A proud day at #TraumaCare22 where the ‘Ten Second Triage’ tool has been officially launched
Recommended as first line triage tool for all incidents
/1
Recommended as first line triage tool for all incidents
/1
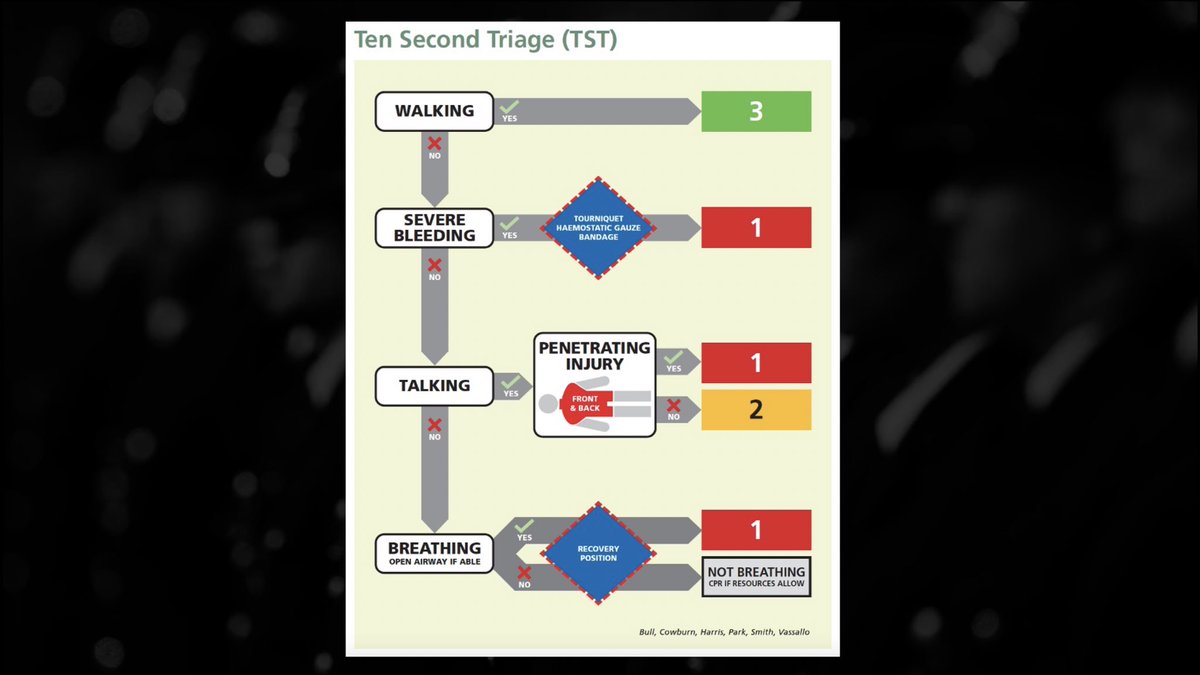
TST is designed as a pan-emergency service early scene triage tool, actively confronting the challenges experienced by tools that have come before it (none of which were good enough)
Signed off for:
Amb & Military
Recommended for:
Police & Fire
(sign off likely imminent)
/2
Signed off for:
Amb & Military
Recommended for:
Police & Fire
(sign off likely imminent)
/2
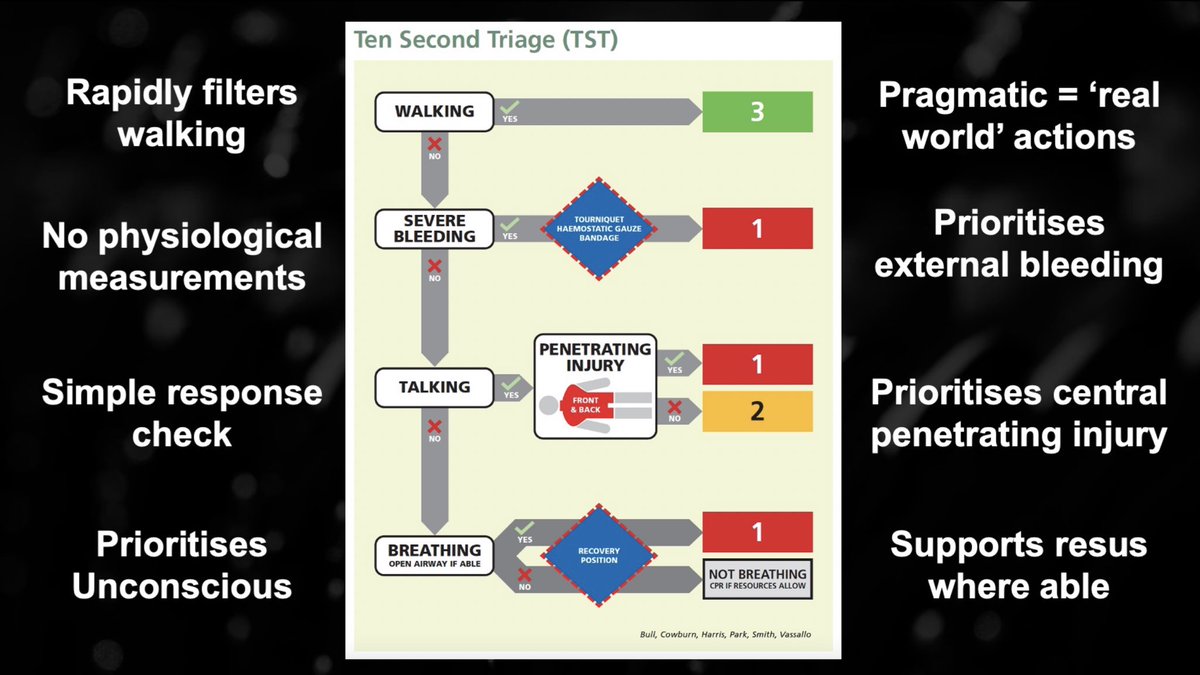
TST rapidly filters walking patients
Especially relevant for initial responding police officers who are likely to control ‘walkers’ robustly
Training will include a caveat for those who are walking with critical injury - you there, sit down
/3
Especially relevant for initial responding police officers who are likely to control ‘walkers’ robustly
Training will include a caveat for those who are walking with critical injury - you there, sit down
/3
It does not rely on physiological measurements:
We know that such measurements are irrelevant in the emerging phase of an incident
Theory ≠ Real World
Try finding any alive casualty with a pulse below 100 or even 120 immediately post explosion or during a marauding attack
/4
We know that such measurements are irrelevant in the emerging phase of an incident
Theory ≠ Real World
Try finding any alive casualty with a pulse below 100 or even 120 immediately post explosion or during a marauding attack
/4
Try reliably finding a pulse if you are an incredibly stressed police officer, firefighter or paramedic in ballistic/CBRN PPE
Try finding a first responder who legitimately & accurately quantifies resp rate in the immediate assessment of GSW victim
Me = Lots, some or none
/5
Try finding a first responder who legitimately & accurately quantifies resp rate in the immediate assessment of GSW victim
Me = Lots, some or none
/5
TST utilises a nuanced response check
Talking is proxy for adequate cerebral perfusion. In the world of AVPU it may feel non clinical but is useful across the spectrum of responders and is sensitive for critical injury
‘Talking’ also P1 safeguards children too young to talk
/6
Talking is proxy for adequate cerebral perfusion. In the world of AVPU it may feel non clinical but is useful across the spectrum of responders and is sensitive for critical injury
‘Talking’ also P1 safeguards children too young to talk
/6

It prioritises unconscious casualties and encourages immediate essential airway management.
TST is not prescriptive and is adaptable, allowing for local interpretation of ‘airway management’ for those who may carry additional airway adjuncts
/7
TST is not prescriptive and is adaptable, allowing for local interpretation of ‘airway management’ for those who may carry additional airway adjuncts
/7

TST is designed to be pragmatic and is reflective of the gold standard, real world actions of any police officer or ambulance responder to the victim of a stabbing or gunshot
/8
/8

I want a police officer to prioritise the victim who is on the floor
I want them to aggressively arrest external haemorrhage
I want them to assess a responsive casualty for central injury in order to report accurately, enabling appropriate enhanced care support
/9
I want them to aggressively arrest external haemorrhage
I want them to assess a responsive casualty for central injury in order to report accurately, enabling appropriate enhanced care support
/9
I want a police officer to prioritise the victim who is on the floor
I want them to aggressively arrest external haemorrhage
I want them to recognise reduced levels of consciousness and intervene with airway management or resuscitation as required
/10
I want them to aggressively arrest external haemorrhage
I want them to recognise reduced levels of consciousness and intervene with airway management or resuscitation as required
/10
I use police officers in this example because if I’m bleeding to death, I don’t care who applies my tourniquet or packs my junctional injury
I also don’t care what brand of tourniquet or type of dressing
The measure of success is effective haemorrhage control
/11
I also don’t care what brand of tourniquet or type of dressing
The measure of success is effective haemorrhage control
/11

This is what we want our initial responders to do for single patients… and under pressure it is what they’ll do for multiple
TST is a structure that can be overlaid on ‘real world’ high threat care and provide triage categories in order to aid what happens next
/12
TST is a structure that can be overlaid on ‘real world’ high threat care and provide triage categories in order to aid what happens next
/12

TST is pragmatically based on real world actions rather than suggesting staff should measure physiology, actioning a complicated, unwieldy and rarely practiced system
On a bad day, we know people will revert to what they know (and what they know is right!)
/13
On a bad day, we know people will revert to what they know (and what they know is right!)
/13
TST prioritises central penetrating injury
Neck, Chest, Back, Axilla, Abdomen, Groin, Buttocks
This is a new consideration
This is the injury pattern I lose sleep over as it’s the one we know we cannot effectively manage out of hospital
/15
Neck, Chest, Back, Axilla, Abdomen, Groin, Buttocks
This is a new consideration
This is the injury pattern I lose sleep over as it’s the one we know we cannot effectively manage out of hospital
/15

If I’m bleeding to death from a non compressible injury I now do care about what uniform you are wearing!
The inclusion of ‘P1 - Central Injury’ is huge, it builds in a bias to action for these patients. The same group we aim for ‘minimum on-scene times’ for every other day
/16
The inclusion of ‘P1 - Central Injury’ is huge, it builds in a bias to action for these patients. The same group we aim for ‘minimum on-scene times’ for every other day
/16

TST allows for all responders to identify those not breathing, using an objective assessment of respiratory effort through an open airway
The following actions are scenario dependent
‘Dead’ is not the simple decision as perhaps we’ve trained it, almost enforcing futility
/17
The following actions are scenario dependent
‘Dead’ is not the simple decision as perhaps we’ve trained it, almost enforcing futility
/17

The tactical scenario can change
The resourcing scenario can change
Traumatic Cardiac Arrest is not always futile
Impact Brain Apnoea should not be fatal
Resuscitation should occur where possible
Decisions regarding ‘death’ should be handled with appropriate gravity
/18
The resourcing scenario can change
Traumatic Cardiac Arrest is not always futile
Impact Brain Apnoea should not be fatal
Resuscitation should occur where possible
Decisions regarding ‘death’ should be handled with appropriate gravity
/18
TST is an important cog in the mass casualty response machine
Policing has been historically focussed on threat confrontation
Healthcare has been historically delayed by threat mitigation
TST allows for concurrent, collaborative clinical activity
/19
Policing has been historically focussed on threat confrontation
Healthcare has been historically delayed by threat mitigation
TST allows for concurrent, collaborative clinical activity
/19

TST allows any activity before formal healthcare to be truly meaningful
Priorities should always include enabling access, but there will be scenarios when this is impossible
TST provides structure for policing to start a casualty management plan compatible with formal NHS
/20
Priorities should always include enabling access, but there will be scenarios when this is impossible
TST provides structure for policing to start a casualty management plan compatible with formal NHS
/20
It prevents duplication of effort and allows healthcare resources to hit the ground running instead of starting from scratch, triaging patients that have been with the police for x amount of time already
What an opportunity for marginal gains!
/20.5
What an opportunity for marginal gains!
/20.5
Casualty flow, or more importantly the lack thereof, has been a challenge in practically every mass casualty incident
Providing police officers a structure that can enable flow in scenarios where healthcare cannot access a scene is crucial
/21
Providing police officers a structure that can enable flow in scenarios where healthcare cannot access a scene is crucial
/21

The Ten Second Triage sieve looks to address many of the challenges presented by high threat mass casualty management
It’s pragmatic
It’s faster
It’s effective in the hands of police officers, ambulance staff and FRS
It’s sensitive where other systems have failed
/23
It’s pragmatic
It’s faster
It’s effective in the hands of police officers, ambulance staff and FRS
It’s sensitive where other systems have failed
/23

I’ve been very lucky to have been a part of the development of this tool, from initial concept, evolution through to final testing
Rolling out in Spring 23
Huge thanks and kudos to @ClairePark01, @NARU_org and @NHSEngland and all others involved
Rolling out in Spring 23
Huge thanks and kudos to @ClairePark01, @NARU_org and @NHSEngland and all others involved
What started as a local idea for the streets of London gained traction far beyond what I thought possible
@ClairePark01 has led and driven the piece phenomenally
The team @NARU_org & @NHSEngland Phil Cowburn, Jamie Vassallo, Jason Smith and Dave Bull have given it wings
@ClairePark01 has led and driven the piece phenomenally
The team @NARU_org & @NHSEngland Phil Cowburn, Jamie Vassallo, Jason Smith and Dave Bull have given it wings
What started off as a scribble in a notebook in wintery wales a number of years ago has been developed by the team into something that I believe is capable of improving outcomes in mass cas incidents
Hearing Phil & Claire announce it in its current guise is a career highlight!
Hearing Phil & Claire announce it in its current guise is a career highlight!
The enormity of the challenge to bring us to this point; the amalgamation of multiple other streams of work, including some alternative models across the country can’t be overlooked
I humbly applaud all of those involved who have made it happen
/end
I humbly applaud all of those involved who have made it happen
/end
• • •
Missing some Tweet in this thread? You can try to
force a refresh








