
272/
At our last inspection we found care records were lengthy, complex documents which staff did not fully understand and that daily care records had not been accurately maintained.
This formed part of a breach of Regulation 17 of the Health and Social Care Act 2008
273/
This formed part of a breach of Regulation 17 of the Health and Social Care Act 2008
273/
At this inspection we found daily care records had been accurately completed and, although care plans remained lengthy, staff had a better understanding of people's needs.
274/
274/
This meant that although the service is no longer in breach of the regulations, further improvements in relation to care plans are required.
The updated care plans gave staff a better understanding of people's current support needs.
275/
The updated care plans gave staff a better understanding of people's current support needs.
275/
However, on the first day of the inspection we identified that one person's care plan that had not yet been updated and contained a number of contradictory protocols not reflected in the rest of their care plan.
276/
276/
This issue was reported to the acting manager and senior carer responsible.
By the second day of the inspection this contradictory guidance had been updated to ensure staff consistently provided support as detailed in the person's care plan.
277/
By the second day of the inspection this contradictory guidance had been updated to ensure staff consistently provided support as detailed in the person's care plan.
277/
Some of the language used in care plans and daily care records did not effectively describe what had happened.
For example, the term "Off baseline" was used to describe people when they became angry, anxious, excited, upset or frustrated.
278/
For example, the term "Off baseline" was used to describe people when they became angry, anxious, excited, upset or frustrated.
278/
This meant it was difficult to identify people's emotional state when reviewing the information. This language use is not in line with best practice.
We recommend the provider seeks guidance from external sources on the appropriate use of language in care records.
279/
We recommend the provider seeks guidance from external sources on the appropriate use of language in care records.
279/
The provider used a digital record keeping system to document the support people had received.
Staff and the manager were unable to review this information in chronological order once it had been entered.
280/
Staff and the manager were unable to review this information in chronological order once it had been entered.
280/
This had made it very difficult to identify developing patterns in people's behaviours or occasions where daily care records had been missed.
The new manager had re-introduced the use of paper based daily care records.
281/
The new manager had re-introduced the use of paper based daily care records.
281/
At our last inspection we found noise levels in the service were impacting on people's wellbeing and people's behaviours were adversely impacting on others.
This was a breach of Regulation 9 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
282/
This was a breach of Regulation 9 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
282/
At this inspection we found these issues had significantly improved and noise levels in the service had reduced.
This meant the service was no longer in breach of this regulation.
283/
This meant the service was no longer in breach of this regulation.
283/
Last inspection staff did not have the skills to communicate effectively with individuals who used signs to aid their communication.
This failing formed part of the breach of Regulation 18 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
284/
This failing formed part of the breach of Regulation 18 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
284/
At this inspection we found three senior staff had begun training in the use of signs to aid communication and that staff had worked with people and relatives to gain a better understanding of how people used signs to communicate.
285/
285/
This meant the service was no longer in beach of this regulation.
One person's care plan had been updated with support from the person and their relatives.
It now included a photo-based dictionary of signs, performed by the person, to help staff identify...
286/
One person's care plan had been updated with support from the person and their relatives.
It now included a photo-based dictionary of signs, performed by the person, to help staff identify...
286/
...and recognise particular signs and understand their meanings.
Staff told us their increased use of signs had impacted positively on other aspects of this person's communication.
[Well what do you know]
287/
Staff told us their increased use of signs had impacted positively on other aspects of this person's communication.
[Well what do you know]
287/
With pleasure, staff explained how this person's speech was returning and how this enabled the person to have greater control of their life.
[This is good, but I can't reconcile this with how much this person had withdrawn due to poor care in the first place]
288/
[This is good, but I can't reconcile this with how much this person had withdrawn due to poor care in the first place]
288/
At our last inspection people spent most of their time in the service with limited opportunities to go out or to access the community.
These issues had been caused by a combination of low staffing levels, limited availability of drivers and the service's rural location.
289/
These issues had been caused by a combination of low staffing levels, limited availability of drivers and the service's rural location.
289/
At this inspection, we found people were now being regularly supported to go out and to access the community.
[When there were enough staff to do so... not at weekends as per earlier]
290/
[When there were enough staff to do so... not at weekends as per earlier]
290/
People's increased engagement in community activities had also impacted positively of staff morale.
Staff enjoyed supporting people to access the community and told us "Now we are getting out most days" and "It is enjoyable as you get out and about."
[Better for everyone]
291/
Staff enjoyed supporting people to access the community and told us "Now we are getting out most days" and "It is enjoyable as you get out and about."
[Better for everyone]
291/
Staff recognised the improved staffing levels had impacted positively on people's freedom but acknowledged there were still occasions when people's freedoms were restricted.
Staff told us, "We need to have the 2:1 hours, otherwise we are confined to base."
292/
Staff told us, "We need to have the 2:1 hours, otherwise we are confined to base."
292/
Although staffing was more limited at the weekend this had not always prevented people from going out and a relative told us, "[My relative] has been going out at weekends as well and has visited us."
[Not always... but it had, and did, and does]
293/
[Not always... but it had, and did, and does]
293/
[Well-led - inadequate]
At the previous inspection, the provider's acting manager had failed to effectively lead the staff team and inconsistencies in information provided by the acting manager prevented concerns about staffing arrangements from being fully investigated.
294/
At the previous inspection, the provider's acting manager had failed to effectively lead the staff team and inconsistencies in information provided by the acting manager prevented concerns about staffing arrangements from being fully investigated.
294/
This meant the service was in breach of regulation 17 (Good governance) of The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
295/
295/
At this inspection a new manager had been appointed.
They provided effective leadership to the staff team and were honest throughout the inspection process.
However, the new manager did not intend to become the service's registered manager.
296/
They provided effective leadership to the staff team and were honest throughout the inspection process.
However, the new manager did not intend to become the service's registered manager.
296/
[Parachuting managers in is a short term solution, they may change things around, but will it remain that way?]
This meant there was ongoing risk of management instability at the service and improvements may not be sustained.
The service remains in breach of regulation 17
297/
This meant there was ongoing risk of management instability at the service and improvements may not be sustained.
The service remains in breach of regulation 17
297/
We were not reassured about the long-term management arrangements at the service.
The new manager had not applied to become the service's registered manager and told us they had been recruited by the provider to manage another type of service...
298/
The new manager had not applied to become the service's registered manager and told us they had been recruited by the provider to manage another type of service...
298/
...and would not be applying for registration at Trelawney House.
This meant there was a risk of further management instability at the service.
The provider did not have a plan in place to mitigate this risk.
[The provider is consistently poor/absent. Zero leadership]
299/
This meant there was a risk of further management instability at the service.
The provider did not have a plan in place to mitigate this risk.
[The provider is consistently poor/absent. Zero leadership]
299/
Staff were highly complementary of the new manager's leadership.
They told us, "[New manager's name] is a proper manager and has just turned everything around. It is a pleasure working here at the moment."
300/
They told us, "[New manager's name] is a proper manager and has just turned everything around. It is a pleasure working here at the moment."
300/
The new manager was open and honest throughout the inspection process.
Where possible, they provided accurate and timely responses to questions raised during the inspection process.
301/
Where possible, they provided accurate and timely responses to questions raised during the inspection process.
301/
Where issues and concerns were identified during the inspection, prompt action was taken to make improvements to the service's performance by the manager and staff team.
302/
302/
Professionals recognised the new manager had a positive impact of the service's performance.
They told us, "Since [manager's name] has taken on the team lead role things have improved."
303/
They told us, "Since [manager's name] has taken on the team lead role things have improved."
303/
Since last inspection two senior carers and positive behaviour support leads had been appointed.
This meant there were now appropriate leadership structures within the service and the manager had been able to delegate some roles and responsibilities to these senior staff.
304/
This meant there were now appropriate leadership structures within the service and the manager had been able to delegate some roles and responsibilities to these senior staff.
304/
Staff had a good understating of the duties and responsibilities of these leaders within the staff team.
Staff recognised the improved leadership arrangements had impacted positively on people's wellbeing and staff morale.
305/
Staff recognised the improved leadership arrangements had impacted positively on people's wellbeing and staff morale.
305/
One staff member told us,
"We were all thinking about quitting at the last inspection. It is so much better now. The care did not go down, but morale was down. It is a million times better now".
[This is so important, yet silent in #socialcare crisis talk]
306/
"We were all thinking about quitting at the last inspection. It is so much better now. The care did not go down, but morale was down. It is a million times better now".
[This is so important, yet silent in #socialcare crisis talk]
306/
This contributed to the breach regulation 17 (Good governance) of The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
307/
307/
At the last inspection, the provider had failed to make necessary safeguarding referrals when abuse had been reported by staff, DoLS condition had not been complied with, necessary notifications had not been submitted to CQC and staffing levels were unsafe.
308/
308/
The providers quality assurance system had failed to identify and address these failing prior to the inspection.
This meant the provider was in breach of the requirements of regulation 17 Good governance) of The Health and Social Care Act 2008 (Regulated Activities)
309/
This meant the provider was in breach of the requirements of regulation 17 Good governance) of The Health and Social Care Act 2008 (Regulated Activities)
309/
At this inspection the provider had addressed some of these issues;
Necessary safeguarding alerts had been made and notifications submitted to the commission as required.
310/
Necessary safeguarding alerts had been made and notifications submitted to the commission as required.
310/
However, the provider's systems had again failed to ensure DoLS conditions were complied with and the service remained understaffed.
This meant that although the service's performance had improved in some areas, governance systems remained ineffective.
311/
This meant that although the service's performance had improved in some areas, governance systems remained ineffective.
311/
This is a repeated breach of the regulations.
There remained a disconnect between the provider and the service.
Staff now felt well supported by their manager but questioned the role of the provider's senior management in supporting the service.
312/
There remained a disconnect between the provider and the service.
Staff now felt well supported by their manager but questioned the role of the provider's senior management in supporting the service.
312/
One staff member said, "The team supporting each other, I would say that is the only support we have had."
While relatives told us, "I think head office are a bit slow to improve things but with regards the actual house we are really pleased..."
313/
While relatives told us, "I think head office are a bit slow to improve things but with regards the actual house we are really pleased..."
313/
"...I think they do not always get enough input from head office."
The provider's quality assurance systems had not ensured the service achieved full compliance with the regulations as detailed in the safe and effective sections of this report.
314/
The provider's quality assurance systems had not ensured the service achieved full compliance with the regulations as detailed in the safe and effective sections of this report.
314/
The provider had not checked recruitment practices at an agency they used extensively.
As detailed in the safe section of this report, the staffing agency had not fully completed pre-employment checks.
This had not been identified by Spectrum.
315/
As detailed in the safe section of this report, the staffing agency had not fully completed pre-employment checks.
This had not been identified by Spectrum.
315/
The provider's systems had failed to identify that the information necessary to achieve compliance with one person's DoLS condition was not being recorded.
An external auditor had visited the service to assess its performance prior to the inspection.
[Performative]
316/
An external auditor had visited the service to assess its performance prior to the inspection.
[Performative]
316/
However, the results of this audit had not been shared with the manager prior to our inspection.
This meant they did not have the necessary information to drive improvements.
[What. Is. The. Point?]
317/
This meant they did not have the necessary information to drive improvements.
[What. Is. The. Point?]
317/
The providers system had failed to ensure compliance with the regulations and there was no registered manager in post.
This meant the provider remains in breach of the requirements of regulation 17 (Good governance) of The Health and Social Care Act 2008
318/
This meant the provider remains in breach of the requirements of regulation 17 (Good governance) of The Health and Social Care Act 2008
318/
[That's it for Trelawney House.
Seems like very fragile progress to me.
I'll get to the other reports tomorrow. Need to step away from it. Grotty, grotty reality for people stuck there, just down the road]
319/tbc
Seems like very fragile progress to me.
I'll get to the other reports tomorrow. Need to step away from it. Grotty, grotty reality for people stuck there, just down the road]
319/tbc
Heightlea in Truro
[More inadequate care from @ASDspectrumASD]
Heightlea is a residential care home providing personal care to five people with a learning disability or autistic people.
320/
[More inadequate care from @ASDspectrumASD]
Heightlea is a residential care home providing personal care to five people with a learning disability or autistic people.
320/

It is part of the Spectrum (Devon and Cornwall Autistic Community Trust) group, a provider with several similar services across Cornwall.
Heightlea is close to the city of Truro.
The model of care did not maximise people's choice, control and independence.
321/
Heightlea is close to the city of Truro.
The model of care did not maximise people's choice, control and independence.
321/
Staff told us they were committed to finding new activities and opportunities that met people's preferences.
However, people received limited support to identify long term goals.
322/
However, people received limited support to identify long term goals.
322/
This meant activities and how they spent their time were not always part of a clearly laid out plan to ensure they lived a meaningful life.
How people spent their time was also sometimes limited by the number of staff or vehicles available.
[Again and again and again]
323/
How people spent their time was also sometimes limited by the number of staff or vehicles available.
[Again and again and again]
323/
People were not always supported to develop their independence or to increase the control they had over their own lives.
People's care plans did not focus on people's strengths or identify areas where people wanted to develop skills.
[This is warehousing, not support]
324/
People's care plans did not focus on people's strengths or identify areas where people wanted to develop skills.
[This is warehousing, not support]
324/
People who experienced periods of distress had plans in place which ensured physical restraint was only used by staff if there was no alternative.
[Except you gotta wonder whether the periods of distress people experienced would be less, if they had meaningful lives]
325/
[Except you gotta wonder whether the periods of distress people experienced would be less, if they had meaningful lives]
325/
However, there were several restrictions in place in the service that were not the least restrictive options or in people's best interests.
People had some choice about their living environment and were able to personalise their rooms.
326/
People had some choice about their living environment and were able to personalise their rooms.
326/
People were able to socialise in the living areas and enjoyed the privacy of their own rooms when they chose.
People were supported to use community health and social care services when needed.
Staff supported people safely with their medicines.
327/
People were supported to use community health and social care services when needed.
Staff supported people safely with their medicines.
327/
The provider had not given sufficient support to the service. This meant staff did not always recognise poor care or take action to make appropriate changes.
People did not always receive support that focused on their quality of life and followed best practice.
328/
People did not always receive support that focused on their quality of life and followed best practice.
328/
There was an overly cautious culture in the service that did not enable people to take positive risks.
[Or live their lives. I'm probably way too cynical this early on, but is it an overly cautious culture, or an overly lazy culture focused on staff convenience? Let's see]
329/
[Or live their lives. I'm probably way too cynical this early on, but is it an overly cautious culture, or an overly lazy culture focused on staff convenience? Let's see]
329/
Information shared by the provider regarding people's finances showed the provider's systems were not robust and did not protect people adequately from the risk of financial abuse.
[Surely they just need closing down at this stage]
330/
[Surely they just need closing down at this stage]
330/
The service was understaffed and did not always provide the number of hours to each person they had been assessed as needing.
[Which, if they continued to bill for them, is also fraud]
People received kind care from staff who valued their relationships with people.
331/
[Which, if they continued to bill for them, is also fraud]
People received kind care from staff who valued their relationships with people.
331/
[Not sure kindness cuts it, when people aren't being supported to live an actual life]
People were able to communicate with staff and understand information given to them by staff who understood their individual communication needs.
332/
People were able to communicate with staff and understand information given to them by staff who understood their individual communication needs.
332/
People did not lead fully inclusive or empowered lives.
The ethos and culture of the service were paternalistic which limited the opportunities people were offered.
[Paternalistic kindness masquerading as support. Not a life I'd want to live]
333/
The ethos and culture of the service were paternalistic which limited the opportunities people were offered.
[Paternalistic kindness masquerading as support. Not a life I'd want to live]
333/
Staff knew and understood people well, however the provider had not ensured they had a good understanding of best practice models of care.
This meant staff did not consistently support people's aspirations to live a quality life of their choosing.
334/
This meant staff did not consistently support people's aspirations to live a quality life of their choosing.
334/
There was a culture of improvement within the service; however staff did not always have the skills and knowledge to identify all areas for improvement.
People's views as well as the views of those who were important to them were respected and listened to.
335/
People's views as well as the views of those who were important to them were respected and listened to.
335/
People were not always supported to have maximum choice and control of their lives and staff did not support them in the least restrictive way possible and in their best interests; the policies and systems in the service did not support best practice.
336/
336/
The last rating for this service was requires improvement (published 19 February 2022) and there were breaches of regulation in staffing, good governance and safe care and treatment.
337/
337/
We specified a date by which the provider needed to meet the requirements of the regulations regarding good governance.
338/
338/
At an inspection in June 2021, due to concerns about staffing, we required the provider to share monthly reports detailing the numbers and training of staff in the service each day, including the number of management hours the registered manager completed.
339/
339/
Concerns about staffing were again identified at the February 2022 inspection so the provider was required to continue sending monthly reports.
At this inspection we found the provider remained in breach of regulations.
340/
At this inspection we found the provider remained in breach of regulations.
340/
The last two ratings for this service were requires improvement (published 15 November 2022 and 19 February 2022).
The service has now deteriorated to inadequate and has therefore been rated below good for the last three consecutive inspections.
341/
The service has now deteriorated to inadequate and has therefore been rated below good for the last three consecutive inspections.
341/
[This 'service' has been sub-standard for over a year. Imagine being one of those people in this place, or any other of the provider's 'homes' with inadequate staffing levels, a paternalistic culture, and no ambition or meaningful activity in your life]
342/
342/
We have found evidence that the provider needs to make improvements.
We have identified breaches in relation to person centred care, safe care and treatment, ensuring all decisions are in people's best interests, staffing and governance of the service.
343/
We have identified breaches in relation to person centred care, safe care and treatment, ensuring all decisions are in people's best interests, staffing and governance of the service.
343/
At the time of our inspection there was a registered manager in post.
This inspection was unannounced.
344/
This inspection was unannounced.
344/
[Safe - inadequate]
At the last inspection we found the provider had not done all that was reasonably practicable to ensure the health and safety of service users.
This was a breach of regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008
345/
At the last inspection we found the provider had not done all that was reasonably practicable to ensure the health and safety of service users.
This was a breach of regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008
345/
Not enough improvement had been made at this inspection and the provider was still in breach of regulation 12.
Measures to keep people safe were not always adequate.
346/
Measures to keep people safe were not always adequate.
346/
Following our visit to the service, we received a report that one person had been in an accident in one of the provider's vehicles.
347/
347/
A removable seat had not been secured in the vehicle properly before the person used it and during a journey, the seat fell out of position onto the floor, with the person still in it with their seat belt attached.
[Awful, just awful. So dangerous]
348/
[Awful, just awful. So dangerous]
348/
Action to review and understand people's behaviour was not always done promptly.
In May 2022, one person began using a behaviour to communicate.
349/
In May 2022, one person began using a behaviour to communicate.
349/
The service sought support from external professionals but were not supported by the provider's internal behavioural team whilst they waited for the response.
[Escalate and then just ignore]
350/
[Escalate and then just ignore]
350/
At the time of the inspection on 14 June, the service had not received any internal advice to help the person stop putting themselves at risk by repeating the behaviour
Regular checks of fire equipment and the fire alarm had been completed.
351/
Regular checks of fire equipment and the fire alarm had been completed.
351/
However, the service did not have signs identifying where fire exits were, or any automatic door releases. We contacted the fire service about this.
[This place is so dangerous]
352/
[This place is so dangerous]
352/
Records of training for three staff members indicated they had not completed fire training despite working in the service regularly.
Staff completed temperature checks of the water, fridge and freezer.
353/
Staff completed temperature checks of the water, fridge and freezer.
353/
Action had been taken when the water temperatures were not within the required range; but records indicated action had not always been taken when the fridge or freezer temperatures were not within a safe range.
[I don't understand what affects water temps; dodgy boiler?]
354/
[I don't understand what affects water temps; dodgy boiler?]
354/
This is an ongoing breach of regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
355/
355/
There were grab bags and PEEPS (personal emergency evacuation plans) available near exits for an emergency.
However, these did not contain any contact numbers or details of people's medicines.
The registered manager said they would put this in place.
356/
However, these did not contain any contact numbers or details of people's medicines.
The registered manager said they would put this in place.
356/
At our last inspection we found staffing levels were not consistently met.
This was a continued breach of regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
[Continued last time... wait for it....]
357/
This was a continued breach of regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
[Continued last time... wait for it....]
357/
Not enough improvement had been made at this inspection and the provider was still in breach of regulation 18.
The service was still not consistently providing the level of support to people it was commissioned to provide.
358/
The service was still not consistently providing the level of support to people it was commissioned to provide.
358/
Each of the five people living in the service required one to one support each day.
However, on five days in April 2022 and seven days in May 2022, staffing was below this level all day.
359/
However, on five days in April 2022 and seven days in May 2022, staffing was below this level all day.
359/
On seven days in April 2022 and on 15 days in May 2022 staffing was below this level for part of the day.
This had a negative impact on people's right to live their life as they chose.
[And it's not what the commissioner, or your taxes, are paying for.
It's not a life]
360/
This had a negative impact on people's right to live their life as they chose.
[And it's not what the commissioner, or your taxes, are paying for.
It's not a life]
360/
The service was understaffed and did not always provide the number of hours to each person they had been assessed as needing.
There were four staff vacancies at the service.
361/
There were four staff vacancies at the service.
361/
Two of these vacancies were being covered by one member of agency staff. Existing permanent and bank staff were covering remaining shifts when possible.
One agency staff member worked a significant number of hours each week.
362/
One agency staff member worked a significant number of hours each week.
362/
The registered manager completed a risk assessment stating the staff member could not work more than 84 hours per week and would have one full day off per week; however, we found occasions in April and May 2022 when the staff member had worked 13 and 14 days in a row.
363/
363/
Working these excessive hours with limited opportunities for rest exposed both the staff member and the people they supported to significant risk of harm.
364/
364/
This was a continued breach of regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
[Another, continued breach]
365/
[Another, continued breach]
365/
The registered manager told us they had taken one person with them to a recruitment day and had let the provider know what sort of staff were suitable for the service; but apart from that, people were not involved in staff recruitment.
[No say on who is in their home]
366/
[No say on who is in their home]
366/
Recruitment checks had been completed on new staff.
One staff member had been recruited via a staffing agency.
Their recruitment details did not include a full employment history, as required.
367/
One staff member had been recruited via a staffing agency.
Their recruitment details did not include a full employment history, as required.
367/
The provider told us they were currently working with the agency to ensure all relevant information was sought and shared in the future.
[Outsourcing responsibility for staffing, and for ensuring adequate checks were in place. Such total apathy]
368/
[Outsourcing responsibility for staffing, and for ensuring adequate checks were in place. Such total apathy]
368/
Three people relied on the provider to transfer their benefits into their personal accounts.
Their benefits were paid fortnightly, but their bank statements showed their benefits were not transferred at fortnightly or consistent intervals.
[Financial abuse in plain sight]
369/
Their benefits were paid fortnightly, but their bank statements showed their benefits were not transferred at fortnightly or consistent intervals.
[Financial abuse in plain sight]
369/
The lack of oversight from any other party indicated a closed culture and increased the risk of abuse.
Following the inspection, the Department for Work and Pensions (DWP) transferred the responsibility for overseeing people's benefits and bank accounts...
370/
Following the inspection, the Department for Work and Pensions (DWP) transferred the responsibility for overseeing people's benefits and bank accounts...
370/
...to the local authority from the provider for all those supported by the provider because the DWP was dissatisfied by how people's personal money was being managed.
[I can't imagine DWP have particularly high standards, or are very proactive, so this says a lot]
371/
[I can't imagine DWP have particularly high standards, or are very proactive, so this says a lot]
371/
This meant the provider was no longer allowed to be responsible for managing people's benefits and finances.
The provider had mismanaged people's money.
Two vehicles had been leased for four people to use at the service. The fifth person had their own vehicle.
372/
The provider had mismanaged people's money.
Two vehicles had been leased for four people to use at the service. The fifth person had their own vehicle.
372/
Information from the provider stated that total charges for the two leased vehicles and the person's own vehicle were charged equally to the five people.
373/
373/
This meant the person who owned and used their own car was also paying money towards the leased vehicle, used by others.
[This is fraud. It is financial abuse, in clear sight. Daylight.
This provider is not fit for purpose]
374/
[This is fraud. It is financial abuse, in clear sight. Daylight.
This provider is not fit for purpose]
374/
This was a breach of regulation 13 (Safeguarding service users from abuse and improper treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
375/
375/
Staff completed three assessments of their competency to administer and manage medicines when they started working at the service.
The provider's policy stated that staff's competence should be re-assessed annually, but this had not been done.
376/
The provider's policy stated that staff's competence should be re-assessed annually, but this had not been done.
376/
The observation form used to assess staff's competence in medicines management and administration did not provide any guidance about specifically what assessors should observe or check.
[Performative scrutiny. Meaningless box ticking]
377/
[Performative scrutiny. Meaningless box ticking]
377/
This meant different staff acting as assessors might not have been consistent in the areas they observed and assessed.
378/
378/
People's care plans detailed that staff needed to administer their medicines, but did not provide person centred detail about how, where or when they preferred their medicines to be administered.
379/
379/
This contributed to the ongoing breach of regulation 17 (Good governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
380/
380/
We were somewhat assured that the provider was preventing visitors from catching and spreading infections.
During the inspection, the staff were no longer wearing masks as the provider had misunderstood changes in government guidance.
381/
During the inspection, the staff were no longer wearing masks as the provider had misunderstood changes in government guidance.
381/
We were somewhat assured that the provider was using PPE effectively and safely.
Changes were made to rectify a misunderstanding of the government guidance following the inspection.
382/
Changes were made to rectify a misunderstanding of the government guidance following the inspection.
382/
We were somewhat assured that the provider's infection prevention and control policy was up to date.
The provider had misunderstood changes to government guidance and changed their policy.
We were told this was changed back promptly following the inspection.
383/
The provider had misunderstood changes to government guidance and changed their policy.
We were told this was changed back promptly following the inspection.
383/
[Effective - requires improvement]
People did not always receive support that focused on their quality of life and followed best practice.
[Am dreading what is coming after reading the previous two inadequate reports - an inevitable abusive star chart/naughty step I fear]
384/
People did not always receive support that focused on their quality of life and followed best practice.
[Am dreading what is coming after reading the previous two inadequate reports - an inevitable abusive star chart/naughty step I fear]
384/
People had reward charts and restrictions in place to alter or control their behaviour, rather than clear plans detailing what steps staff needed to take to understand the behaviour and how to better meet the person's needs.
[Adults, in their own home, infantalised]
385/
[Adults, in their own home, infantalised]
385/
Two people had reward charts in place.
The use of rewards to modify behaviour was infantilising.
The reward charts involved the people being given tokens by staff members if their behaviour complied with the expectations of the service.
[Noooooooo. Just no]
386/
The use of rewards to modify behaviour was infantilising.
The reward charts involved the people being given tokens by staff members if their behaviour complied with the expectations of the service.
[Noooooooo. Just no]
386/
This produced an imbalance of power between the people and staff members.
It was also a punitive approach as the tokens were restricted if the people's behaviour did not meet expectations.
387/
It was also a punitive approach as the tokens were restricted if the people's behaviour did not meet expectations.
387/
There was an overly cautious culture in the service that did not enable people to take positive risks.
Some people had restrictions placed on them that were not always the least restrictive option.
[Eurgh. In their own home. Taking what little pleasure they have away]
388/
Some people had restrictions placed on them that were not always the least restrictive option.
[Eurgh. In their own home. Taking what little pleasure they have away]
388/
One person had their radio locked away because they liked to play it loudly and another person had their alcoholic drink stored in the office.
[Imagine. You like loud music. Your source of joy is locked away.... you're not bought headphones, or asked to turn it down]
389/
[Imagine. You like loud music. Your source of joy is locked away.... you're not bought headphones, or asked to turn it down]
389/
A record was in place to review restrictive practices, but it had not been used effectively to review and reduce these restrictions.
There was no evidence that these restrictions were a last resort and that other less restrictive options had previously been tried.
390/
There was no evidence that these restrictions were a last resort and that other less restrictive options had previously been tried.
390/
At times staff restricted people's choices and options without clear evidence this was in the person's best interests.
[Control. The subtext to this is staff, however kind, were treating grown adults like lesser humans, children, or less than]
391/
[Control. The subtext to this is staff, however kind, were treating grown adults like lesser humans, children, or less than]
391/
For example, one person enjoyed mixing different foods together.
Staff were discouraging the person from doing this rather than taking time to understand what need the person was trying to meet.
392/
Staff were discouraging the person from doing this rather than taking time to understand what need the person was trying to meet.
392/
One person did not have their own bank account.
This had denied them the right to manage and control their own money and placed them at risk of financial abuse.
Their money was paid into the service's housekeeping account.
[No wonder @ChtyCommission are investigating]
393/
This had denied them the right to manage and control their own money and placed them at risk of financial abuse.
Their money was paid into the service's housekeeping account.
[No wonder @ChtyCommission are investigating]
393/
They did not always use all the money they received each month and so did not withdraw the full amount.
This meant some of their saved money was kept in the service's housekeeping account.
[Whaaat. This is financial abuse, it's not a risk of financial abuse, it is abuse]
394/
This meant some of their saved money was kept in the service's housekeeping account.
[Whaaat. This is financial abuse, it's not a risk of financial abuse, it is abuse]
394/
They had not been supported to set up their own personal bank account and so continued to be reliant on staff withdrawing and keeping their money in a bank account that did not belong to them.
395/
395/
This was a breach of regulation 13 (Safeguarding service users from abuse and improper treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
396/
396/
Skills teaching and individualised learning programmes were not part of the culture in the service.
People's care plans did not focus on people's strengths or identify areas where people wanted to develop skills.
397/
People's care plans did not focus on people's strengths or identify areas where people wanted to develop skills.
397/
Plans to help people achieve aspirations focused mostly on staff completing tasks rather than on how people could be supported to complete or be involved in these tasks, whilst learning skills.
398/
398/
This contributed to a breach of regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
399/
399/
Systems to ensure staff had the appropriate skills and knowledge to support people in line with their needs were not robust.
This meant staff did not always recognise poor care or take appropriate action to make changes.
400/
This meant staff did not always recognise poor care or take appropriate action to make changes.
400/
Staff were required by the provider to undertake assessments of their understanding of various aspects of the service, including the care and support each person required.
Some staff who had worked in the service for several months had not completed all assessments.
401/
Some staff who had worked in the service for several months had not completed all assessments.
401/
Other staff members had partially completed the assessments and others had completed the assessments, but these had not signed by the staff member or the assessor.
402/
402/
This meant their competence and understanding of the service and the people they supported had not been assessed in line with the provider's procedure.
[Such total disregard for the basics. Such care-less non-leadership from the provider]
403/
[Such total disregard for the basics. Such care-less non-leadership from the provider]
403/
The service was delivered for people with autism, however, according to the service's training records, four staff members who had worked at the service had not completed autism training.
404/
404/
There was no evidence that staff continued to develop their understanding of autism and related best practice.
Staff completed forms which recorded how people used their behaviour to communicate.
[I bet they did. And took their 'tokens' away when they did so]
405/
Staff completed forms which recorded how people used their behaviour to communicate.
[I bet they did. And took their 'tokens' away when they did so]
405/
The registered manager told us the forms were to record regular but low intensity behaviour.
However, not all information recorded was relevant.
For example, sometimes staff recorded something someone did to tell staff they wanted support with personal care.
406/
However, not all information recorded was relevant.
For example, sometimes staff recorded something someone did to tell staff they wanted support with personal care.
406/
This showed staff did not have a comprehensive understanding of the reason for the form.
This formed part of a continued breach of regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
407/
This formed part of a continued breach of regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
407/
People were involved in choosing their food, shopping, and planning their meals; however apart from some dislikes, there was no information about their food or meal preferences in their care plans.
[Which is hugely problematic given the reliance on agency staff]
408/
[Which is hugely problematic given the reliance on agency staff]
408/
Staff supported people to be involved in preparing and cooking their own meals; however detailed information about what support people required to prepare food, or what skills they wanted to develop to increase their independence was not included.
409/
409/
Following the inspection, the provider told us care planning documentation was being revised and this information would be included in the future.
[Of course. Didn't bother after the previous inspections though. Inspector induced apathetic action]
410/
[Of course. Didn't bother after the previous inspections though. Inspector induced apathetic action]
410/
The communal areas of the service were being redecorated but the people living at the service had not been involved in choosing the colours.
[I mean it's only their home. How many of you live in a home where you have no say in any decor anywhere except your own bedroom?]
411/
[I mean it's only their home. How many of you live in a home where you have no say in any decor anywhere except your own bedroom?]
411/
The registered manager told us people would be offered the choice to have their own rooms decorated and would be able to choose the colours they preferred.
[Performative paint chart choices... meanwhile radios locked away so you can't relax in your room listening to music]
412/
[Performative paint chart choices... meanwhile radios locked away so you can't relax in your room listening to music]
412/
Some mental capacity assessments were in place; however some decisions had been made on people's behalf without an assessment of their capacity to make their own decision; or a record of why the decisions made were in their best interests.
413/
413/
Several restrictions were in place in the service but no record that the people involved could not make these decisions; or records to show the restrictions were in their best interests.
414/
414/
People's benefits had been used to pay for vehicles the provider had leased on their behalf.
The charges to people included a fee for a tracking device on each vehicle, related to the vehicle insurance.
415/
The charges to people included a fee for a tracking device on each vehicle, related to the vehicle insurance.
415/
There were no records of people's consent or why the decisions for people to pay for these things were in their best interests.
The provider had not ensured senior staff had a comprehensive understanding of the MCA.
416/
The provider had not ensured senior staff had a comprehensive understanding of the MCA.
416/
They did not understand the need for best interests' decisions to be completed regarding the costs people were charged for the vehicles they used.
This was a breach of regulation 11 (Consent) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
417/
This was a breach of regulation 11 (Consent) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
417/
[Caring - requires improvement]
Staff did not always promote people's independence.
[Which should in no way be a surprise given that staff haven't been trained appropriately, and there is no leadership from the provider, and a paternalistic culture]
418/
Staff did not always promote people's independence.
[Which should in no way be a surprise given that staff haven't been trained appropriately, and there is no leadership from the provider, and a paternalistic culture]
418/
When people went to the shops, staff generally took money out of the person's cash box which was kept in the office, and then held the money for them until they wanted to pay for something.
People's care plans guided staff to do this.
419/
People's care plans guided staff to do this.
419/
People's care plans did not detail how staff could support them to increase their independence.
The service had identified that one person could be supported to take more control regarding their own money.
420/
The service had identified that one person could be supported to take more control regarding their own money.
420/
However, for the other people, there were no plans in place to support them to have greater autonomy over their money.
This was part of a breach of regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
421/
This was part of a breach of regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
421/
Staff knew when people needed their space and privacy and respected this.
People received kind and compassionate care from staff.
[I struggle with this statement. Earlier in the report they identified a closed, paternalistic culture... that's not kind or compassionate]
422/
People received kind and compassionate care from staff.
[I struggle with this statement. Earlier in the report they identified a closed, paternalistic culture... that's not kind or compassionate]
422/
People's care and support was not designed holistically around each person.
People were supported to make day to day decisions about how they spent their time but were provided with limited opportunities to be involved in making meaningful decisions about their future.
423/
People were supported to make day to day decisions about how they spent their time but were provided with limited opportunities to be involved in making meaningful decisions about their future.
423/
People had individualised tools to help them communicate. Their care plans detailed how to recognise if someone was not happy with something.
This helped reduce the likelihood the person would need to use their behaviour to communicate.
424/
This helped reduce the likelihood the person would need to use their behaviour to communicate.
424/
Staff were patient and engaged people in daily tasks and activities.
When people had received the right support to communicate their views, these had been respected.
[When]
425/
When people had received the right support to communicate their views, these had been respected.
[When]
425/
One person's care plan recorded that they still had some concerns about the pandemic, so staff would review college and work opportunities with them again in a couple of months.
[By which time they'll have missed the start of term. No forward planning]
426/
[By which time they'll have missed the start of term. No forward planning]
426/
Staff treated people well and during the inspection people were at ease and happy.
A relative confirmed their family member was happy and settled at the service.
[Which one, the one not allowed to listen to music, or the one having tokens taken away from them?]
427/
A relative confirmed their family member was happy and settled at the service.
[Which one, the one not allowed to listen to music, or the one having tokens taken away from them?]
427/
Staff showed they valued people by staff treating them with respect and showing a genuine interest in their well-being.
[Hmmmmm. Star charts. Tokens. Treating with respect. These sentences make no sense]
428/
[Hmmmmm. Star charts. Tokens. Treating with respect. These sentences make no sense]
428/
At our last inspection we found staffing levels had impacted on people's opportunities.
This contributed to a continued breach of regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
[Continued breach, last time...]
429/
This contributed to a continued breach of regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
[Continued breach, last time...]
429/
At this inspection we found improvements had been made but further improvements were still required.
Activities and how people spent their time were not always part of a holistic plan to ensure they lived a meaningful life.
430/
Activities and how people spent their time were not always part of a holistic plan to ensure they lived a meaningful life.
430/
People did not have complete freedom of choice and control over what they did and their opportunities to make spontaneous decisions about how they spent their time were limited.
[Are you living if you don't have the opportunity to be spontaneous? Is that not essential?]
431/
[Are you living if you don't have the opportunity to be spontaneous? Is that not essential?]
431/
Staff tried to ensure people were able to do the things they liked and chose; however, one staff member told us it was difficult to juggle people's activities and needs when they were short staffed.
[And they wonder whey they can't fill their staffing vacancies]
432/
[And they wonder whey they can't fill their staffing vacancies]
432/
People's records showed that at times, people had become upset because they were unable to spend their time how they wanted to due to a lack of staff or vehicles.
People did not lead fully inclusive or empowered lives.
433/
People did not lead fully inclusive or empowered lives.
433/
Records of how people spent their time showed that where people went was often dependent on what other people were doing that day.
People would often go to drop another person and their staff member off at an activity and then continue on to a different location.
434/
People would often go to drop another person and their staff member off at an activity and then continue on to a different location.
434/
They would then have to return at the correct time to pick up the person and staff member they had dropped off.
This did not show people's care was personalised and designed around the individual.
[No chance to be spontaneous, or change your plans at the last minute]
435/
This did not show people's care was personalised and designed around the individual.
[No chance to be spontaneous, or change your plans at the last minute]
435/
This formed part of a continued breach of regulation 18 (Staffing) of Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
[So many continued breaches. How long are people expected to live these non-lives? How many years is it acceptable to be wasted?]
436/
[So many continued breaches. How long are people expected to live these non-lives? How many years is it acceptable to be wasted?]
436/
People did not always receive person centred care.
Items that belonged to them were sometimes stored in the office or locked away.
[It's bad enough that there's an office in someone's home, but then to use it to deny, to lock away, just awful]
437/
Items that belonged to them were sometimes stored in the office or locked away.
[It's bad enough that there's an office in someone's home, but then to use it to deny, to lock away, just awful]
437/
For example, one person's bottle of wine, a key to unlock a cupboard that contained another person's radio, and people's money was kept in cash boxes in the office.
People had not been consulted about whether they were happy with this arrangement.
438/
People had not been consulted about whether they were happy with this arrangement.
438/
Records showed that on one occasion, one person had accompanied staff to take another staff member to work at a different Spectrum service in the car people were paying for.
[Time and again. Happened in an earlier report of another service too]
439/
[Time and again. Happened in an earlier report of another service too]
439/
This showed the service was not focused on meeting people's individual preferences and decisions but had prioritised the needs of the provider.
[Everything about @ASDspectrumASD seems to prioritise the needs of the provider. Poor charitable provision, again]
440/
[Everything about @ASDspectrumASD seems to prioritise the needs of the provider. Poor charitable provision, again]
440/
People enjoyed the things they spent their time doing; however, there was little evidence staff had used person-centred planning tools and approaches to understand what a meaningful life looked like for each person.
441/
441/
This meant people's choices were limited to things they already knew, and opportunities staff sought to offer people reflected only their prior knowledge of what the person liked.
442/
442/
This contributed to the breach of regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
443/
443/
[Well-led - inadequate]
At our last inspection we rated this key question requires improvement.
At this inspection the rating has changed to inadequate.
This meant there were widespread and significant shortfalls in service leadership.
444/
At our last inspection we rated this key question requires improvement.
At this inspection the rating has changed to inadequate.
This meant there were widespread and significant shortfalls in service leadership.
444/
Leaders and the culture they created did not assure the delivery of high-quality care.
At this inspection we checked if the provider had met the requirements of the warning notice we previously served in relation to the governance of the service.
445/
At this inspection we checked if the provider had met the requirements of the warning notice we previously served in relation to the governance of the service.
445/
We found the required improvements had not been made.
At the last inspection we found the provider had failed to continually assess, monitor and drive improvement in the quality and safety of the services provided.
446/
At the last inspection we found the provider had failed to continually assess, monitor and drive improvement in the quality and safety of the services provided.
446/
This was a continued breach of regulation 17 (Good governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
Not enough improvement had been made at this inspection and the provider was still in breach of regulation 17.
447/
Not enough improvement had been made at this inspection and the provider was still in breach of regulation 17.
447/
Our findings from the other key questions showed the provider's governance processes were ineffective and had not resulted in people consistently receiving good quality care and support based on best practice.
448/
448/
The providers systems and processes to assess, monitor and improve the quality and safety of the service were not operating effectively.
The registered manager completed a monthly checklist to advise the provider of outstanding actions needed at the service.
449/
The registered manager completed a monthly checklist to advise the provider of outstanding actions needed at the service.
449/
However, the checklist did not always reflect correct information about the service.
Due to a lack of oversight of the service, the provider had not identified the checklist was incorrect.
[Total apathy]
450/
Due to a lack of oversight of the service, the provider had not identified the checklist was incorrect.
[Total apathy]
450/
The registered manager completed monthly checks of people's expenditure to help ensure staff were handling people's money safely.
However, the provider did not check these were correct as all receipts stayed in the service.
[This is utterly bizarre]
451/
However, the provider did not check these were correct as all receipts stayed in the service.
[This is utterly bizarre]
451/
An environmental assessment of the service to check if it met the needs of autistic people had not been used to good effect.
One question answered that as people received one to one support from staff, their needs would be met if they wanted to leave the service.
452/
One question answered that as people received one to one support from staff, their needs would be met if they wanted to leave the service.
452/
This was not reflective of the current staffing levels at the service and was therefore incorrect.
During the inspection, two people did not have one to one support, they were sharing one staff member.
[A half life, at best]
453/
During the inspection, two people did not have one to one support, they were sharing one staff member.
[A half life, at best]
453/
The rota showed this happened regularly and meant the people would not always be able to leave the service with one to one support as the assessment suggested.
Action had not always been taken promptly to assess or improve people's lives.
454/
Action had not always been taken promptly to assess or improve people's lives.
454/
The same assessment noted,
"To further support our understanding of the residents' sensory needs we will complete an outline of the sensory behavioural scale for each individual."
This had not been completed.
455/
"To further support our understanding of the residents' sensory needs we will complete an outline of the sensory behavioural scale for each individual."
This had not been completed.
455/
There were several warning signs of a closed culture in the service; such as the use of potentially punitive approaches, restrictions being used without an assessment of need and blanket restrictions in place that were not necessarily the least restrictive.
456/
456/
There was no system in place to monitor the service to help ensure a closed culture had not developed.
Information we requested from the provider about the management of people's benefits and finances was not all provided.
457/
Information we requested from the provider about the management of people's benefits and finances was not all provided.
457/
This was a continued breach of continued Regulation 17 (Good Governance) of The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
458/
458/
Following the inspection, the provider told us governance processes were being revised.
They also told us care planning documentation was being revised.
[Future future, always future, stagnated half lives on hold]
459/
They also told us care planning documentation was being revised.
[Future future, always future, stagnated half lives on hold]
459/
There was limited evidence of the provider's ability to drive improvement at the service.
At an inspection in June 2021 we imposed conditions on the provider's registration to report to us on a monthly basis about staffing levels.
460/
At an inspection in June 2021 we imposed conditions on the provider's registration to report to us on a monthly basis about staffing levels.
460/
This enforcement action is intended to drive improvement at the service; however, at the last inspection (November 2021) and this inspection, we had ongoing concerns about staffing.
[Guess the enforcement action aint working; its not driving improvements, so shut it down]
461/
[Guess the enforcement action aint working; its not driving improvements, so shut it down]
461/
This meant this was the third consecutive time the service had been in breach of the regulations in relation to staffing.
[How many more. Who would want to work for this provider]
462/
[How many more. Who would want to work for this provider]
462/
At the last inspection we served a warning notice for failures in governance; however, at this inspection we had ongoing concerns and found the warning notice had not been met.
The provider had failed to use the findings from our previous inspections to drive improvements.
463/
The provider had failed to use the findings from our previous inspections to drive improvements.
463/
The service has been rated below Good since May 2018 but the provider has not made the required improvements to the service.
[Over 4 years]
The registered manager was keen to improve the service but had not received the outcome of a provider level audit of the service.
464/
[Over 4 years]
The registered manager was keen to improve the service but had not received the outcome of a provider level audit of the service.
464/
This meant the registered manager had not received the correct support, advice and guidance to identify and implement best practice and the required improvements.
465/
465/
A staff member told us,
"It is very disheartening when we get a poor rating because we try our best, but we get requires improvement because of the lack of support from head office. They never come in and see."
[Can you imagine. Another inadequate report, zero leadership]
466/
"It is very disheartening when we get a poor rating because we try our best, but we get requires improvement because of the lack of support from head office. They never come in and see."
[Can you imagine. Another inadequate report, zero leadership]
466/
Staff knew people well, however the provider had not ensured they had a good understanding of best practice models of care.
This meant staff did not consistently support people's aspirations to live a quality life of their choosing.
467/
This meant staff did not consistently support people's aspirations to live a quality life of their choosing.
467/
The ethos and culture of the service were paternalistic which limited the opportunities people were offered.
Last inspection we were told the provider was developing their auditing system to ensure it was aligned to principles of Right support, right care, right culture.
468/
Last inspection we were told the provider was developing their auditing system to ensure it was aligned to principles of Right support, right care, right culture.
468/
These had not been effective as aspects of the service still did not reflect these principles.
[Future promises. Meaningless future promises]
469/
[Future promises. Meaningless future promises]
469/
This was part of a continued breach of continued Regulation 17 (Good Governance) of The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014
470/
470/
The providers systems and processes had not identified that the model of care provided at Heightlea did not reflect best practice.
This meant people's lives and opportunities were limited.
471/
This meant people's lives and opportunities were limited.
471/
The provider had not ensured the service consistently achieved good outcomes for people in all areas of their lives.
How people spent their time was still at times, dictated by staffing levels and vehicles available and, as a result, was not always person centred.
472/
How people spent their time was still at times, dictated by staffing levels and vehicles available and, as a result, was not always person centred.
472/
The provider had not monitored the culture in the service to ensure it was truly inclusive and empowered people to develop and flourish.
[The provider was so far from doing any meaningful monitoring]
473/
[The provider was so far from doing any meaningful monitoring]
473/
People enjoyed their day to day activities and pastimes but there was no evidence of people being supported to describe or explore what a meaningful life meant for them or to make plans on how to reach their goals and aspirations.
474/
474/
There was an overly restrictive culture in the service which meant people did not always have free access to key aspects of their lives.
Restrictions were placed on people that had not been assessed as necessary or the least restrictive option.
475/
Restrictions were placed on people that had not been assessed as necessary or the least restrictive option.
475/
This was part of a continued breach of continued Regulation 17 (Good Governance) of The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
476/
476/
The registered manager knew people well, was approachable and took a genuine interest in what people, staff, family, advocates and other professionals had to say.
A relative told us
"[Registered manager] is the rock of the service. We have a very high opinion of them."
477/
A relative told us
"[Registered manager] is the rock of the service. We have a very high opinion of them."
477/
The registered manager encouraged staff to reflect on and challenge the way they supported people and welcomed new ideas.
478/
478/
Staff were committed to reviewing people's care and support on an ongoing basis to ensure it continued to reflect people's needs and wishes as they changed over time.
479/
479/
A relative told us they were happy with the service provided to their family member adding, "We think [registered manager] and the team do a really good job."
Staff valued their relationships with the people they supported.
480/
Staff valued their relationships with the people they supported.
480/
When we asked staff to describe achievements of the service, they were keen to describe what each individual had achieved; this included college courses, one off trips such as going to watch Abba, as well as supporting people back into work placements.
481/
481/
Staff told us they were well supported by the registered manager but not by the provider.
Comments included,
"I feel valued by the manager, but I don't from head office" and....
482/
Comments included,
"I feel valued by the manager, but I don't from head office" and....
482/
"We do everything we can but it's with the head office where the issue is."
[Aint that the perfect quote to end on. State of this provider. Honestly. That's it for Heightlea.
There's one more report, will try to get to it tonight. Need to feed the dog/cat now]
483/ tbc
[Aint that the perfect quote to end on. State of this provider. Honestly. That's it for Heightlea.
There's one more report, will try to get to it tonight. Need to feed the dog/cat now]
483/ tbc
Carrick @ASDspectrumASD inadequate api.cqc.org.uk/public/v1/repo…
Carrick is a residential care home providing personal care and accommodation for up to five people with learning disabilities or who are autistic.
Five people lived at the service at the time of this inspection.
484/
Carrick is a residential care home providing personal care and accommodation for up to five people with learning disabilities or who are autistic.
Five people lived at the service at the time of this inspection.
484/
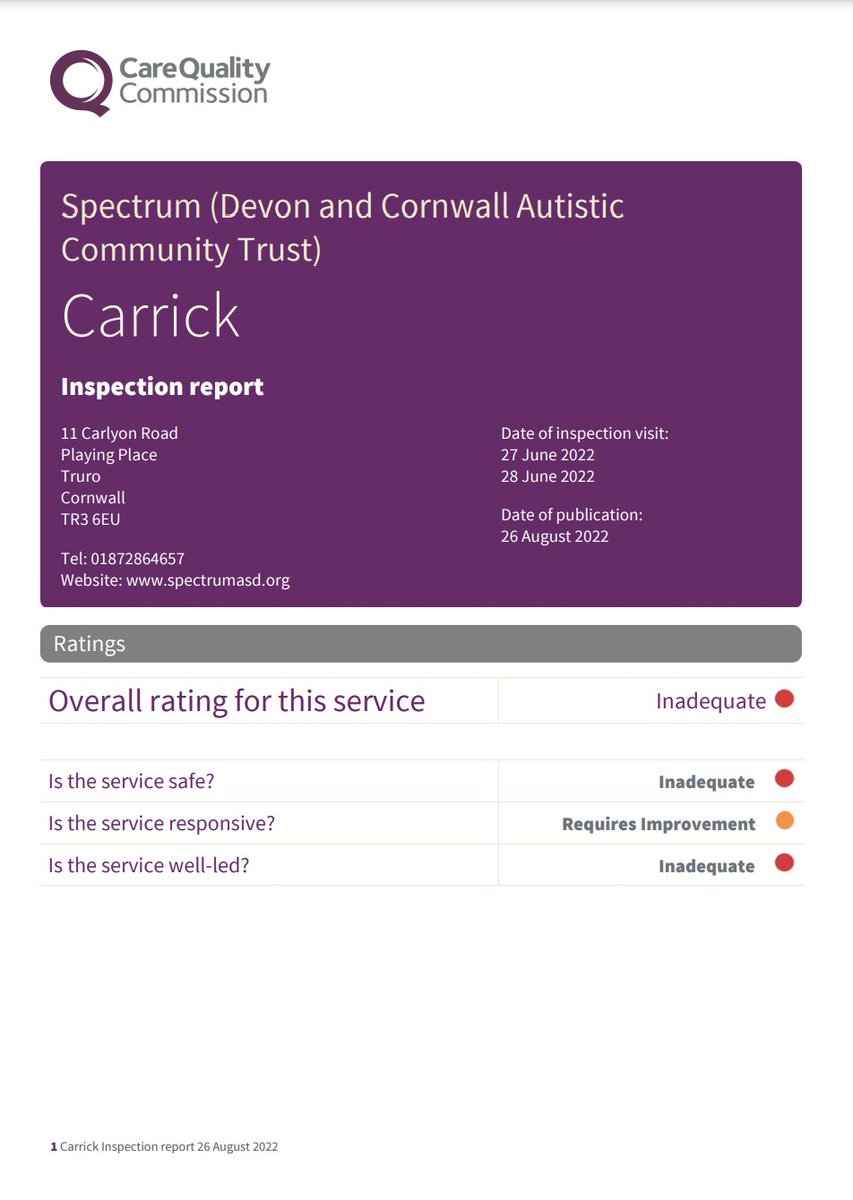
One person had their own self-contained accommodation and the remaining four people lived in the main house.
The service is part of the Spectrum group who run similar services throughout Cornwall
485/
The service is part of the Spectrum group who run similar services throughout Cornwall
485/
The service was not able to demonstrate how they were meeting all of the underpinning principles of the statutory guidance Right Support, Right Care, Right Culture.
486/
486/
One person's support needs had significantly increased, and this had impacted on other people's safety and well-being.
Prior to the new manager's arrival in the week prior to the inspection, staff had not received appropriate support and guidance...
487/
Prior to the new manager's arrival in the week prior to the inspection, staff had not received appropriate support and guidance...
487/
...to help them meet this person's needs.
The numbers of staff on duty each day had increased since the last inspection and in the month prior to the inspection the staffing numbers had been safe.
However, staffing arrangements at Carrick remained challenging.
488/
The numbers of staff on duty each day had increased since the last inspection and in the month prior to the inspection the staffing numbers had been safe.
However, staffing arrangements at Carrick remained challenging.
488/
The service had significant numbers of staff vacancies and had been unable to recruit additional staff.
The service had become dependent on a small group of agency staff to achieve the required staffing levels.
[Why would anyone want to work for this provider?]
489/
The service had become dependent on a small group of agency staff to achieve the required staffing levels.
[Why would anyone want to work for this provider?]
489/
These agency staff continued to be permitted to work excessive hours each week and had regularly worked over 84 hours per week with limited opportunities for rest.
These working practices exposed people and the staff to ongoing risk of harm.
490/
These working practices exposed people and the staff to ongoing risk of harm.
490/
The provider had not made sure that necessary, pre employment checks had been completed for agency staff working in the service.
People were protected from abuse. Appropriate referrals had been made to the local authority when significant incidents occurred.
491/
People were protected from abuse. Appropriate referrals had been made to the local authority when significant incidents occurred.
491/
The new manager had a good understanding of local safeguarding procedures.
Medicines were not managed safely.
Records were incomplete and it was not possible to establish if people had received their medicines as prescribed.
[So dangerous]
492/
Medicines were not managed safely.
Records were incomplete and it was not possible to establish if people had received their medicines as prescribed.
[So dangerous]
492/
Staff skills in relation to medicine had not been regularly assessed.
Additional training had not been provided to staff on how to meet people's communication needs.
This continued to limit opportunities for people to participate in decision making.
493/
Additional training had not been provided to staff on how to meet people's communication needs.
This continued to limit opportunities for people to participate in decision making.
493/
Access to the community had improved for people since the last inspection.
People had been offered regular opportunities to go out and people were being supported to engage in more activities.
494/
People had been offered regular opportunities to go out and people were being supported to engage in more activities.
494/
Sensory items were available to people in the lounge and plans were being developed to improve access to the garden.
[Still planning]
The culture of the service remains of concern.
495/
[Still planning]
The culture of the service remains of concern.
495/
There was no registered manager in post and limited leadership support had been provided prior to the new manager's arrival in the week prior to our inspection.
496/
496/
This, in combination with the small number of agency staff regularly working excessive hours, meant there was a risk of a closed culture developing.
This had not been identified and there were no plans in place to mitigate the risk.
497/
This had not been identified and there were no plans in place to mitigate the risk.
497/
The provider has again failed to demonstrate to the commission that there were appropriate systems in place to ensure people were protected from financial abuse.
We have shared our concerns in relation to this issue with the local authority.
498/
We have shared our concerns in relation to this issue with the local authority.
498/
[It's odd, people's non-lives tolerated for years, but it seems it is only the financial mismanagement that gets @ChtyCommission engaged]
The provider's quality assurance systems had failed to ensure the service achieved compliance with the requirement of the regulations.
499/
The provider's quality assurance systems had failed to ensure the service achieved compliance with the requirement of the regulations.
499/
The new manager had impacted positively on staff morale.
[Except the new manager is not full time permanent in post. In this complete vacuum of leadership its not surprising staff are impressed, but its a sticking plaster on a gaping wound]
500/
[Except the new manager is not full time permanent in post. In this complete vacuum of leadership its not surprising staff are impressed, but its a sticking plaster on a gaping wound]
500/
Staff were complimentary of the new manager's approach and told us,
"I have been really impressed with the manager, she is really nice and is a good manager. I know they are looking for a full-time manager and I hope we get someone like that."
[Lives lived on hope]
501/
"I have been really impressed with the manager, she is really nice and is a good manager. I know they are looking for a full-time manager and I hope we get someone like that."
[Lives lived on hope]
501/
The new manager had a good understanding of the Mental capacity act and appropriate applications had been made to the local authority for the authorisation of potentially restrictive care plans.
502/
502/
The last rating for this service was Inadequate. (Report published 17 May 2022). Breaches of the regulations were identified.
At this inspection we found not enough improvements had been made and the provider was still in breach of the regulations.
503/
At this inspection we found not enough improvements had been made and the provider was still in breach of the regulations.
503/
We received concerns in relation to a significant increase in the number of incidents occurring in the service.
A decision was made for us to inspect and examine those risks and the performance of the service.
504/
A decision was made for us to inspect and examine those risks and the performance of the service.
504/
We have again found evidence that the provider needs to make improvements.
We have identified breaches in relation to Person centred care, Safe care and treatment, Safeguarding, Staffing, Governance and the Fitness of staff to work at this inspection.
505/
We have identified breaches in relation to Person centred care, Safe care and treatment, Safeguarding, Staffing, Governance and the Fitness of staff to work at this inspection.
505/
The service did not have a manager registered with the Care Quality Commission.
However, a manager, registered at another service operated by the provider, was leading the service at the time of this inspection.
This inspection was unannounced.
506/
However, a manager, registered at another service operated by the provider, was leading the service at the time of this inspection.
This inspection was unannounced.
506/
[Safe - inadequate]
At the last inspection we found restrictions to people's freedoms due to the availability of vehicles had increased the risk of incidents occurring which exposed people to risk of harm.
507/
At the last inspection we found restrictions to people's freedoms due to the availability of vehicles had increased the risk of incidents occurring which exposed people to risk of harm.
507/
This was a breach of Regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
At this inspection vehicles were available to enable people to access the community. However...
508/
At this inspection vehicles were available to enable people to access the community. However...
508/
...there had been a significant increase in one person's support needs which had impacted adversely on the other people living in the service.
This meant the service remains in breach of the regulation.
509/
This meant the service remains in breach of the regulation.
509/
This inspection was completed in response to a number of notifications, received from the service, detailing incidents of aggression and violence between people who lived there.
[Already feel like screaming, shut it down]
510/
[Already feel like screaming, shut it down]
510/
The information provided did not give enough assurance that action was being taken to ensure people were safe at Carrick.
Last inspection we noted there had been a reduction in number of incidents involving one person following changes in how their support was provided.
511/
Last inspection we noted there had been a reduction in number of incidents involving one person following changes in how their support was provided.
511/
In the period following that inspection, this person's support needs had increased significantly.
Incidents had occurred where the person had harmed themselves and others.
512/
Incidents had occurred where the person had harmed themselves and others.
512/
On the first day of our inspection staff told us this person had been upset for four and a half hours earlier in the day.
Incident and daily care records showed the person had experienced high levels of incidents throughout June.
[And what support was put in place?]
513/
Incident and daily care records showed the person had experienced high levels of incidents throughout June.
[And what support was put in place?]
513/
There was limited evidence available to show what additional support had been provided or changes made to how the service operated in response to these changes in the person's needs.
514/
514/
During the second day of our inspection people attempted to avoid spending time with another person the service supported and exhibited signs of anxiety and possibly fear in response to their actions.
[Living under constant anxiety and fear... recipe for PTSD]
515/
[Living under constant anxiety and fear... recipe for PTSD]
515/
Staff recognised that the actions of individuals could impact on the wellbeing of others the service supported.
Staff reported people had been upset and distressed by other actions and that they felt some people were no longer comfortable in their own home.
516/
Staff reported people had been upset and distressed by other actions and that they felt some people were no longer comfortable in their own home.
516/
Prior to the arrival of the new acting manager, a week prior to the inspection, there was limited evidence that additional support, guidance or training had been provided to the staff team to enable them to meet this person's increased needs.
517/
517/
Some staff had become fearful for their safety and lacked confidence in their ability to meet people's needs.
Accidents and incidents had been appropriately documented via the provider's digital reporting system.
518/
Accidents and incidents had been appropriately documented via the provider's digital reporting system.
518/
These records had been reviewed by the provider's behavioural team.
Prior to the new manager's arrival comments had been added to these records demonstrating they had been reviewed.
[Performative scrutiny]
519/
Prior to the new manager's arrival comments had been added to these records demonstrating they had been reviewed.
[Performative scrutiny]
519/
However, this had not led to additional support and guidance being provided to the staff team in response to the significant increase in one person's incidents and the harm caused to themselves and others.
[Pointless paperwork]
520/
[Pointless paperwork]
520/
When staff had been involved in particularly complex incidents, limited additional guidance and support had been provided to help them process and learn from their experiences.
521/
521/
Staff told us this lack of support had impacted on both their confidence and ability to meet people's needs.
The provider had failed to take timely and appropriate action to manage risk associated with changes in people's support needs.
522/
The provider had failed to take timely and appropriate action to manage risk associated with changes in people's support needs.
522/
This was a breach of the requirement of Regulation 12 (Safe care and treatment) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
523/
523/
The new acting manager was an experienced member of the provider's team who had begun working in the service in the week prior to our inspection.
[Fragile, all so fragile, the new manager only in place for a week... a week, what happened before then?]
524/
[Fragile, all so fragile, the new manager only in place for a week... a week, what happened before then?]
524/
Following their arrival in the service, the new manager had successfully sought support and practical guidance for staff from the provider's behavioural team.
On the second day of the inspection one of the provider's behaviour team was present in the service.
525/
On the second day of the inspection one of the provider's behaviour team was present in the service.
525/
They were shadowing staff while attempting to gain a better understanding of the meanings of the person's specific behaviours and to differentiate between actions taken to meet sensory needs and those actions which indicted the person was upset or anxious.
526/
526/
Staff were engaging positively with the support and guidance provided and told us,
"We are working together more as a team, we are moving forward, taking what we have been told and moving with it".
[A week]
527/
"We are working together more as a team, we are moving forward, taking what we have been told and moving with it".
[A week]
527/
As the support had not been in place in a timely fashion, this approach had not been implemented for long enough to assess whether it would sustainably reduce the risk of harm.
528/
528/
There were two vehicles available to enable people to access the community.
The issue, which at the last inspection had restricted people's access to these vehicles, had been resolved and there were staff available on most shifts who were able to drive.
529/
The issue, which at the last inspection had restricted people's access to these vehicles, had been resolved and there were staff available on most shifts who were able to drive.
529/
One staff member told us, "At the moment we have three drivers plus one additional driver when [staff member's name] returns".
At the last inspection we found risks in relation to scalding and hot water temperatures had not been appropriately managed.
530/
At the last inspection we found risks in relation to scalding and hot water temperatures had not been appropriately managed.
530/
This was a part of breach of Regulation 12 (Safe care and treatment) of Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
At this inspection these issues had been addressed and the service was no longer in breach of this aspect of the regulations.
531/
At this inspection these issues had been addressed and the service was no longer in breach of this aspect of the regulations.
531/
[It is mind boggling to me that anyone can have failed to manage risks around scalding and hot water; so great that they're now being addressed, for now, but seriously how dire is this provider]
532/
532/
At the last two inspection we found agency staff were working excessive hours and routinely completing six, 14-hour shift each week.
Such long working hours represent an inherent risk to people and the staff who supported them.
533/
Such long working hours represent an inherent risk to people and the staff who supported them.
533/
This was a breach of Regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
At this inspection, agency staff were continuing to work excessive numbers of hours.
534/
At this inspection, agency staff were continuing to work excessive numbers of hours.
534/
This exposed people to ongoing risk of harm and meant the service remains in breach of the regulation.
The provider continues to experience significant staff recruitment challenges and no new staff had been recruited since our last inspection.
535/
The provider continues to experience significant staff recruitment challenges and no new staff had been recruited since our last inspection.
535/
Rotas showed there were six and a half full time staff vacancies at Carrick at the time of the inspection.
Agency staff were regularly working in the service.
Agency staff routinely worked six, 14-hour shifts each week.
536/
Agency staff were regularly working in the service.
Agency staff routinely worked six, 14-hour shifts each week.
536/
Staff working these excessive hours meant people and the staff members themselves were exposed to risk of harm.
[This provider isn't fit for purpose. They can't recruit adequate staff for any of their services. They're the common denominator]
537/
[This provider isn't fit for purpose. They can't recruit adequate staff for any of their services. They're the common denominator]
537/
We again identified an occasion were an agency staff member had worked 96 hours in a single week and two other occasions where agency staff members completed 14-hour care shifts on eight consecutive days.
538/
538/
Working these excessive hours was unsafe and as it impacted on both the quality of support people received and on staff's ability to rest and recharge.
539/
539/
The provider had completed risk assessments in an attempt to manage the risks associated with agency staff to working these excessive hours.
[Risk assessments don't manage risk. If no action is taken they're just performative]
540/
[Risk assessments don't manage risk. If no action is taken they're just performative]
540/
These assessments did not appropriately mitigate the risk of staff falling asleep on shift.
As noted at previous inspection when this occurred it was treated as a staff disciplinary issue as opposed to the predictable consequence of permitting staff to work excessive hours
541/
As noted at previous inspection when this occurred it was treated as a staff disciplinary issue as opposed to the predictable consequence of permitting staff to work excessive hours
541/
We noted two occasions in the month prior to the inspection where agency staff became unwell and were unable to return to work after a single rest day having completed periods of six or more consecutive 14-hour days.
542/
542/
The provider had again failed to ensure enough staff were safely deployed in order to meet people's recognised needs.
This was an ongoing breach of Regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
543/
This was an ongoing breach of Regulation 18 (Staffing) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
543/
Necessary pre employment checks had not been fully completed for staff employed by the agency and working in Carrick.
Records showed required references had not been gathered from these staff member's most recent employers in the care sector.
544/
Records showed required references had not been gathered from these staff member's most recent employers in the care sector.
544/
This meant the provider was unable to demonstrate agency staff had been recruited safely.
This was a breach of the requirements of regulation 19 (fit and proper persons) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
545/
This was a breach of the requirements of regulation 19 (fit and proper persons) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
545/
Medicines were not always managed safely. Staff supported people to take their medicines.
Medicines administration was recorded on medicines admin records (MARs) but there were gaps, so it was not possible to tell if people had received their medicines as prescribed.
546/
Medicines administration was recorded on medicines admin records (MARs) but there were gaps, so it was not possible to tell if people had received their medicines as prescribed.
546/
Staff received training on medicines handling but were not regularly assessed to make sure they had the required skills, knowledge and competence.
MARs did not contain enough information to make sure that medicines were given safely and effectively.
547/
MARs did not contain enough information to make sure that medicines were given safely and effectively.
547/
For example, to take with or after food or to swallow whole rather than chewing or crushing.
Where medicines taken on an as required basis had a maximum dose that should be taken in a 24 hour period, times were not recorded on MARs.
548/
Where medicines taken on an as required basis had a maximum dose that should be taken in a 24 hour period, times were not recorded on MARs.
548/
This meant people were at risk of taking too much medicine. However, there was no evidence that people had received more than the maximum dose.
[The absence of evidence ≠ it did not happen]
549/
[The absence of evidence ≠ it did not happen]
549/
Guidance was not always in place for some 'as required' medicines.
One person needed an 'as required' medicine to help with pain relief.
There was no guidance in place to inform staff when this person might need the medicine.
550/
One person needed an 'as required' medicine to help with pain relief.
There was no guidance in place to inform staff when this person might need the medicine.
550/
This meant the person was at risk of not get their medicine when they needed and experience unnecessary pain.
551/
551/
The provider failed to ensure that medicines administration records were accurate, that protocols were in place for 'when required' medicines and that staff were assessed as competent to deliver medicines support.
552/
552/
This was a breach of Regulation 12 (safe care and treatment) of the Health and Social care Act 2008 (Regulated Activities) Regulations 2014.
553/
553/
At the last inspection we identified concerns in relation to the management of people's financial affairs and requested more information from the provider.
This information was not provided.
554/
This information was not provided.
554/
This was a breach of Regulation 13 (Safeguarding) of Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
At this inspection we again asked for information about the management of one person's financial affairs. Some information was provided.
[Some]
555/
At this inspection we again asked for information about the management of one person's financial affairs. Some information was provided.
[Some]
555/
However, this did not provide enough assurance that the person was appropriately protected from financial abuse.
The service remains in breach of this regulation.
[Pass it to the police, and shut it down, please]
556/
The service remains in breach of this regulation.
[Pass it to the police, and shut it down, please]
556/
Whistle-blowers have previously raised with us the concerns that one person living at Carrick was being financially abused by @ASDspectrumASD.
At this inspection we asked repeatedly for details of the financial links between Spectrum and this person.
557/
At this inspection we asked repeatedly for details of the financial links between Spectrum and this person.
557/
No detailed explanation of the financial relationship between the two parties was given to us.
This issue had been raised directly with the providers chief executive, but no appropriate explanations had been provided.
[Raise it with the police]
558/
This issue had been raised directly with the providers chief executive, but no appropriate explanations had been provided.
[Raise it with the police]
558/
The commission remains concerned that this individual is exposed to the ongoing risk of financial abuse.
Information gathered during this inspection indicated that this financial relationship may not been in the person's best interests.
559/
Information gathered during this inspection indicated that this financial relationship may not been in the person's best interests.
559/
As a result, we have shared this information with the local authority as a safeguarding alert.
[This is baffling. I hope that this is understatement and that it's been raised further afar than just the LA safeguarding team.
Everyone must know what is going on].
560/
[This is baffling. I hope that this is understatement and that it's been raised further afar than just the LA safeguarding team.
Everyone must know what is going on].
560/
The provider failed to provide the requested information about the management arrangements for this person's finances meant it was not possible to establish they were protected from financial abuse.
561/
561/
This was an ongoing breach of Regulation 13 (Safeguarding) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
562/
562/
The local authority had recently taken on responsibility for managing two people's finances.
This had impacted on systems for supporting them to make withdrawals from the bank.
[In another service, staff had left so ppl couldn't access their money. State of it]
563/
This had impacted on systems for supporting them to make withdrawals from the bank.
[In another service, staff had left so ppl couldn't access their money. State of it]
563/
As a result, the provider was having to lend these individuals money to enable them to participate in activities and make day to day purchases.
At last two inspections people were not always protected from the risk of harm as necessary safeguarding alerts had not been made
564/
At last two inspections people were not always protected from the risk of harm as necessary safeguarding alerts had not been made
564/
This was a breach of Regulation 13 (Safeguarding) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
At this inspection we found safeguarding alerts had been appropriately made. This meant the service was no longer in breach of this regulation.
565/
At this inspection we found safeguarding alerts had been appropriately made. This meant the service was no longer in breach of this regulation.
565/
A number of incidents had occurred between people living in the service since the last inspection.
These incidents had been appropriately referred to the local authority as safeguarding alerts.
566/
These incidents had been appropriately referred to the local authority as safeguarding alerts.
566/
The new manager had a good understanding of safeguarding procedures and had sufficient confidence to make alerts to the local authority independently. Staff also understood their role in ensuring people were protected from abuse.
567/
567/
[I'm not sure calling the temporary stand in, "the new manager" is really that sensible.
Given staff have been explicit this is a temporary solution.
There is no registered manager for this service. So great as a good temporary manager is, they're not the solution]
568/
Given staff have been explicit this is a temporary solution.
There is no registered manager for this service. So great as a good temporary manager is, they're not the solution]
568/
The new manager had a good understanding of the MCA and recognised the importance of enabling people to make meaningful decisions and choices.
[See above. The temporary stand-in manager, is not really "the new manager" and their knowledge of the MCA will leave with them]
569/
[See above. The temporary stand-in manager, is not really "the new manager" and their knowledge of the MCA will leave with them]
569/
[Responsive - requires improvement]
At the last inspection, the provider had failed to meet people's communication needs which restricted their ability to participate in decision making.
570/
At the last inspection, the provider had failed to meet people's communication needs which restricted their ability to participate in decision making.
570/
This contributed to the breach of the requirements of regulation 9 (Person centred care) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
571/
571/
At this inspection we found no action had been taken to address this situation and additional training in communication techniques had not been provided to staff.
The service remains in breach of the regulation.
[Another repeated breach]
572/
The service remains in breach of the regulation.
[Another repeated breach]
572/
During our last two inspections, we identified that staff needed additional training and support to meet people's communication needs.
The provider had previously recognised this training was required and stated it would be provided in 2021.
[Providers' false promises]
573/
The provider had previously recognised this training was required and stated it would be provided in 2021.
[Providers' false promises]
573/
At this inspection, Staff had again not received any additional training in the use of signs to facilitate communication.
We noted no increase in the use of signs or other aids to meet the communication needs of people living in the main part of Carrick.
574/
We noted no increase in the use of signs or other aids to meet the communication needs of people living in the main part of Carrick.
574/
The provider had again failed to provide staff with the skills, they recognised as necessary to meet people's communication needs.
This meant the service remained in breach of regulation 9 (Person centred care) of the Health and Social Care Act 2008
575/
This meant the service remained in breach of regulation 9 (Person centred care) of the Health and Social Care Act 2008
575/
At the last inspection people were not being supported to engage with activities and live meaningful lives like ordinary members of society.
This contributed to the breach of the requirements of regulation 9 (Person centred care) of the Health and Social Care Act 2008
576/
This contributed to the breach of the requirements of regulation 9 (Person centred care) of the Health and Social Care Act 2008
576/
At this inspection, we found people were now more regularly being supported to leave the service. The service is no longer in breach of this part of the regulation.
However, further improvements in relation to staff practices are required.
577/
However, further improvements in relation to staff practices are required.
577/
During this inspection, we again observed periods of minimal engagement by staff with the people they were supporting in the service's communal areas.
578/
578/
People spent significant periods of the day in the service's lounge with limited support from staff to engage in meaningful activities.
Staff did not always enable people to participate in decision making.
579/
Staff did not always enable people to participate in decision making.
579/
When a film, one person was enjoying ended, staff spent time channel surfing without involving the people present in deciding what to watch next.
We recommend the provider seeks advice and guidance from reputable sources on the provision of effective person-centred care.
580/
We recommend the provider seeks advice and guidance from reputable sources on the provision of effective person-centred care.
580/
At this inspection, the sensory box one person required access to was now available.
The person was able to access sensory items when they wished and engaged with this equipment at points during both days of the inspection.
[How long were they without it?]
581/
The person was able to access sensory items when they wished and engaged with this equipment at points during both days of the inspection.
[How long were they without it?]
581/
Staff reported that the re-introduction of this equipment to the lounge had not impacted adversely on others.
Daily care records showed people were now more often able to access the community.
Everyone was now being offered opportunities to go out.
[To do what exactly?]
582/
Daily care records showed people were now more often able to access the community.
Everyone was now being offered opportunities to go out.
[To do what exactly?]
582/
Staff confirmed people had been able to go out more often and told us,
"We are offering opportunities to go to the pub, woodland walk or out for a drive. [Person's name] is not interested in high end activities, we are trying to make it person centred"
[Hmmmm]
583/
"We are offering opportunities to go to the pub, woodland walk or out for a drive. [Person's name] is not interested in high end activities, we are trying to make it person centred"
[Hmmmm]
583/
"The most important thing is we are getting our service users out"
[Is it though? I mean they're not meant to be in prison, so freedom is important, sure, but staff who can't communicate well with people might not be best placed to judge how ppl want to spend their time]
584/
[Is it though? I mean they're not meant to be in prison, so freedom is important, sure, but staff who can't communicate well with people might not be best placed to judge how ppl want to spend their time]
584/
"[Person's name] needs two staff now when going out, just in case for trip hazards. [They] have been for fish and chips. It is just a pleasure for [them] to go out in the car".
[This. Is. Not. A. Life.
I love fish n chips, but that can't be one's sole source of pleasure]
585/
[This. Is. Not. A. Life.
I love fish n chips, but that can't be one's sole source of pleasure]
585/
Since the last inspection one person had been supported to join a local sports team, which they greatly enjoyed.
Plans were beginning to be developed to support people to engage with a wider range of more interesting activities.
[Beginning to be developed]
586/
Plans were beginning to be developed to support people to engage with a wider range of more interesting activities.
[Beginning to be developed]
586/
The new manager told us of their intention to develop more a person-centred approach to activities, where people would be offered opportunities to develop new skills and re-engage with their known interest.
[Good. Let's remember they're only a week in]
587/
[Good. Let's remember they're only a week in]
587/
A water sports lesson had been arranged for one person on the second day of our inspection, but this had to be postponed due to unsuitable conditions.
588/
588/
Staff and the new manager had identified alterations were needed to the service environment to enable people whose needs were changing to continue to access the service's outdoor spaces independently.
589/
589/
These issues had been raised with the provider's maintenance team and plans were being developed to improve access to and facilities in the garden.
[Remember earlier when they said at a previous inspection they'd been told X or Y would be done... hot air promises]
590/
[Remember earlier when they said at a previous inspection they'd been told X or Y would be done... hot air promises]
590/
People's care plans provided staff with guidance on how to meet their individual needs.
These lengthy documents were difficult for new or agency staff to access and understand quickly.
[Not fit fir purpose]
591/
These lengthy documents were difficult for new or agency staff to access and understand quickly.
[Not fit fir purpose]
591/
[Well-led - inadequate]
At our last inspection we found the provider had failed to address and resolve issues previously identified in relation to the management of the service, low staffing levels, excessive working hours and the accuracy of record keeping.
592/
At our last inspection we found the provider had failed to address and resolve issues previously identified in relation to the management of the service, low staffing levels, excessive working hours and the accuracy of record keeping.
592/
This was a breach of regulation 17 (Governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
593/
593/
At this inspection we again found there was no registered manager in post, that agency staff continued to be permitted to work excessive working hours and quality assurance systems remained ineffective.
This meant the provider remained in breach of the regulation.
594/
This meant the provider remained in breach of the regulation.
594/
There was no registered manager at Carrick.
The acting manager who had been responsible for the service at the time of our last inspection had left shortly after that inspection.
[Temporary solutions, don't last. Who could have predicted it]
595/
The acting manager who had been responsible for the service at the time of our last inspection had left shortly after that inspection.
[Temporary solutions, don't last. Who could have predicted it]
595/
This had meant the service had lacked effective leadership in the period between these inspections.
A registered manager from another location, operated by the provider, had agreed to take on responsibility for managing Carrick.
596/
A registered manager from another location, operated by the provider, had agreed to take on responsibility for managing Carrick.
596/
The new manager told us, "I offered to come across here, do a review and be interim manager, I started officially last Monday."
597/
597/
The new manager at Carrick intended to be based in the service three days per week and was available to give guidance and support by telephone while working in their other service.
[Potentially risking stability in both services]
598/
[Potentially risking stability in both services]
598/
Staff were complimentary of the new manager and gave positive feedback based on their initial interactions with the new manager.
[This is good. Really. It is also very new and very fragile and given the provider's apathy highly unlikely to be sustainable long term]
599/
[This is good. Really. It is also very new and very fragile and given the provider's apathy highly unlikely to be sustainable long term]
599/
Due to the temporary arrangement we were not assured the provider had ensured there was stable leadership at the service and positive approaches would be embedded and sustained.
600/
600/
The new manager recognised significant improvements were needed to enable the service to meet people's needs.
601/
601/
They had requested and had been provided support from both the provider's facilities management and positive behaviour support teams since they took on responsibility for Carrick.
602/
602/
During the inspection, we noted this support was beginning to impact positively on the service's performance, but we could not assess whether this would be embedded and sustained.
603/
603/
Staff were receiving practical guidance on how to meet people's support needs and maintenance issues were now being addressed.
Further improvements were planned to declutter and upgrade the service's outdoor spaces.
604/
Further improvements were planned to declutter and upgrade the service's outdoor spaces.
604/
The provider had also appointed three staff to other leadership roles within the service. A positive behaviour support lead and two senior carer posts had been filled.
[Check out the earlier inspection reports to see how dangerous PBS is in this organisation]
605/
[Check out the earlier inspection reports to see how dangerous PBS is in this organisation]
605/
However, there was limited evidence available to demonstrate these staff had been provided with additional training or support to enable them to fulfil these new roles.
[So internal promotion without training or support, highly unlikely to raise standards really is it]
606/
[So internal promotion without training or support, highly unlikely to raise standards really is it]
606/
The provider continued to operate a digital recording system. This system did not enable staff or the manager to view daily care records in chronological order.
[The system isn't fit for purpose. Why are they still using it?]
607/
[The system isn't fit for purpose. Why are they still using it?]
607/
Although it remained difficult to quickly identify missing care records, we found there had been an improvement in the quality and accuracy of the information recorded.
[An improvement, but not one that provided a safe, responsive and useful system for staff to use]
608/
[An improvement, but not one that provided a safe, responsive and useful system for staff to use]
608/
The provider' had failed to ensure there was a registered manager in post.
This failure contributed to the breach of regulation 17 (Governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
609/
This failure contributed to the breach of regulation 17 (Governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
609/
The provider did not demonstrate they had implemented a learning culture at the service.
The provider had continued to allow agency staff to work excessive hours as they had been unable to recruit additional permanent members of staff.
610/
The provider had continued to allow agency staff to work excessive hours as they had been unable to recruit additional permanent members of staff.
610/
These working practices continued to expose people and staff to risk of harm as detailed [in safe - above]
The provider's quality assurance systems remained ineffective and a number of repeat breaches of the regulation have been identified during this inspection.
611/
The provider's quality assurance systems remained ineffective and a number of repeat breaches of the regulation have been identified during this inspection.
611/
No additional audits of the service's performance had been completed by the provider since the February 2022 inspection.
612/
612/
Although meetings had been held at provider level about the issues identified during that inspection, no details of these meetings or any actions identified as necessary to improve the service's performance were available in the service.
[Complete apathy]
613/
[Complete apathy]
613/
Relatives were concerned that the provider was continuing to struggle to meet people's needs.
There comments included,
"I do not feel very comfortable with the place at the moment, I do not feel it is reaching the standard it should" and
614/
There comments included,
"I do not feel very comfortable with the place at the moment, I do not feel it is reaching the standard it should" and
614/
"I hope Spectrum can stabilise itself."
Staff had not been given prompt and appropriate support from the provider's behaviour team in response to the significant increase in one person's behaviours that was harming themselves and others prior to this inspection.
615/
Staff had not been given prompt and appropriate support from the provider's behaviour team in response to the significant increase in one person's behaviours that was harming themselves and others prior to this inspection.
615/
Incident records had been read and reviewed by the behavioural team and the significant increase in frequency recognised.
However, limited additional practical support or guidance had been provided.
616/
However, limited additional practical support or guidance had been provided.
616/
The provider had failed to appropriately manage agency staff working hours and to ensure compliance with the requirements of the regulations. This contributed to the breach of regulation 17 (Governance) of the Health and Social Care Act 2008
617/
617/
The culture of the service remains of concern.
There had been a lack of effective oversight by the provider since the last inspection and limited management support prior to the most recent new manager's arrival in the week prior to this inspection.
618/
There had been a lack of effective oversight by the provider since the last inspection and limited management support prior to the most recent new manager's arrival in the week prior to this inspection.
618/
The provider had recognised that additional senior managers were required to support its services.
A recruitment campaign was underway for additional regional managers to meet this need.
[Underway... one look at the CQC website and why would anyone choose to work there?]
619/
A recruitment campaign was underway for additional regional managers to meet this need.
[Underway... one look at the CQC website and why would anyone choose to work there?]
619/
The service was entirely dependent on a small number of agency staff, working excessive hours to enable people's needs to be met.
620/
620/
This combined with the lack of consistent and effective leadership in the service since the last inspection meant there was a significant risk of a closed culture developing which could significantly adversely impact on people's well-being.
621/
621/
The provider had not identified or addressed these risks.
[The provider clearly could not care less. This is wilful disregard for people's health, safety, welfare, lives.
Repeated wilful disregard, in multiple services]
622/
[The provider clearly could not care less. This is wilful disregard for people's health, safety, welfare, lives.
Repeated wilful disregard, in multiple services]
622/
We again found people's equality characteristics were not fully considered and support the provider had recognised as necessary, to enable staff to meet people's communication needs had not been provided.
623/
623/
The provider had failed to manage the risk of a closed culture developing at the service.
This contributed to the breach of regulation 17 (Governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
624/
This contributed to the breach of regulation 17 (Governance) of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014.
624/
[That's it, all four reports detailing inadequate care at latest @ASDspectrumASD services to be inspected.
There's a @ChtyCommission inspection underway. More here, on a thread about another inadequate Spectrum service
Hope others also take action]
625/
There's a @ChtyCommission inspection underway. More here, on a thread about another inadequate Spectrum service
https://twitter.com/GeorgeJulian/status/1553650001393377280
Hope others also take action]
625/
[@CareQualityComm say records of enforcement action taken will be added to reports in due course - I'll try to keep you posted.
@ChrisNInquest starts tomorrow, you can meet Chris here
Thanks, as always, to my crowdfunders chuffed.org/project/openju…]
/END
@ChrisNInquest starts tomorrow, you can meet Chris here
https://twitter.com/GeorgeJulian/status/1568253022916198402
Thanks, as always, to my crowdfunders chuffed.org/project/openju…]
/END
• • •
Missing some Tweet in this thread? You can try to
force a refresh