@DrSanjayPopat @myESMO #ESMO22 @DrSanjayPopat points out that the DFS HR is on par with the original analysis but the shape of the curves is different, especially for stage II/III 





This is not new - we see a rise in recurrence once TKI is stopped in multiple other adjuvant TKI studies. Is this suggestive of cure or just proper therapy of unidentified (micro)metastatic cancer? #ESMO22 
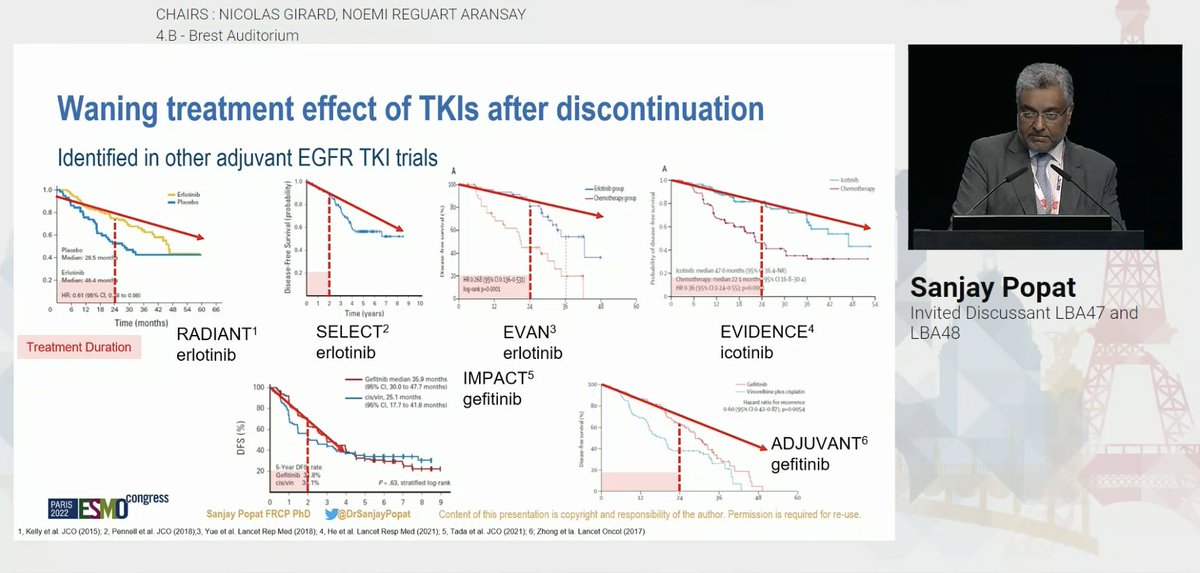
When looking at recurrence - is it on osimertinib or off osimertinib? @DrSanjayPopat also reminds us of some of the imaging limitations in ADAURA with respect to PET scans (occult metastases?) and MRI surveillance. #ESMO22 



#ESMO22 Overall, the DFS benefit is strong but there is evidence of a waning effect. Are we preventing or simply delaying recurrence? How will this impact survival? Great perspective from @DrSanjayPopat - the best in the business. #LCSM 



• • •
Missing some Tweet in this thread? You can try to
force a refresh