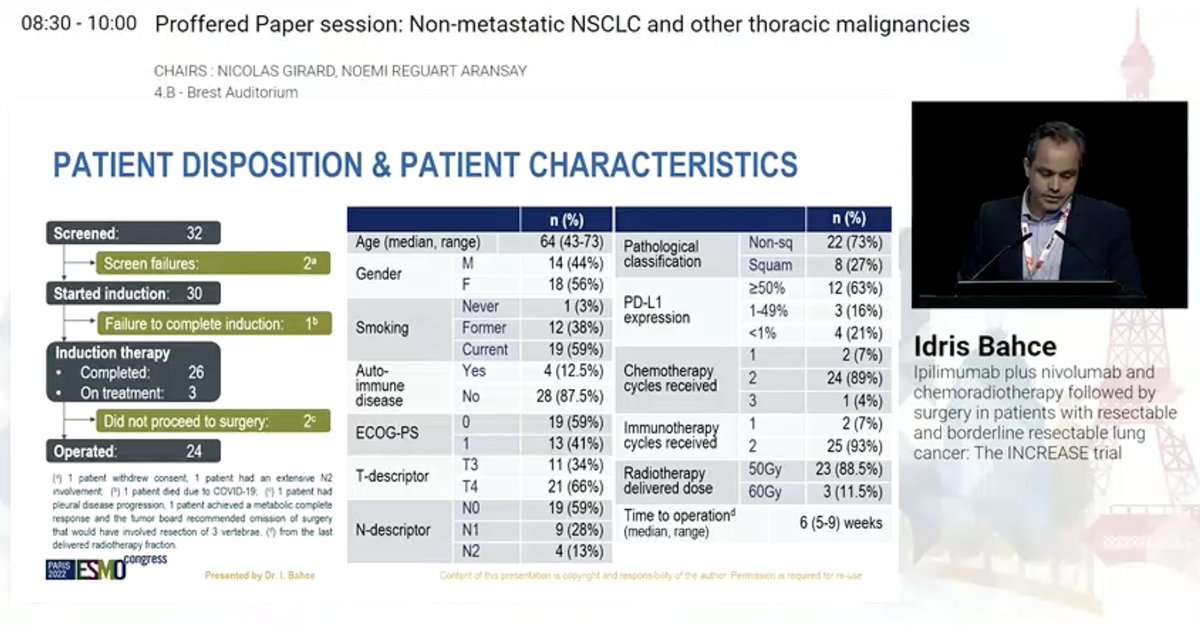
Dr. Idris Bahce presents data from the INCREASE trial - ipilimumab plus nivolumab and chemoradiation followed by surgery in resectable and borderline resectable NSCLC. #ESMO22 

Focus is on high T stage and low N stage - not resectable initially but potentially resectable after therapy. Patients here received nivo/ipi on day 1 and nivo on day 22 with chemoradiation then resection 6w later (after restaging) with pCR/MPR primary endpoint. #ESMO22 



#ESMO22 Patient disposition here - of 26 patients who completed induction therapy, 3 are still on therapy and 24 completed surgery. Included 66% T4 and 59% N0 (only 13% N2). Majority (63%) had PDL1 high disease. There was one G5 AE (COVID). No AE prevented surgery. 


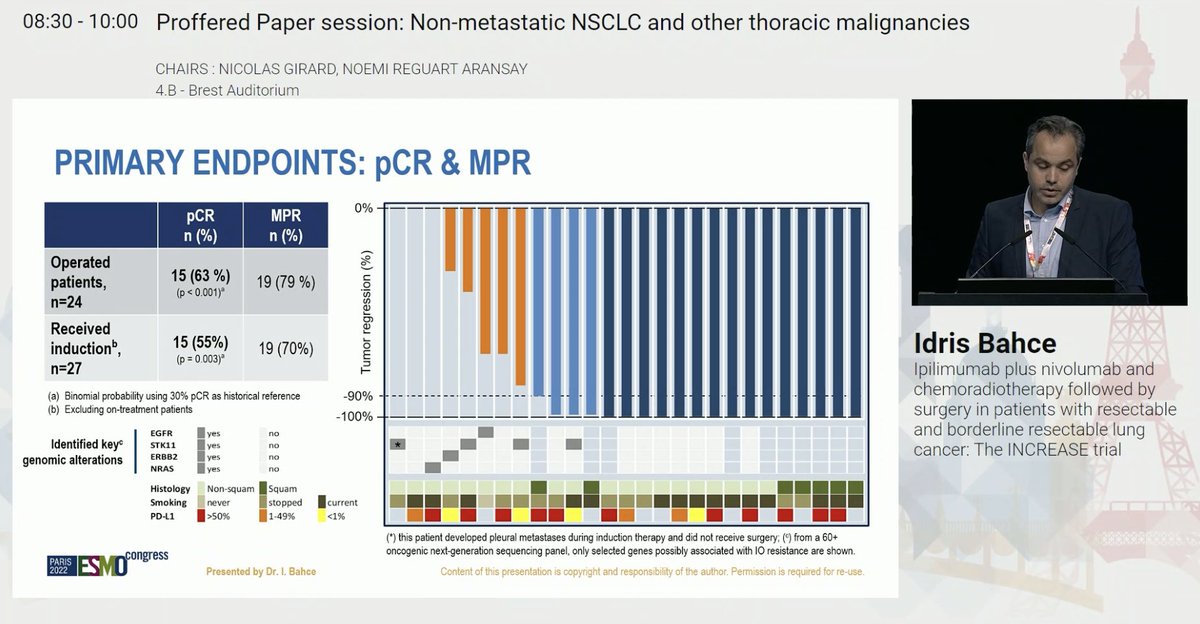
Wow. Of those who underwent surgery after neoadjuvant nivo + ipi + radiation, 63% (!) had pCR and 79% had MPR. #ESMO22 
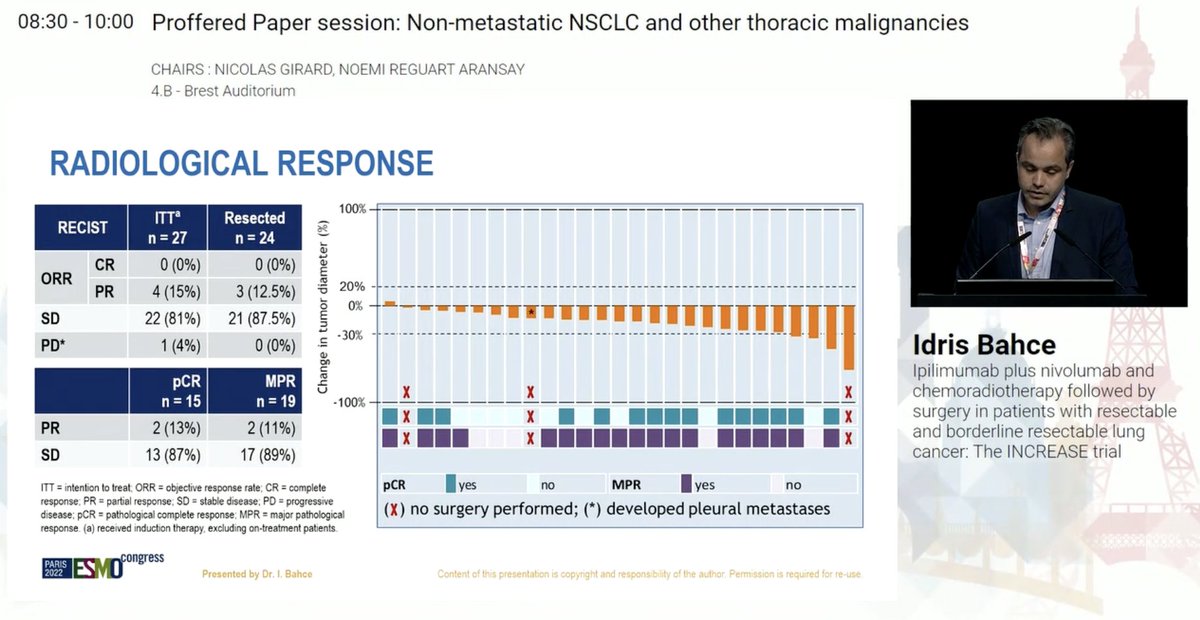
Radiographic response rate only 15% - reinforcing disconnect between RECIST and pathologic responses. Illustrative superior sulcus case. Some interesting changes in CD8+ subset of T cells especially in those who have a pCR #ESMO22 




Small study but impressive pCR rate here. Appealing for superior sulcus tumors, where chemoradiation is our standard, but perhaps we need to revisit the role of neoadjuvant radiation in resectable NSCLC in the perioperative immunotherapy era? #ESMO22 

• • •
Missing some Tweet in this thread? You can try to
force a refresh