🧵Complex #Hemodynamics in ESRD:
Middle age pt ➡️ 🏥 for syncope
HPI: Low BP during HD sessions. Does not achieve dry weight. Today she has had 6 episodes of syncope!
Last episode happened as she stood up from a chair
BP 88/62, HR 87 🧠 OK, CRT 2 sec
1/8
Middle age pt ➡️ 🏥 for syncope
HPI: Low BP during HD sessions. Does not achieve dry weight. Today she has had 6 episodes of syncope!
Last episode happened as she stood up from a chair
BP 88/62, HR 87 🧠 OK, CRT 2 sec
1/8
On #Echofist you notice this👇
During systole, flow from the LV towards the Aorta should all be blue in color! (Direction away from the probe)
This apparent change in direction (red sphere) is called Aliasing
Aliasing = Very high flow Velocity!
2/8
During systole, flow from the LV towards the Aorta should all be blue in color! (Direction away from the probe)
This apparent change in direction (red sphere) is called Aliasing
Aliasing = Very high flow Velocity!
2/8

Velocity can be quantified!
Use CW Doppler passing through the red sphere 👇
Velocity = 3.8 m/s 🚨🚨🚨 This is very fast!
Whenever you see a very fast flow, think of obstruction (similar to blocking a hose with your thumb👇)
What is causing the obstruction?
3/8

Use CW Doppler passing through the red sphere 👇
Velocity = 3.8 m/s 🚨🚨🚨 This is very fast!
Whenever you see a very fast flow, think of obstruction (similar to blocking a hose with your thumb👇)
What is causing the obstruction?
3/8


Obstruction is caused by severe LVH, this is not rare in ESRD with long term uncontrolled HTN.
Thick myocardial walls are causing mid ventricular obstruction during systole ➡️ some blood gets trapped at the apex ➡️ Lower CO
This worsens with exertion ➡️ syncope!
4/8
Thick myocardial walls are causing mid ventricular obstruction during systole ➡️ some blood gets trapped at the apex ➡️ Lower CO
This worsens with exertion ➡️ syncope!
4/8

How to treat?
We need to increase LV cavity volume to push the myocardial walls apart and relieve the obstruction!
This is usually achieved by some combination of:
🔷 Increase Preload
🔷 Increase Afterload
🔷 Decrease Contractility / HR
But this case had a twist!
5/8
We need to increase LV cavity volume to push the myocardial walls apart and relieve the obstruction!
This is usually achieved by some combination of:
🔷 Increase Preload
🔷 Increase Afterload
🔷 Decrease Contractility / HR
But this case had a twist!
5/8

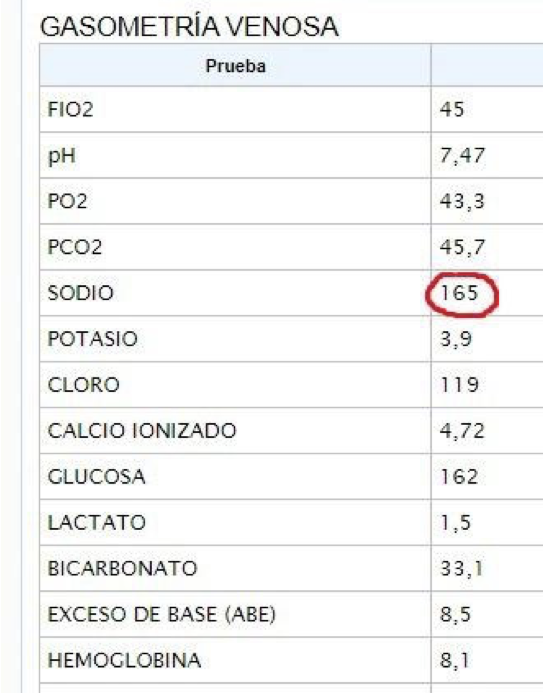
Look at parasternal long axis view! There is obvious RV dilation!
Remember the patient had not been able to achieve dry weight!
E/E' was 25! TRVMax 2.9
#VExUS Portal Vein Pulsatility Fraction > 100%
This patient has severe venous congestion!
6/8
Remember the patient had not been able to achieve dry weight!
E/E' was 25! TRVMax 2.9
#VExUS Portal Vein Pulsatility Fraction > 100%
This patient has severe venous congestion!
6/8
Dilated RV is compressing the LV!
This makes the LV cavity smaller and EXACERBATES Obstruction! 🤯
Treatment is decongestion!
Ultrafiltration ➡️ reduced RV Volume ➡️ reduced septal shift ➡️ less LV compression ➡️ less mid-ventricular obstruction!
7/8
This makes the LV cavity smaller and EXACERBATES Obstruction! 🤯
Treatment is decongestion!
Ultrafiltration ➡️ reduced RV Volume ➡️ reduced septal shift ➡️ less LV compression ➡️ less mid-ventricular obstruction!
7/8
We started vasopressin and removed fluid (used Portal Vein to monitor decongestion); Then added oral Beta-Blocker
Patient decongested nicely to a normal portal vein and obstruction improved significantly! (Velocity = 1.9 m/s)
Syncope is now completely gone!
#POCUSAlways
8/8

Patient decongested nicely to a normal portal vein and obstruction improved significantly! (Velocity = 1.9 m/s)
Syncope is now completely gone!
#POCUSAlways
8/8


• • •
Missing some Tweet in this thread? You can try to
force a refresh