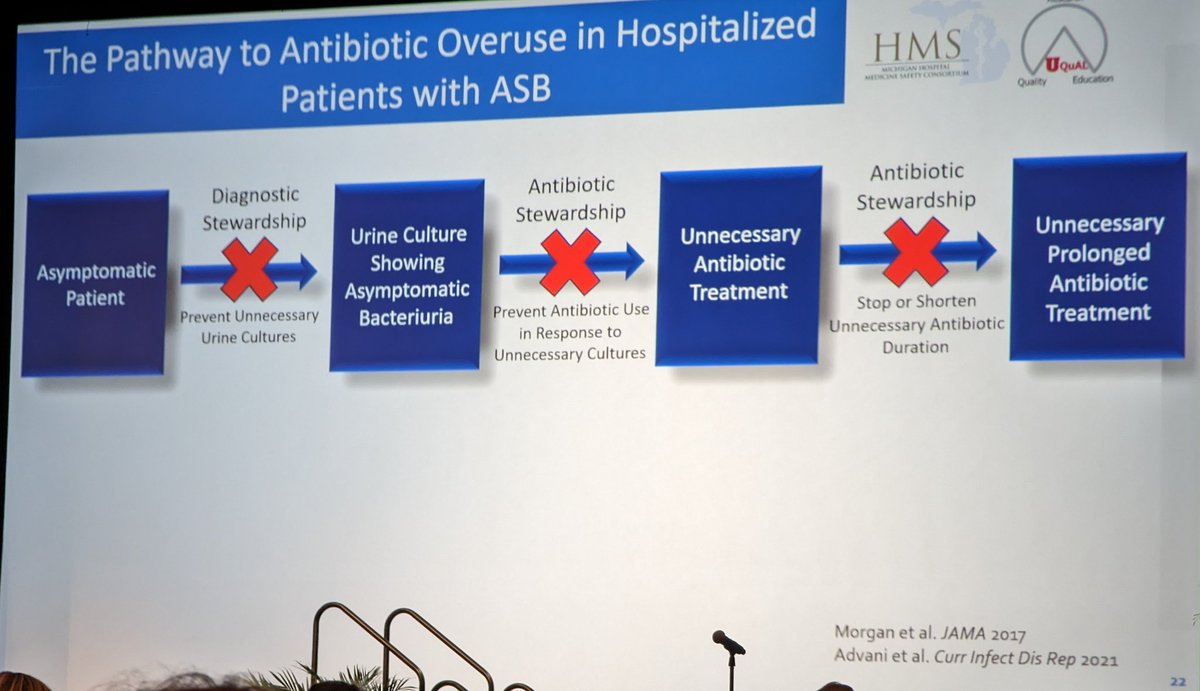
What's better for reducing unnecessary treatment of asymptomatic bacteriuria? Diagnostic stewardship or antibiotic stewardship?
@ValerieVaughnMD presenting the @SHEA_Epi featured oral abstract.
#IDWeek2022

@ValerieVaughnMD presenting the @SHEA_Epi featured oral abstract.
#IDWeek2022


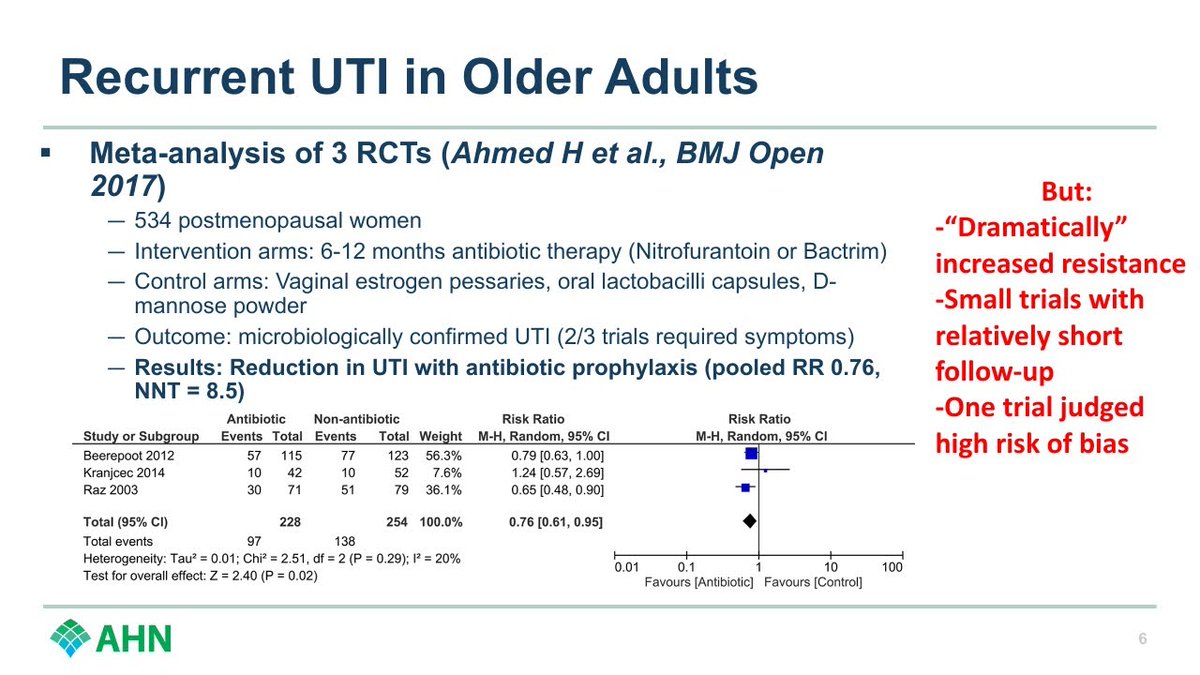
Antibiotic stewardship metric was ASB treated with abx / ASB and ASB treatment duration.
#IDWeek2022


#IDWeek2022



Antibiotic stewardship metric did not for the collective of hospitals, but did for some hospitals.
I'd be curious about how stewardship programs at these hospitals differed and whether that may have had a role.
#IDWeek2022
I'd be curious about how stewardship programs at these hospitals differed and whether that may have had a role.
#IDWeek2022

Conclusion
Diagnostic stewardship > antibiotic stewardship for ASB.
There's likely value in work at any stage along the pathway above, but appears preventing the UCx from happening in the first place is the best bang for your buck.
Great work, @ValerieVaughnMD!
#IDWeek2022


Diagnostic stewardship > antibiotic stewardship for ASB.
There's likely value in work at any stage along the pathway above, but appears preventing the UCx from happening in the first place is the best bang for your buck.
Great work, @ValerieVaughnMD!
#IDWeek2022



• • •
Missing some Tweet in this thread? You can try to
force a refresh