@JohnKastelein John - Perhaps the only thing we'll agree on is that FH ppl have high LDL and increased CHD early in life (as Mundal et al showed). Where we disagree is why this occurs. As FH ppl have high LDL all their lives, why does CVD mortality decline over time? 

@JohnKastelein While the increased CVD mortality early in life is frightening, the magnitude of the mortality overall is small, and all-cause mortality, even early in life, is not statistically significant compared to the non-FH population. So a small % of the FH population dies from CVD. 

@JohnKastelein Let's address your comment from 2001 that environmental factors influence FH CHD and mortality. 

@JohnKastelein First, LDL-C as well as LDL-P are both composed of heterogeneous components, including sdLDL, which is increased with insulin resistant, and Lp(a), which is an indep CHD risk factor. Thus, high LDL-C or LDL-P, alone, does not address metabolic factors that affect sdLDL vs lbLDL. 

@JohnKastelein Indeed, if you look at the population level, high LDL-C is irrelevant when you take into account sdLDL vs lbLDL. The metabolic environment affects which will dominate to become pattern A (healthy) or pattern B (unhealthy) which is assoc with high TG/low HDL. 

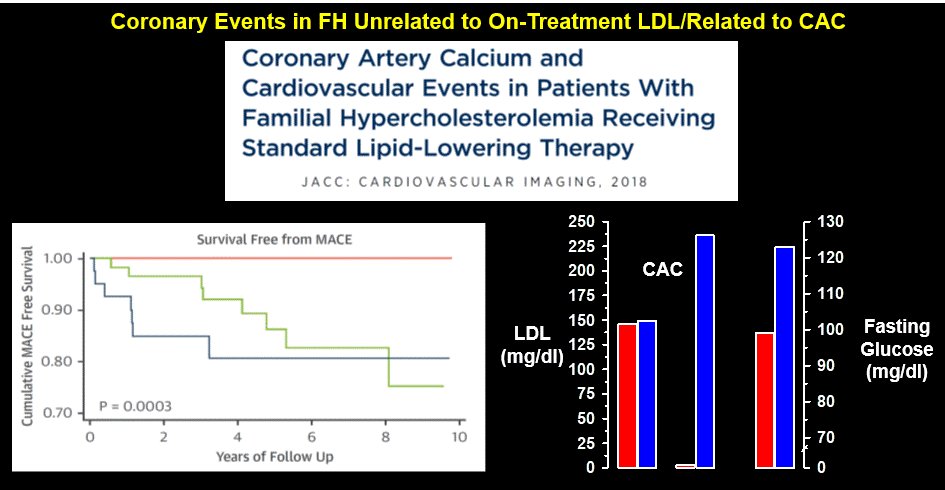
@JohnKastelein In FH, what is best indicator of CVD risk: coronary calcium (CAC), which is largely indep of LDL. In this study, LDL in statin-treated ppl was equivalent between high and 0 CAC. A major difference: High vs low fasting glucose (indep of LDL). 
@JohnKastelein The field has focused on high LDL in FH, but there is a secondary risk factor that is ignored: FH ppl tend to have elevated clotting factors. This is important because environmental/metabolic triggers will produce more CHD in FH by activating clotting factors more readily. 

@JohnKastelein What activates clotting factors? Smoking is a strong factor and FH may be more sensitive to the hypercoagulant effect of smoking than non-FH. Look at the vast difference in 25 year CVD free survival between FH smokers and non-smokers. 

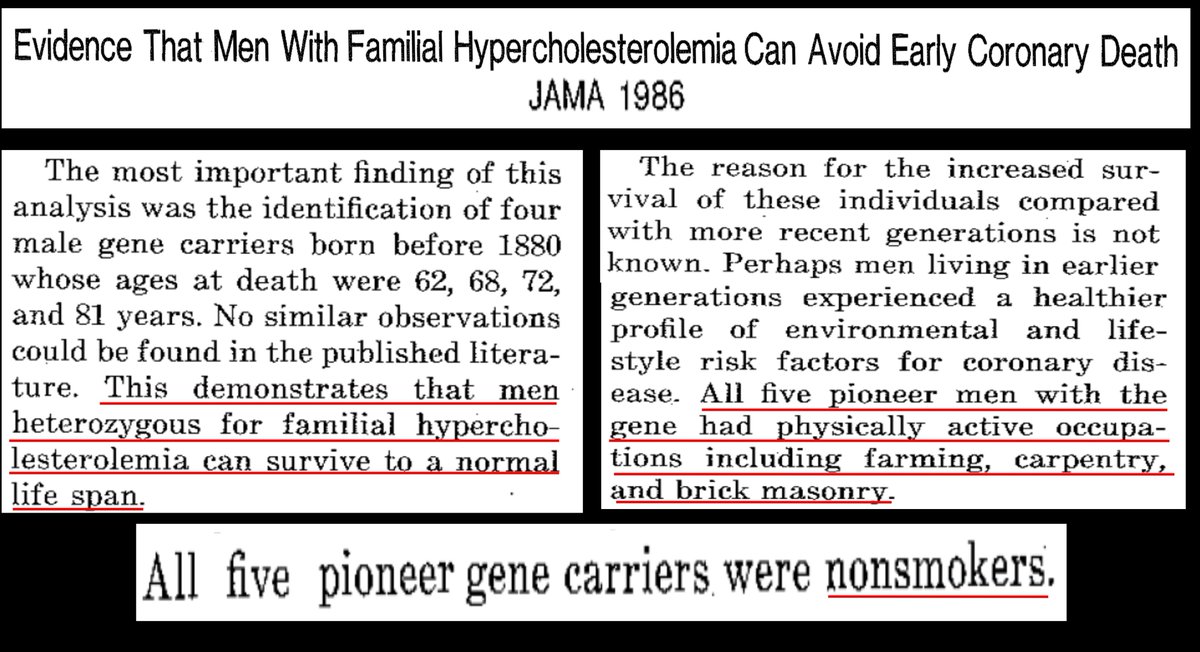
@JohnKastelein Indeed, smoking was noticed as a survival factor in FH people born in the 19th c and surviving to old age in the 20th 
@JohnKastelein In addition, FH ppl are very sensitive to hypertension, which can be ameliorated with #LCHF
Compared hypertensive with non-hypertensive FH 25 year CVD free survival over 25 years.
Compared hypertensive with non-hypertensive FH 25 year CVD free survival over 25 years.

@JohnKastelein Related to everything in this thread is insulin resistance (e.g., obesity, insulin). As we showed in our review, FH ppl who are not overweight with low insulin have CAD rates equivalent to non-FH taking LDL into account. Again, a risk factor that is ameliorated by #LCHF 

@JohnKastelein So, putting this all together, the mechanism common to multiple CVD risk factors, including the subset of FH that develop CVD: hypercoagulation and hypofibrinolysis (not LDL) 

@JohnKastelein We covered much this lit in our papers on enhanced coagulation in a subset of FH. This explains ⬆️ CVD, particularly early in life, when activation of clotting factors via metabolism/smoking, takes its toll. This is where survivor bias is specific to clotting, not LDL. 

@JohnKastelein As to the small absolute risk benefits of statins, the basis is their pleiotropic, e.g., antithrombotic, effects, which is why statins are more effective in unhealthy (smokers, diabetics) compared to healthy ppl. 

@JohnKastelein Finally, you view LDL as inherently atherogenic, I don't.
LDL-p is damaged by the metabolism (⬆️BP, glucose, etc). Native LDL (lbLDL) in a metabolically health person is an energy transport cluster which has been unjustly convicted of causing atherosclerosis.
@bschermd
LDL-p is damaged by the metabolism (⬆️BP, glucose, etc). Native LDL (lbLDL) in a metabolically health person is an energy transport cluster which has been unjustly convicted of causing atherosclerosis.
@bschermd
• • •
Missing some Tweet in this thread? You can try to
force a refresh









