Dr Anna Nunokawa presents case of Amniotic Fluid Embolism (#AFE) at @DalAnesthesia grand rounds #OBAnes
(get her on #Medtwitter @garrettsbarry @axe1314 @Ropivacaine @jon_bailey_anes @AnaSjaus @bmacaulay2000 @Dolores_McKeen?)
(get her on #Medtwitter @garrettsbarry @axe1314 @Ropivacaine @jon_bailey_anes @AnaSjaus @bmacaulay2000 @Dolores_McKeen?)

The case: #AFE #OBAnes
Any questions at this point?
(Written consent for case presentation from patient)



Any questions at this point?
(Written consent for case presentation from patient)




A brief discussion of epidemiology and pathophysiology. #AFE is rare, but some retrospective literature suggests up to 45% mortality even in developed world - much higher in developing world #OBAnes 





Considerations for diagnosis of #AFE: up to 25% will be atypical (not meeting all 4 Clark’s Criteria). A quick refresher on diagnosis of DIC. Other signs include aura in awake patients and seizures/stroke
#OBAnes


#OBAnes



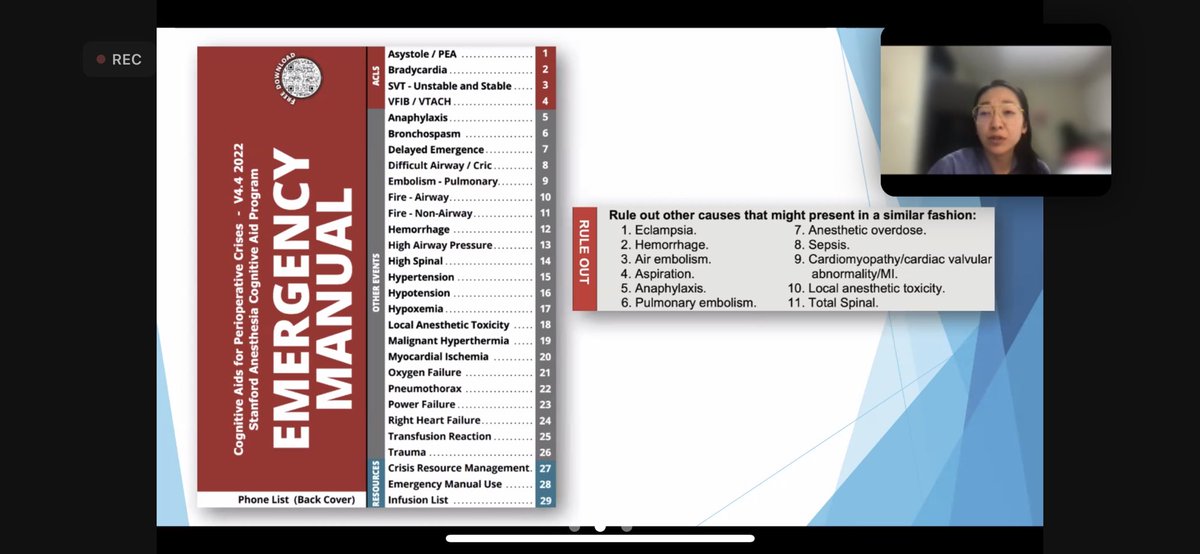
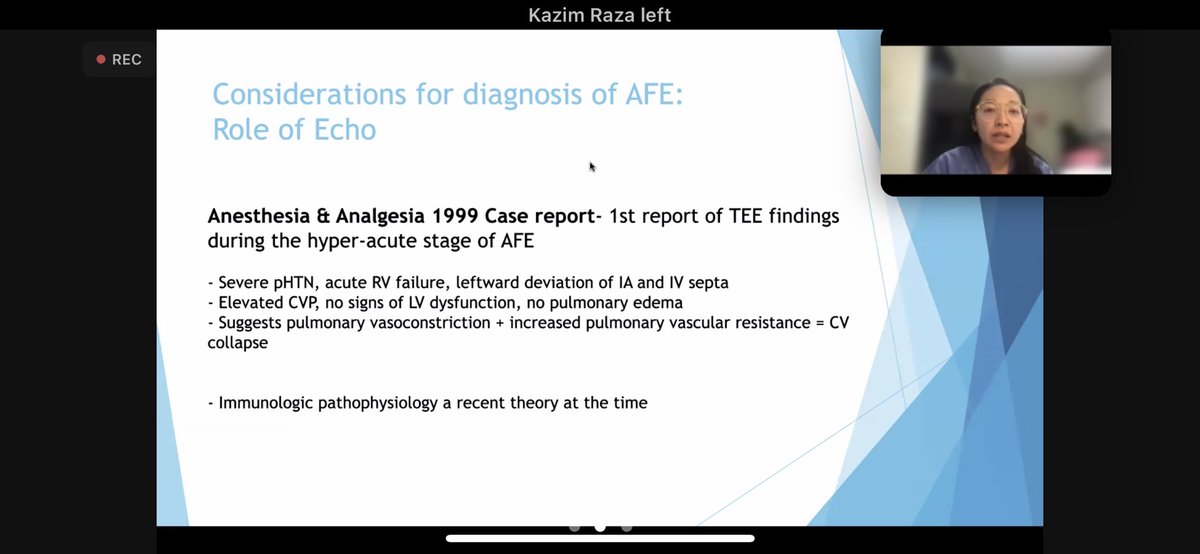
The differential diagnosis of #AFE is necessarily broad. @stanfordanes emergency manual has a list to rule out, although latest version puts AFE under embolism, losing the specific section. Investigations help - including echo
#OBAnes


#OBAnes


On echo in #AFE - what was found in the case (less movement of RV wall, TR, elevated RVSP - all resolved postoperatively
#OBAnes



#OBAnes




What does literature say about echo in #AFE? @CJA_Journal case series and review in 2021 - will add reference. LV failure in Acute phase suggests an alternative diagnosis.
#OBAnes


#OBAnes


Our outcome was great for this #AFE, able to mobilize a great team (@Dolores_McKeen @OBsleepmerchant @AnaSjaus), but recognize limitations of no POC ABG (@IWKHealth lab against POC), no ROTEM, pumps not set for significant resus. #OBAnes 

Some discussion points:
* reluctance to use cell salvage in setting of #AFE despite major transfusion (UK/IE/EU experience?) @noolslucas
* REBOA is becoming more useful in #OBAnes setting - definitely consider if surgeons applying aortic compression buys time to stabilize
* reluctance to use cell salvage in setting of #AFE despite major transfusion (UK/IE/EU experience?) @noolslucas
* REBOA is becoming more useful in #OBAnes setting - definitely consider if surgeons applying aortic compression buys time to stabilize

MOST important take home point: we were able to mobilize a team of 3 #OBAnes fellowship trained specialists, and despite a few POC limitations had capacity to access vascular surgery and interventional radiology during the case.
This is NOT the norm in the community hospital.
This is NOT the norm in the community hospital.
How do we improve outcomes in #AFE more widely?
@SOAPHQ @ruthi_landau @Ron_George @emilysharpe @OAAinfo @noolslucas @Eltonchris @girardDev @DrNickB_ObAnaes @LoughreyJPR @MarcVandeVelde6 @runa123 @yusuke_mazda
#OBAnes
@SOAPHQ @ruthi_landau @Ron_George @emilysharpe @OAAinfo @noolslucas @Eltonchris @girardDev @DrNickB_ObAnaes @LoughreyJPR @MarcVandeVelde6 @runa123 @yusuke_mazda
#OBAnes
@threadreaderapp unroll please
• • •
Missing some Tweet in this thread? You can try to
force a refresh