GP is changing because the needs of community care have changed over the past 30 years
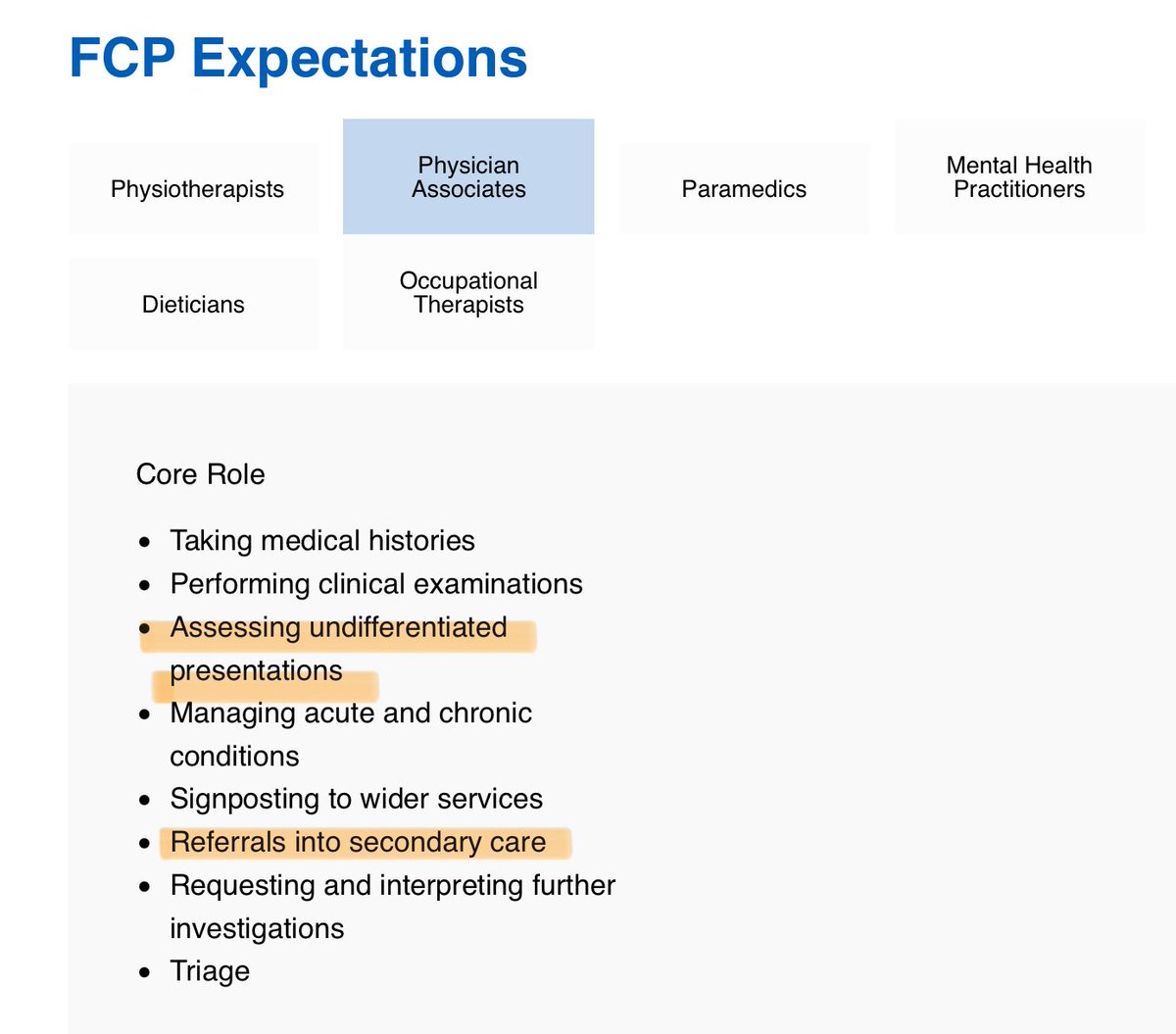
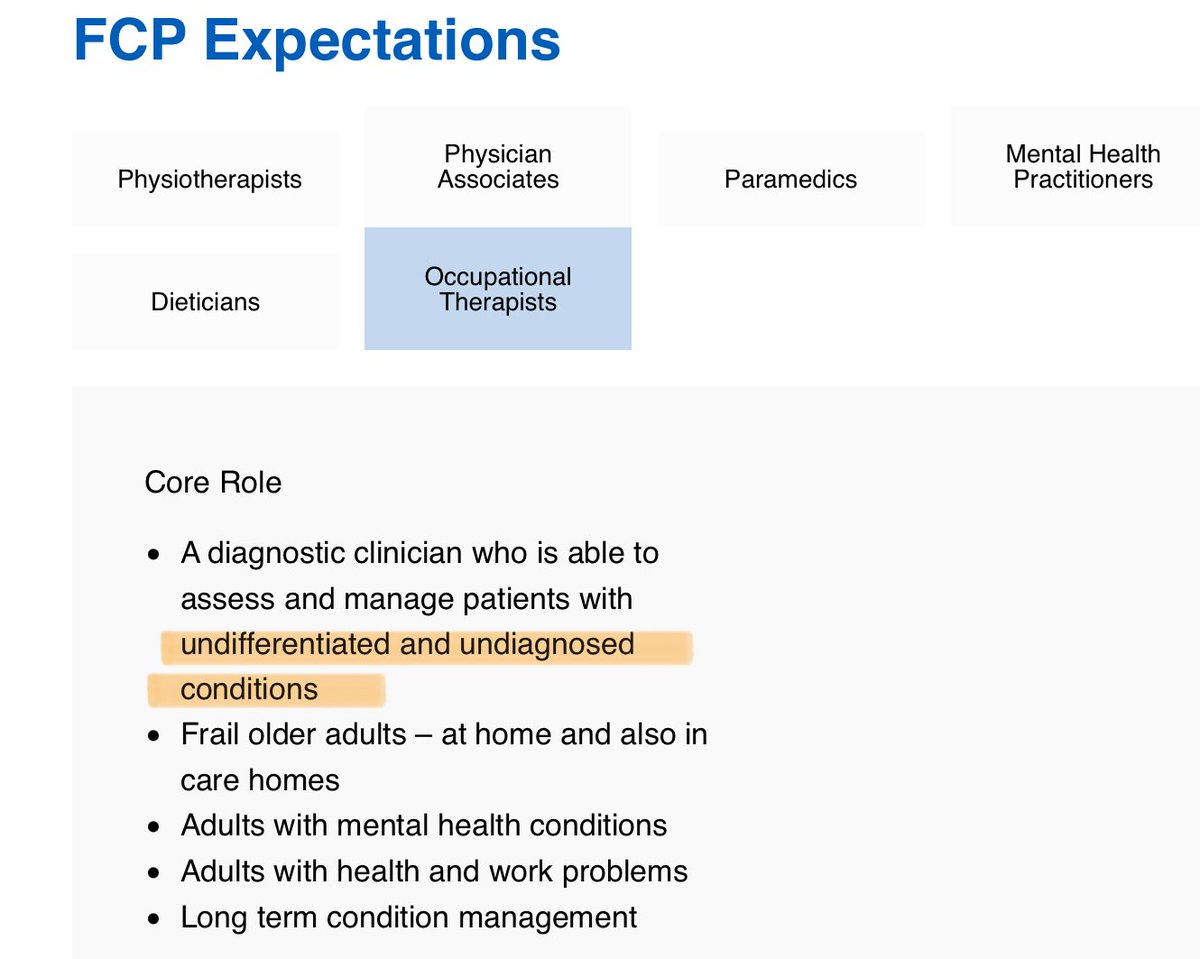
So in addition to Practice Nurses & GPs there are many other clinicians in the team
Thread 🧵👇🏻
So in addition to Practice Nurses & GPs there are many other clinicians in the team
Thread 🧵👇🏻

1.4million people a day consult a GP practice
Demand has increased (120% compared with 2019) but GP numbers have fallen (1800 fewer since 2015)
In order to manage demand additional systems have been needed as well as using different methods to consult, & additional clinicians 2/
Demand has increased (120% compared with 2019) but GP numbers have fallen (1800 fewer since 2015)
In order to manage demand additional systems have been needed as well as using different methods to consult, & additional clinicians 2/

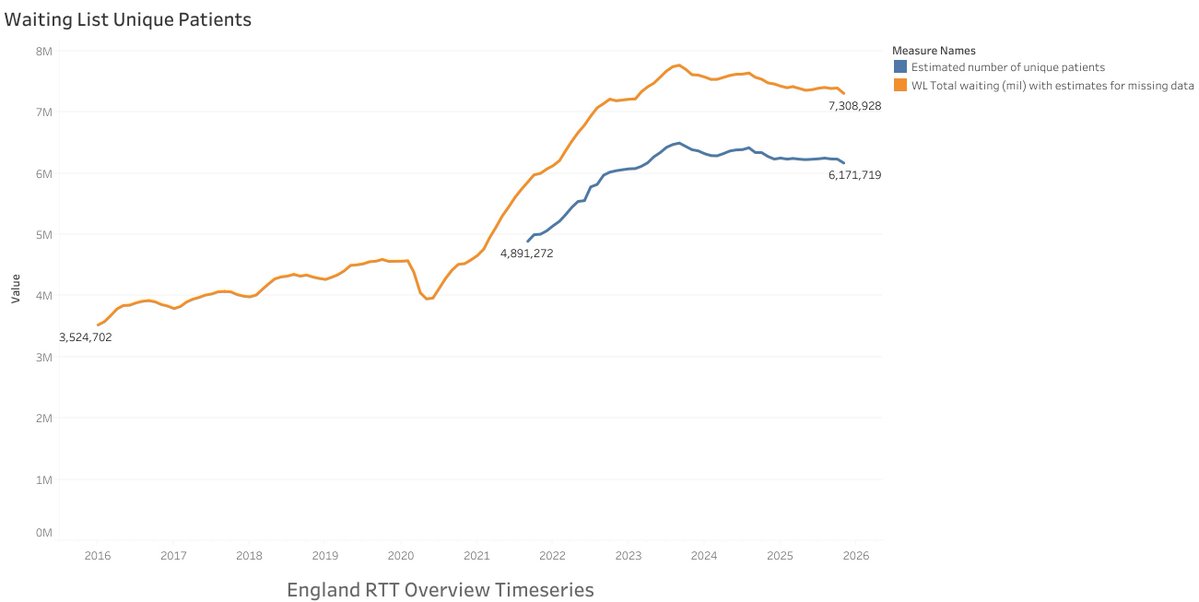
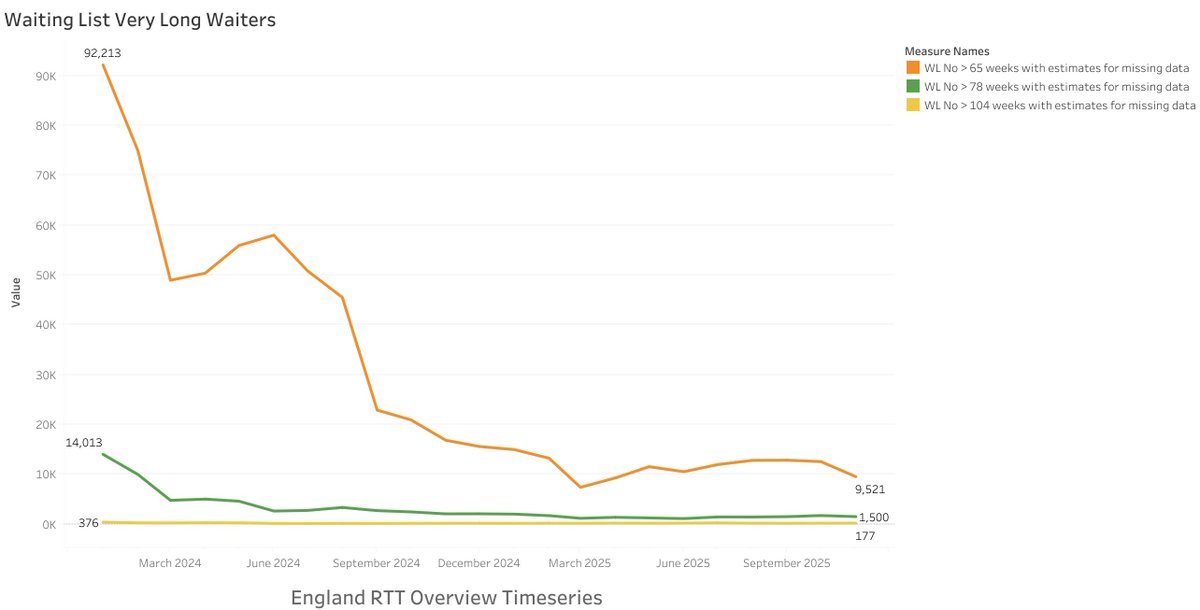
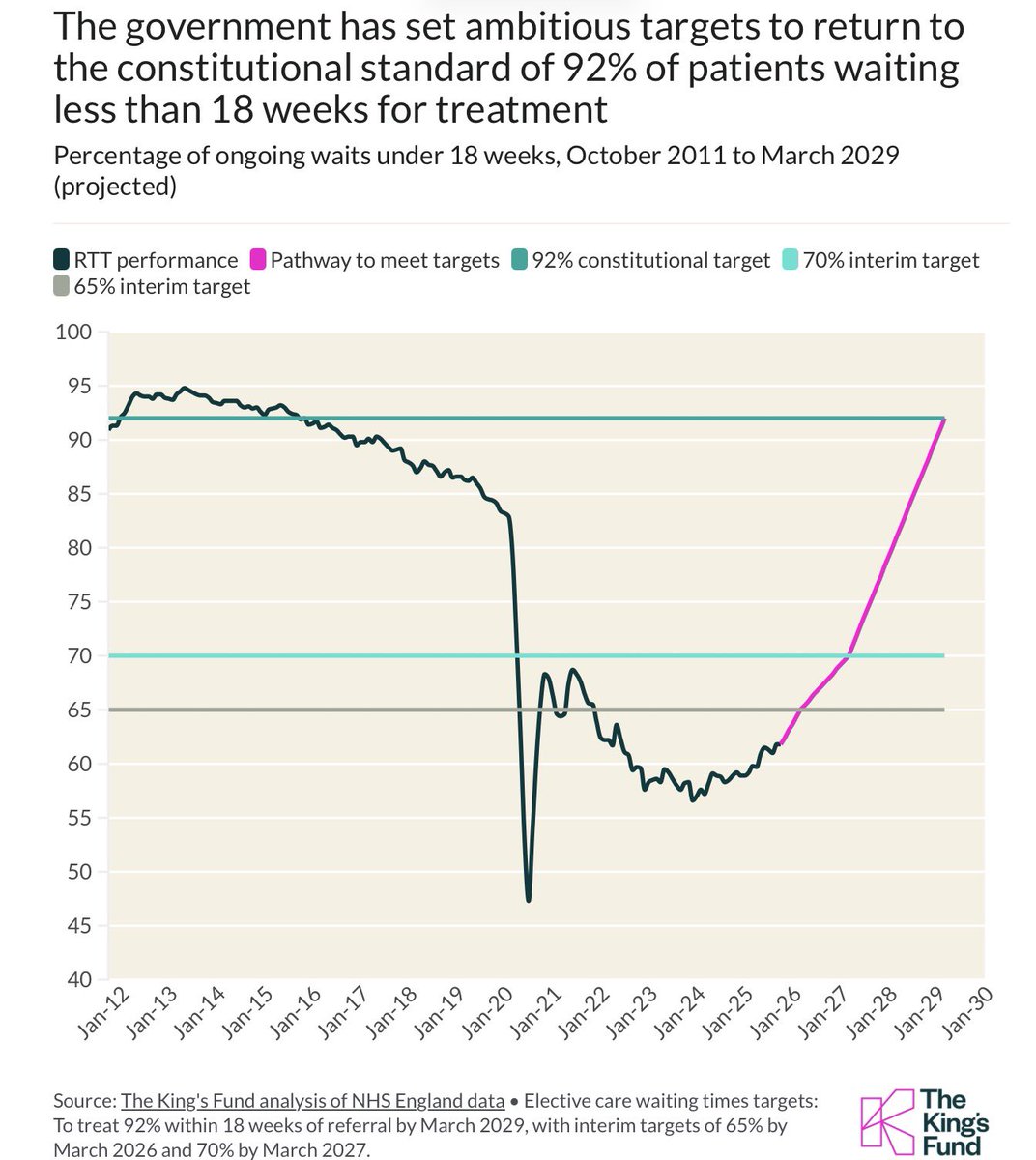
With 7m awaiting hospital treatment, 10m awaiting follow-up appts, an additional 500k are on long term sick leave since 2019
In addition advances in medical care mean many more are on medications, & have regular reviews of care
People live longer, population has increased
3/
In addition advances in medical care mean many more are on medications, & have regular reviews of care
People live longer, population has increased
3/

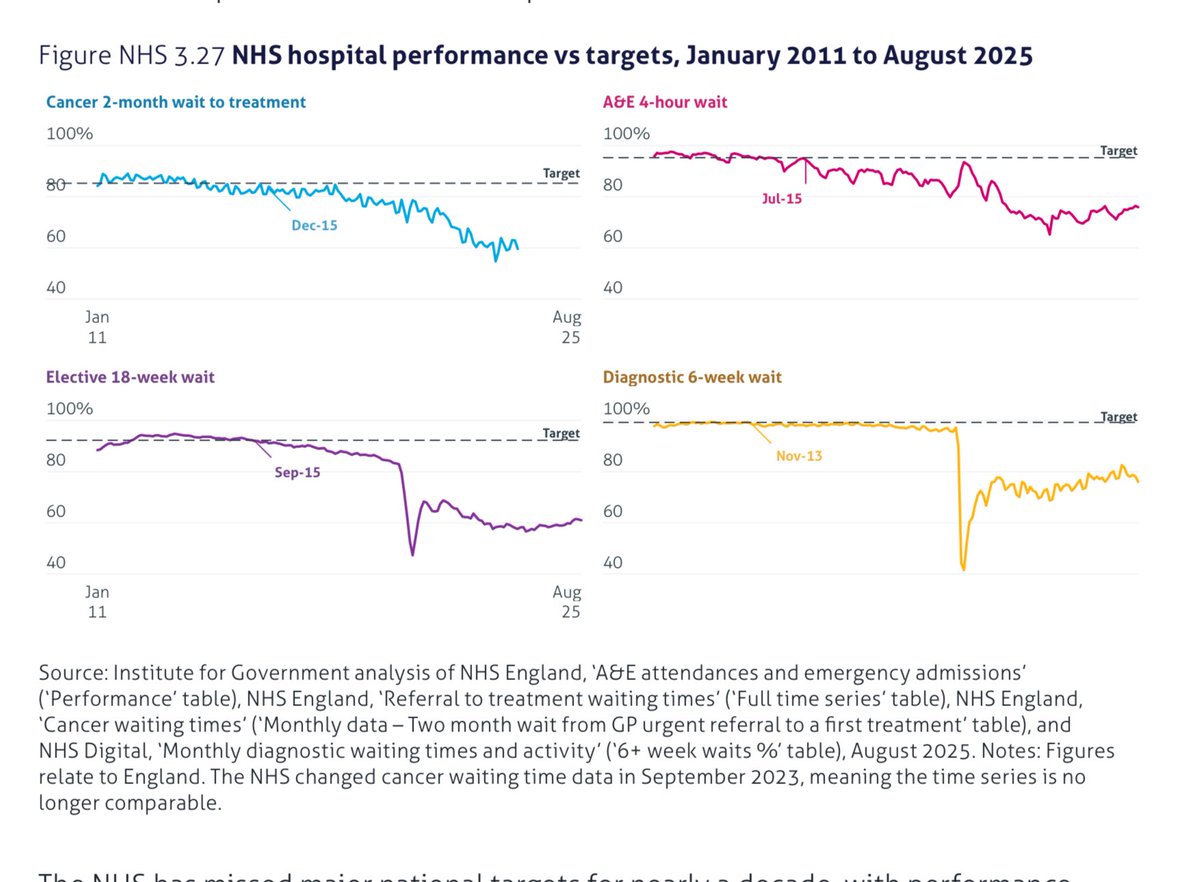
There have been many reasons why GP surgeries are struggling
Many negative comments
A lot of misinformation
But there are reasons for #GPCrisis
4/
Many negative comments
A lot of misinformation
But there are reasons for #GPCrisis
4/
https://twitter.com/drstevetaylor/status/1564154568090521600
There is a lot more work being done in community care
And demand is rising
5/

And demand is rising
5/
https://twitter.com/DrSteveTaylor/status/1578335397595475969


The GP workforce is ageing
The Government has failed to address the issues of retention
Pension Tax
No income increase since 2005
Increased workload & bureaucracy
6/
The Government has failed to address the issues of retention
Pension Tax
No income increase since 2005
Increased workload & bureaucracy
6/
https://twitter.com/drstevetaylor/status/1573674632925925376
We have to accept that funding across the NHS is not enough but the lack of investment in Primary Care leads inevitably to all the other parts struggling
10% of NHS budget spend on Primary Care
7/



10% of NHS budget spend on Primary Care
7/




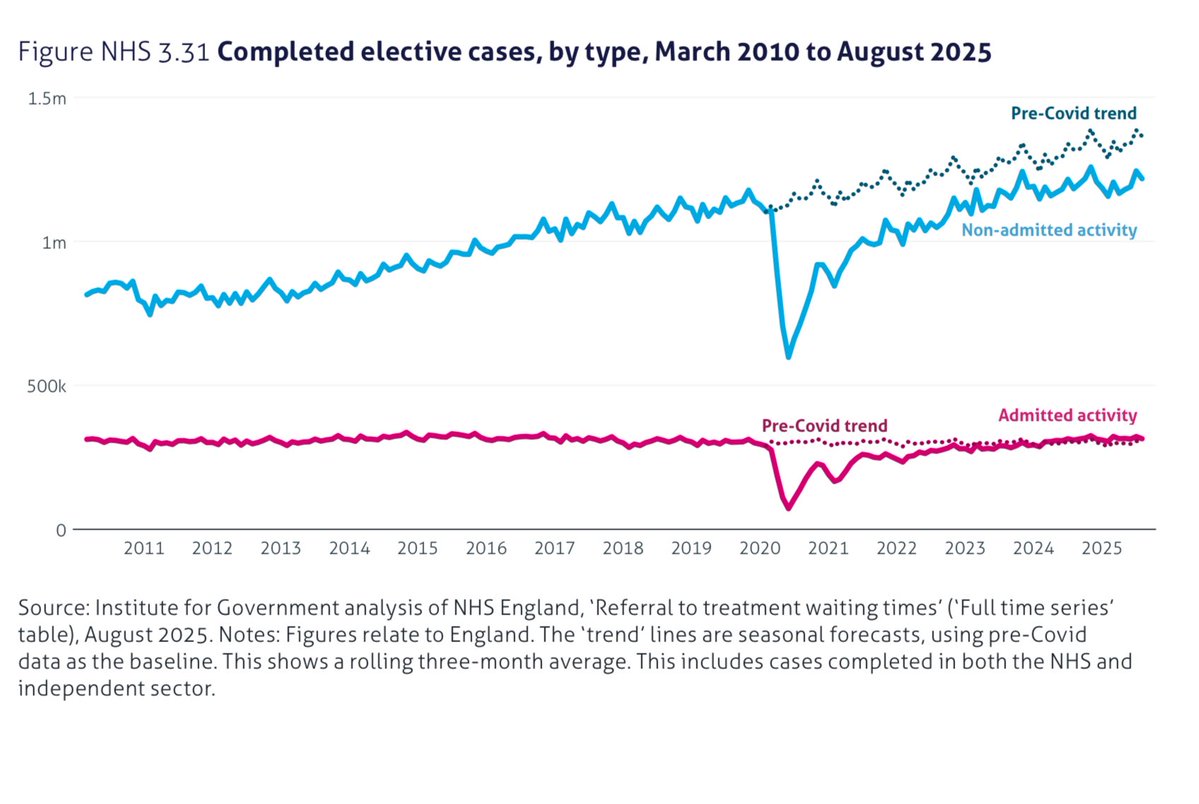
An overview of the NHS shows all parts are struggling
Investment is needed in most areas
I would argue that General Practice is outperforming with 10% of the budget (£8bn)
Given sufficient it would help solve the current crisis
8/
Investment is needed in most areas
I would argue that General Practice is outperforming with 10% of the budget (£8bn)
Given sufficient it would help solve the current crisis
8/
https://twitter.com/drstevetaylor/status/1582380861600636928
• • •
Missing some Tweet in this thread? You can try to
force a refresh