
Co-Founder, Chief Medical Officer @accomplishhlth | Physician dedicated to reimagining obesity and sleep care in the US
How to get URL link on X (Twitter) App


 1⃣ Insurance navigation
1⃣ Insurance navigation


 2/ If you're familiar with semaglutide, you may know it is FDA-approved for treating obesity and chronic weight management under the brand name "WE-GOVY."
2/ If you're familiar with semaglutide, you may know it is FDA-approved for treating obesity and chronic weight management under the brand name "WE-GOVY." 

 link.springer.com/article/10.100…
link.springer.com/article/10.100…

 Bariatric surgery is exceedingly effective for people with obesity and NASH.
Bariatric surgery is exceedingly effective for people with obesity and NASH. 









 Weight Loss Goal? Not a number but a health improvement. With modern treatments, I would argue we should aim for 10% TBWL. #YWM2022Virtual
Weight Loss Goal? Not a number but a health improvement. With modern treatments, I would argue we should aim for 10% TBWL. #YWM2022Virtual 



 2/ First off, all study participants "received open-label once-weekly subcutaneous semaglutide, 0.25 mg, increased every 4 weeks to the maintenance dose of 2.4 mg once weekly by week 16, and continued to week 20."
2/ First off, all study participants "received open-label once-weekly subcutaneous semaglutide, 0.25 mg, increased every 4 weeks to the maintenance dose of 2.4 mg once weekly by week 16, and continued to week 20."

https://twitter.com/TheMooreLab/status/15054197275936890902/ Do Diets Matter? Yes and No. They matter because you have to eat, and you want to do so in a way that promotes health. But, are they reliable txs for obesity? No. Meta-analysis of long-term RCTs (avg wt loss 0-4 kg). Most intensive diet interventions result in 3-5% wt loss.


 2/ Intervention: Intensive Behavioral Therapy + Low Calorie Diet +/- SEMA 2.4 mg #OW2021
2/ Intervention: Intensive Behavioral Therapy + Low Calorie Diet +/- SEMA 2.4 mg #OW2021 
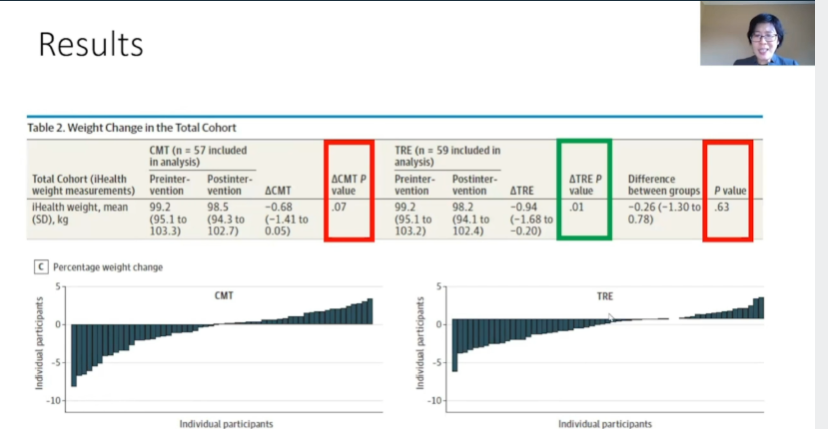
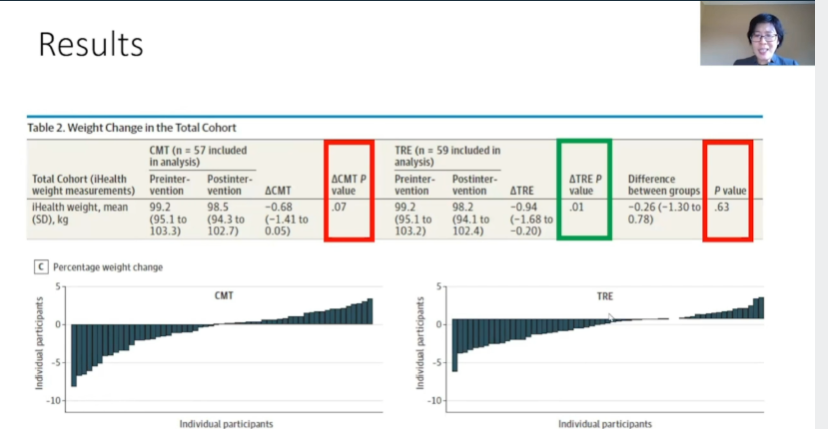
 2/ Eating in the AM is possibly more satiating. #OW2021
2/ Eating in the AM is possibly more satiating. #OW2021 

 Point #2: An active, involuntary physiological system determines body fatness at any one time. #OW2021
Point #2: An active, involuntary physiological system determines body fatness at any one time. #OW2021 


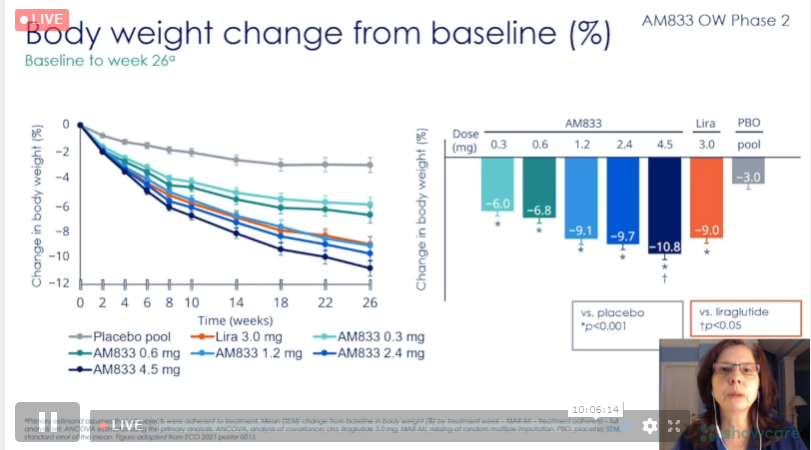
 2/ Tirzepatide; hard to imagine a future without tirzepatide (as long as safety & tolerability remain) for the treatment of metabolic dz when >10% wt loss and -2.5% A1c are avg results. Also, >50% of participants achieved normoglycemia with most doses‼️
2/ Tirzepatide; hard to imagine a future without tirzepatide (as long as safety & tolerability remain) for the treatment of metabolic dz when >10% wt loss and -2.5% A1c are avg results. Also, >50% of participants achieved normoglycemia with most doses‼️


