
1/ Step 1 - Don’t
👉Shut anything off
👉Touch the vent
👉Remove restraints
👉Pause sedation
if you have not explicitly asked permission to do so.
[This is a survival thing! For the pt… (and you 😉)]
A #tweetorial @medtweetorial about critical care things for #neurologists
👉Shut anything off
👉Touch the vent
👉Remove restraints
👉Pause sedation
if you have not explicitly asked permission to do so.
[This is a survival thing! For the pt… (and you 😉)]
A #tweetorial @medtweetorial about critical care things for #neurologists

2/
Vibe check for the #neurologists out there. Do you like doing ICU consults?
#MedEd #NeuroTwitter #NeuroTwitterNetwork #EmoryNCCTweetorials
Vibe check for the #neurologists out there. Do you like doing ICU consults?
#MedEd #NeuroTwitter #NeuroTwitterNetwork #EmoryNCCTweetorials
3/
Tip 1⃣: Induction meds for intubation have different hemodynamic profiles.
In emergent situations, explicitly tell whoever is intubating the patient’s BP goals.
For ex: AIS = ⬆️ BP good; induction with propofol (frequently = hypotension) is suboptimal.
Reminders are 🔑
Tip 1⃣: Induction meds for intubation have different hemodynamic profiles.
In emergent situations, explicitly tell whoever is intubating the patient’s BP goals.
For ex: AIS = ⬆️ BP good; induction with propofol (frequently = hypotension) is suboptimal.
Reminders are 🔑
4/
Tip 2⃣: many EDs are comfortable w/ peripheral pressors.
If an ischemic stroke patient drops their blood pressure & exam worsens in the ED: ask for pressor.
Don’t wait for a central line to start it.
Reasonable to target the BP they came in with or a 20% increase.
Tip 2⃣: many EDs are comfortable w/ peripheral pressors.
If an ischemic stroke patient drops their blood pressure & exam worsens in the ED: ask for pressor.
Don’t wait for a central line to start it.
Reasonable to target the BP they came in with or a 20% increase.
5/
Thinking:can that cause vasoconstriction of the cerebral arteries and maybe worsen CBF?
Is this dangerous?
Old (but a paper I love) suggests not: ahajournals.org/doi/10.1161/01…
Small trial: pubmed.ncbi.nlm.nih.gov/11342689/
Thinking:can that cause vasoconstriction of the cerebral arteries and maybe worsen CBF?
Is this dangerous?
Old (but a paper I love) suggests not: ahajournals.org/doi/10.1161/01…
Small trial: pubmed.ncbi.nlm.nih.gov/11342689/
6/
The 🗝️ here is that this only works for patients who would depend on collaterals. Often, these patients just need temporizing until they get a thrombectomy.
I get that this is trickier to do on floors.
So…HOB flat & bolus fluids?
⚠️There is not great evidence for this
The 🗝️ here is that this only works for patients who would depend on collaterals. Often, these patients just need temporizing until they get a thrombectomy.
I get that this is trickier to do on floors.
So…HOB flat & bolus fluids?
⚠️There is not great evidence for this
7/
*Some* patients may augment CBF with a flat trial: pubmed.ncbi.nlm.nih.gov/15851722/
But, there is an aspiration risk.
Trial has some flaws, I think it is convincing enough that we should *not* routinely lay patients flat “just because” that’s a protocol:
pubmed.ncbi.nlm.nih.gov/28636854/
*Some* patients may augment CBF with a flat trial: pubmed.ncbi.nlm.nih.gov/15851722/
But, there is an aspiration risk.
Trial has some flaws, I think it is convincing enough that we should *not* routinely lay patients flat “just because” that’s a protocol:
pubmed.ncbi.nlm.nih.gov/28636854/
8/
Bolus then? Interestingly, some lit suggest that the hemodynamic effect of a fluid bolus may be due to the temperature❄️!
From @pulmcrit 🙏about how blousing fluids is not the solution to all hemodynamic problems: emcrit.org/pulmcrit/bolus/
Cooling blanket anyone? 🤔🤷♀️
Bolus then? Interestingly, some lit suggest that the hemodynamic effect of a fluid bolus may be due to the temperature❄️!
From @pulmcrit 🙏about how blousing fluids is not the solution to all hemodynamic problems: emcrit.org/pulmcrit/bolus/
Cooling blanket anyone? 🤔🤷♀️
9/
That said all, there may be pts that do respond to fluid challenge so it’s not an unreasonable thing to try.
What is unreasonable? “Maintenance fluids”
Tip 3⃣: Maintenance fluids can have all kinds of deleterious side effects!
@neuro_intensive begs you to
That said all, there may be pts that do respond to fluid challenge so it’s not an unreasonable thing to try.
What is unreasonable? “Maintenance fluids”
Tip 3⃣: Maintenance fluids can have all kinds of deleterious side effects!
@neuro_intensive begs you to
10/
Quick summary of hemodynamic tips:
🗣️Communicate BP goals
💉Pressors are a more reliable way to achieve a hemodynamic target than fluids & HOB: ie perfusion dependent pts deserve a unit bed and very close monitoring!
🛑Stop maintenance fluids 🙏
Quick summary of hemodynamic tips:
🗣️Communicate BP goals
💉Pressors are a more reliable way to achieve a hemodynamic target than fluids & HOB: ie perfusion dependent pts deserve a unit bed and very close monitoring!
🛑Stop maintenance fluids 🙏
11/
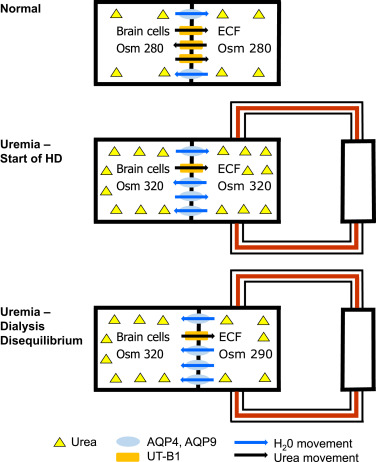
Tip 4⃣: Hemodialysis can kill people with brain pathology ! ☠️
Hemodialysis causes fluid shift (check out @ericlawso
w/ an ICP problem this can be enough to result in herniation 😱 pubmed.ncbi.nlm.nih.gov/33771393/
Tip 4⃣: Hemodialysis can kill people with brain pathology ! ☠️
Hemodialysis causes fluid shift (check out @ericlawso
https://twitter.com/EricLawson90/status/1456382546636312580) and thus can cause cerebral edema.
w/ an ICP problem this can be enough to result in herniation 😱 pubmed.ncbi.nlm.nih.gov/33771393/
12/
As a neurologist, if there is a patient with ESRD who has a new space occupying lesion (bleed, hydrocephalus, malignant stroke) – advocate for CRRT with Q1H neurochecks.
As a neurologist, if there is a patient with ESRD who has a new space occupying lesion (bleed, hydrocephalus, malignant stroke) – advocate for CRRT with Q1H neurochecks.
13/
Tip 5⃣: If you do get into an ICP crisis issue, a 3% infusion is not the solution🙏
Hyperosmolar therapy works by rapidly “dehydrating” the brain.
This depends on the fast creation of a gradient. An infusion will not create said gradient.
More: emcrit.org/emcrit/hyperos…
Tip 5⃣: If you do get into an ICP crisis issue, a 3% infusion is not the solution🙏
Hyperosmolar therapy works by rapidly “dehydrating” the brain.
This depends on the fast creation of a gradient. An infusion will not create said gradient.
More: emcrit.org/emcrit/hyperos…
14/
Mannitol can go through a filtered peripheral IV. New evidence that 23% HTS can too. If you want to use 3%, give as a bolus (250cc). You can even use code-cart hypertonic bicarb!
Whatever the solution, the goal is the rapid creation of a gradient.
Mannitol can go through a filtered peripheral IV. New evidence that 23% HTS can too. If you want to use 3%, give as a bolus (250cc). You can even use code-cart hypertonic bicarb!
Whatever the solution, the goal is the rapid creation of a gradient.
https://twitter.com/caseyalbin/status/1581244808336506882?s=42&t=fA1xK6yzlBDEBMIyXFJjEw
15/
Tip 6⃣: PLEX and CRRT are not mutually exclusive. If a patient needs CRRT but also needs PLEX, have a conversation with the critical care team about when it’s appropriate to alternate in the PLEX.
Or use a different induction immunotherapy if it’s a ½ dozen or the other.
Tip 6⃣: PLEX and CRRT are not mutually exclusive. If a patient needs CRRT but also needs PLEX, have a conversation with the critical care team about when it’s appropriate to alternate in the PLEX.
Or use a different induction immunotherapy if it’s a ½ dozen or the other.
16/
Bonus PLEX can be run through a peripheral line! Ask your PLEX team.
More about my love of PLEX here:
emcrit.org/emcrit/ivig-pl…
Bonus PLEX can be run through a peripheral line! Ask your PLEX team.
More about my love of PLEX here:
emcrit.org/emcrit/ivig-pl…
17/
Tip 7⃣: Respiratory therapy protocols sometimes exclude SBTs if patient isn’t “awake enough” to follow commands. The pt may be aphasic or neglectful o “less awake” but they can and *SHOULD* still be working on spontaneous breathing.
AC/VC isn't comfy, work on spontaneous.
Tip 7⃣: Respiratory therapy protocols sometimes exclude SBTs if patient isn’t “awake enough” to follow commands. The pt may be aphasic or neglectful o “less awake” but they can and *SHOULD* still be working on spontaneous breathing.
AC/VC isn't comfy, work on spontaneous.
18/
Tip 8⃣: Most of the time crit care providers are very attuned to the bowels… but it doesn’t hurt to remind your CC colleagues that most GBS patients develop ileus and need aggressive bowel reg.
Same thing for ⚡️status patients!⚡️
Not great for pt’s KUB to look like this⬇️
Tip 8⃣: Most of the time crit care providers are very attuned to the bowels… but it doesn’t hurt to remind your CC colleagues that most GBS patients develop ileus and need aggressive bowel reg.
Same thing for ⚡️status patients!⚡️
Not great for pt’s KUB to look like this⬇️

19/
Tip 9⃣: Weaning infusions:
It’s a pain to titrate down a small amount every hour.
Unless this is a very delicate patient, pick a more moderate dose change and adjust every 4-6 hours
(ie. asking to go down on Midazolam by 1mg q1hour creates extra work; consider 4q4)
Tip 9⃣: Weaning infusions:
It’s a pain to titrate down a small amount every hour.
Unless this is a very delicate patient, pick a more moderate dose change and adjust every 4-6 hours
(ie. asking to go down on Midazolam by 1mg q1hour creates extra work; consider 4q4)
20/
⚠️NOTE⚠️: This is not true for the patients with ICP issues who have required sedatives for crisis management… those patients need to be treated with extreme care, and sedative/temperature changes are best done in tiny increments!
⚠️NOTE⚠️: This is not true for the patients with ICP issues who have required sedatives for crisis management… those patients need to be treated with extreme care, and sedative/temperature changes are best done in tiny increments!
21/
Tip 🔟: The ICU is probably more comfortable with ketamine than most neurologists are. This is a great drug for refractory status!
Mostly well tolerated although can lead to metabolic acidosis & hemodynamic instability w/ prolonged, high dose use (+sometimes lots of saliva)
Tip 🔟: The ICU is probably more comfortable with ketamine than most neurologists are. This is a great drug for refractory status!
Mostly well tolerated although can lead to metabolic acidosis & hemodynamic instability w/ prolonged, high dose use (+sometimes lots of saliva)
22/
Finally, all of this can be summarized by a saying from a very wise colleague: “below the neck, there is a body.”
It is tempting to just focus on the brain - we all love it best🧠! But a holist view, especially for a complicated ICU patient, makes a huge difference in care
Finally, all of this can be summarized by a saying from a very wise colleague: “below the neck, there is a body.”
It is tempting to just focus on the brain - we all love it best🧠! But a holist view, especially for a complicated ICU patient, makes a huge difference in care
Thank you to @CajalButterfly @sigman_md and @feras_akbik who chipped in tips and peer reviewed! 🙏 love to hear other tips that people find helpful!😄 @namorrismd @drdangayach @aartisarwal @rkchoi @MicieliA_MD @a_charidimou @andrewyu8 @ShadiYaghi2 @SubinMatthews @bobvarkey
@neurologyrules @BuslKatharina @emcrit @EM_RESUS @JimSiegler @JayKinariwala @nickmmark @LyellJ @almuftifawaz @JayKinariwala @maness_caroline @zach_london @aszelikovich @Tracey1milligan @teachplaygrub @EmoryNeuroCrit @RoyStrowdMD @theABofPharmaC @AJWPharm
Oops @MedTweetorials didn’t link you in the first tweet cause I forgot the s… 🤦♀️
• • •
Missing some Tweet in this thread? You can try to
force a refresh











