My living 🧵 on the highlights from 'Causes of obesity: theories, conjectures and evidence.' #RScausesobesity
@royalsociety
Link: causes-obesity.royalsociety.org
@royalsociety
Link: causes-obesity.royalsociety.org
DAY 1 -- From genetics to nutrient-dependent conditioned eating, variable mitochondrial energy efficiency, neuroendocrine feedback systems, and nutrient-sensing food liking, obesity is very clearly more complicated than CICO. Energy balance is a constraint, that is all.
GENETIC SUBTYPING OBESITY by Dr. Loos
👉Genes contribute to genetic susceptibility, but it is hard to say how much.
👉Obesity subtyping will require more than genetic information. #RScausesobesity


👉Genes contribute to genetic susceptibility, but it is hard to say how much.
👉Obesity subtyping will require more than genetic information. #RScausesobesity



GENETICS OF OBESITY AND THINNESS by Dr. Farooqi
👉LoF and GoF variants in MC4R can predispose to weight gain or defend against weight gain, respectively
👉Leptin-melanocortin system mediates nutrient preference #RScausesobesity


👉LoF and GoF variants in MC4R can predispose to weight gain or defend against weight gain, respectively
👉Leptin-melanocortin system mediates nutrient preference #RScausesobesity



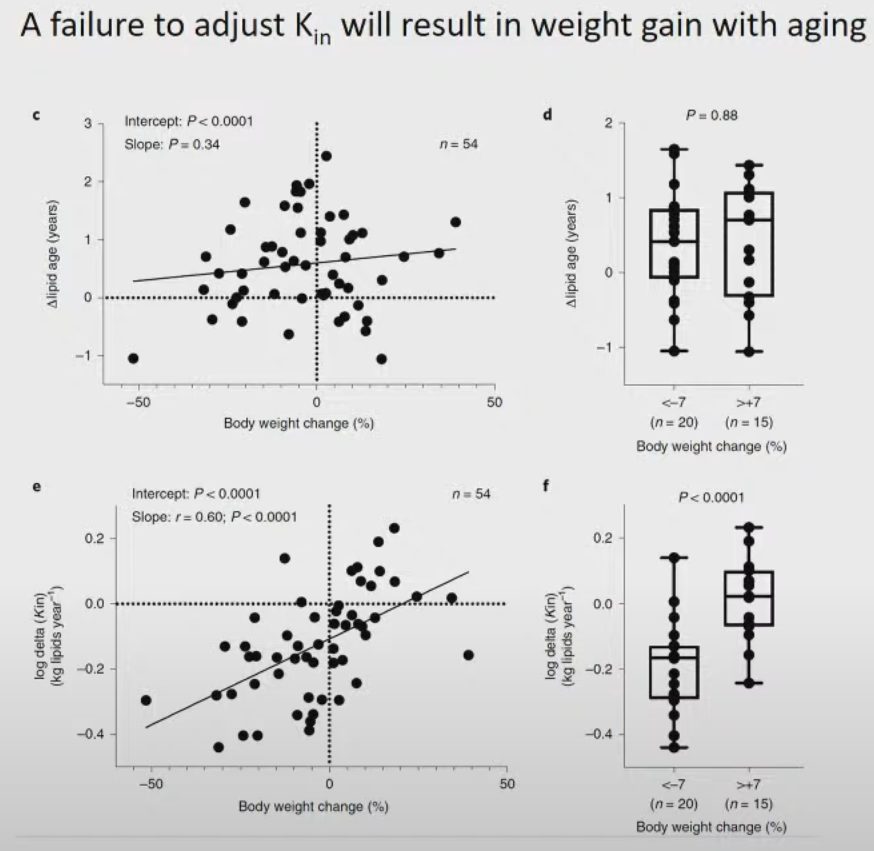
Adipocyte and lipid turnover in human adipose tissue by Dr. Spalding
Aging adipocytes are less flexible, reducing lipid turnover with age and ultimately predisposing to more wt gain over time. #RScausesobesity


Aging adipocytes are less flexible, reducing lipid turnover with age and ultimately predisposing to more wt gain over time. #RScausesobesity


A unifying pathway for obesity mediated by fructose metabolism by Dr. Johnson
--
Fructose can ⬇️ ATP levels inside cells ➡️metabolic inflexibility & wt gain. The degree of ATP depletion depends on the concentration of nutrients the liver sees & mitochondrial health.


--
Fructose can ⬇️ ATP levels inside cells ➡️metabolic inflexibility & wt gain. The degree of ATP depletion depends on the concentration of nutrients the liver sees & mitochondrial health.



As Dr. Johnson states: eat your whole fruits. Don't drink your fruits or fruit juice concentrates. They elicit very different biological responses.
Sex hormones impact ALL aspects of metabolism by Dr. Clegg #RScausesobesity
--
Estrogen influences adipocyte flexibility, likely related to estrogen's ability to increase the expression of ERalpha in adipocytes. Estrogen has so many effects on adipose tissue!!


--
Estrogen influences adipocyte flexibility, likely related to estrogen's ability to increase the expression of ERalpha in adipocytes. Estrogen has so many effects on adipose tissue!!



Is there a role for higher cognitive functions in the development of obesity? by Dr. Higgs
It's all hard to untangle due to flawed study designs and many confounders. #RScausesobesity

It's all hard to untangle due to flawed study designs and many confounders. #RScausesobesity


High-fat/high-sugar diets rewire dopamine circuits to impact behaviour before the onset of weight gain by Dr. Small
--
👉Energy-dense foods alter dopamine physiology which alters metabolism (in mice)
👉High energy-dense foods likely alter motivation and reward pathways in humans

--
👉Energy-dense foods alter dopamine physiology which alters metabolism (in mice)
👉High energy-dense foods likely alter motivation and reward pathways in humans


Obesity, mitochondrial energy efficiency and insulin secretion by. Dr. Corkey
Presents an interesting hypothesis whereby non-nutritive food agents could alter REDOX metabolism leading to mitochondrial dysfunction, insulin hypersecretion, and obesity. #RScausesobesity

Presents an interesting hypothesis whereby non-nutritive food agents could alter REDOX metabolism leading to mitochondrial dysfunction, insulin hypersecretion, and obesity. #RScausesobesity


Leptin and a simple circuit regulating feeding by. Dr. Friedman #RScausesobesity
--
--
https://twitter.com/MichaelAlbertMD/status/1582029631250903042?s=20&t=XQWga8AS8wTxE1G6N1fTzA
Day 2: Dr. Friedman provided my favorite lines of the day.
"Telling ppl to eat less & exercise more will not work. The question is, why does it not work? The available evidence is that there are biological factors that resist that conscious drive in most, not all ppl."
"Telling ppl to eat less & exercise more will not work. The question is, why does it not work? The available evidence is that there are biological factors that resist that conscious drive in most, not all ppl."
Paraphrasing another wonderful point: "the failure of eating less does not mean we disregard the consensus evidence around energy balance...doing this would be a strawman interpretation of the evidence." #RScausesobesity
Competing obesity paradigms: the energy balance vs. carbohydrate-insulin models by Dr. Ludwig.
Maybe the most provocative slide from the talk. How do we explain this phenomenon? Stable Ein with an almost linear rise in obesity prevalence. Food for thought. #RScausesobesity
Maybe the most provocative slide from the talk. How do we explain this phenomenon? Stable Ein with an almost linear rise in obesity prevalence. Food for thought. #RScausesobesity

Protein leverage and human obesity by Dr. Simpson
Does protein dilution explain the rise in Ein?
👉Provocative thought: reformulating UPFs to contain higher amounts of protein (less sugar and fat) may attenuate some harmful effects. #RScausesobesity

Does protein dilution explain the rise in Ein?
👉Provocative thought: reformulating UPFs to contain higher amounts of protein (less sugar and fat) may attenuate some harmful effects. #RScausesobesity


Dietary fat, energy density and energy intake by Dr. Stubbs
People tend to eat in proportion to the energy density of their diets (i.e., higher ED => more consumption).
👉Equating the ED of diets with different macros ablates the discrepancy in ad-lib eating.🤯 #RScausesobesity



People tend to eat in proportion to the energy density of their diets (i.e., higher ED => more consumption).
👉Equating the ED of diets with different macros ablates the discrepancy in ad-lib eating.🤯 #RScausesobesity




2/3rds of the foods you encounter daily fall into a higher energy density category!!! #RScausesobesity 

Do ultra-processed foods cause obesity? by Kevin Hall.
Food scientists are engineering new products to sell more food, and despite the massive increase in food production, nearly 2/3rd of Calories turned into food waste.
Food scientists are engineering new products to sell more food, and despite the massive increase in food production, nearly 2/3rd of Calories turned into food waste.

FFM and RMR are strong determinants of energy intake: integration into a theory of appetite by Dr. Blundell
"Appetite is the property of the whole system."
👉FFM, not fat mass, is related to Ein (i.e., FFM is providing tonic feedback).
#RScausesobesity



"Appetite is the property of the whole system."
👉FFM, not fat mass, is related to Ein (i.e., FFM is providing tonic feedback).
#RScausesobesity




Does eating less or exercising more to reduce energy availability produce distinct physiological responses? by Professor Halsey
Many microsystems within the body may adapt to changing energy & BM, that collectively, provide the measured adaptive response. 🤔 #RScausesobesity
Many microsystems within the body may adapt to changing energy & BM, that collectively, provide the measured adaptive response. 🤔 #RScausesobesity

Paleolithic perspectives on human diet and cardiometabolic health by Dr. Pontzer
Primitive humans ate a diverse diet that would change due to seasonality and what was available.
Significant difference: modern humans make energy-dense foods easier to acquire.
#RScausesobesity



Primitive humans ate a diverse diet that would change due to seasonality and what was available.
Significant difference: modern humans make energy-dense foods easier to acquire.
#RScausesobesity




Riveting follow-up: the Hadza don't mix foods together at one meal. Could the diversity of foods introduced in a given meal predispose to overeating? Does this explain how 'sensory-specific satiety' contributes to appetite regulation?
The "Gravitostat" by Dr. Jansson
Proposal for 'sensor-independent mechanism' whereby increasing Ein in relation to BW when working against gravity.
Proposal for 'sensor-independent mechanism' whereby increasing Ein in relation to BW when working against gravity.

Questioning the foundations of the gut microbiota and obesity by @MatthewJDalby
Takeaway: the causal role of gut microbiota in obesity remains unproven.


Takeaway: the causal role of gut microbiota in obesity remains unproven.



Big congrats to Matthew! This incredible investigation has only reinforced my skepticism on microbiome claims, particularly concerning bodyweight regulation. 👏👏👏
• • •
Missing some Tweet in this thread? You can try to
force a refresh