
I wish it wasn't so, but surgical procedures disrupt tumors leading to hematological dissemination and the need for more treatment. Here, a randomized trial reports efforts to reduce this risk. jtcvs.org/article/S0022-… 1/ 🧵 

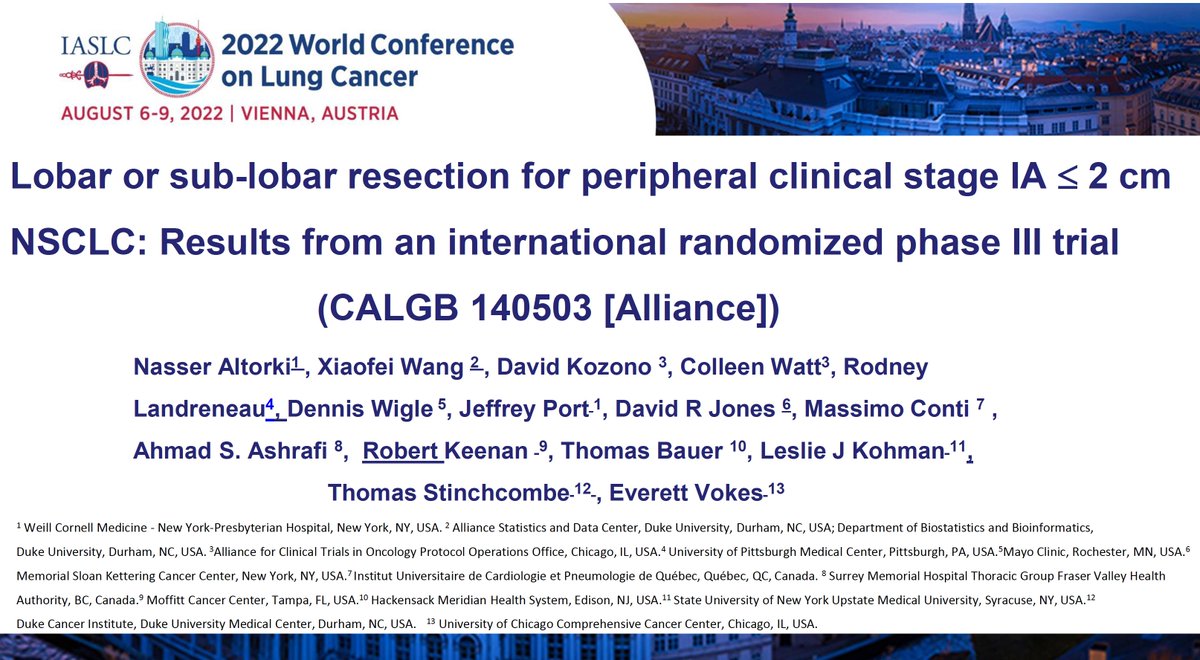
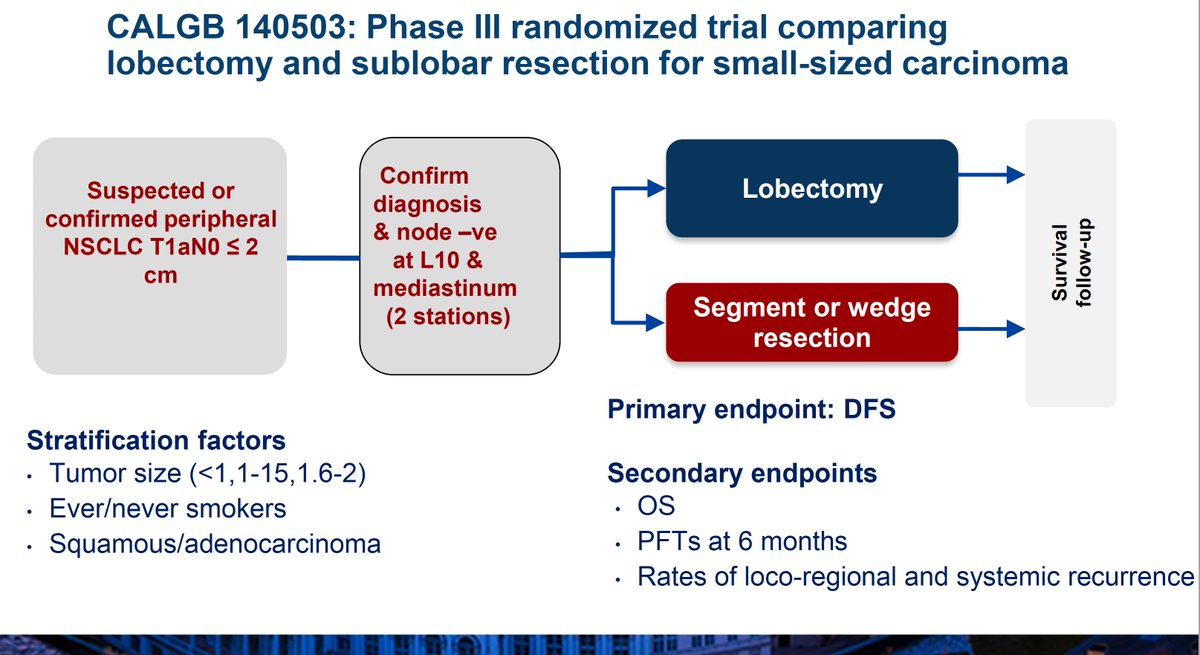
Sadly, contemporary trials show that surgical removal of even the smallest lung cancers (≤2 cm) cannot cure most patients. Note that neither of the DFS curves shows a sign of plateauing. @AltorkiNasser 





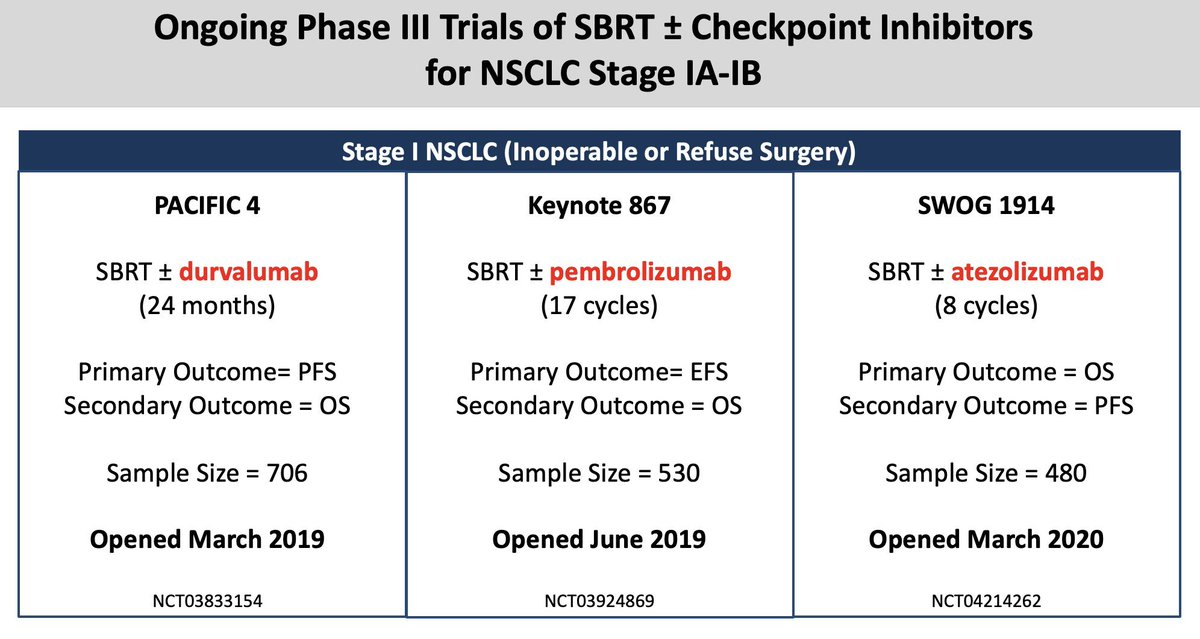
But what's the alternative? SBRT is promising, keeps the tumor in place, and might lead to better DFS and an earlier plateau. But even if it could, SBRT isn't always safer than surgery. Hence, we need to optimize surgical procedures for whenever its preferred. 







The other alternative to resecting and hoping for no further relapse is to give "just to be safe" postop adjuvant drug therapies. Unfortunately, this approach has yet to be demonstrated as an effective option for pts who undergo resection for tumors ≤2 cm.
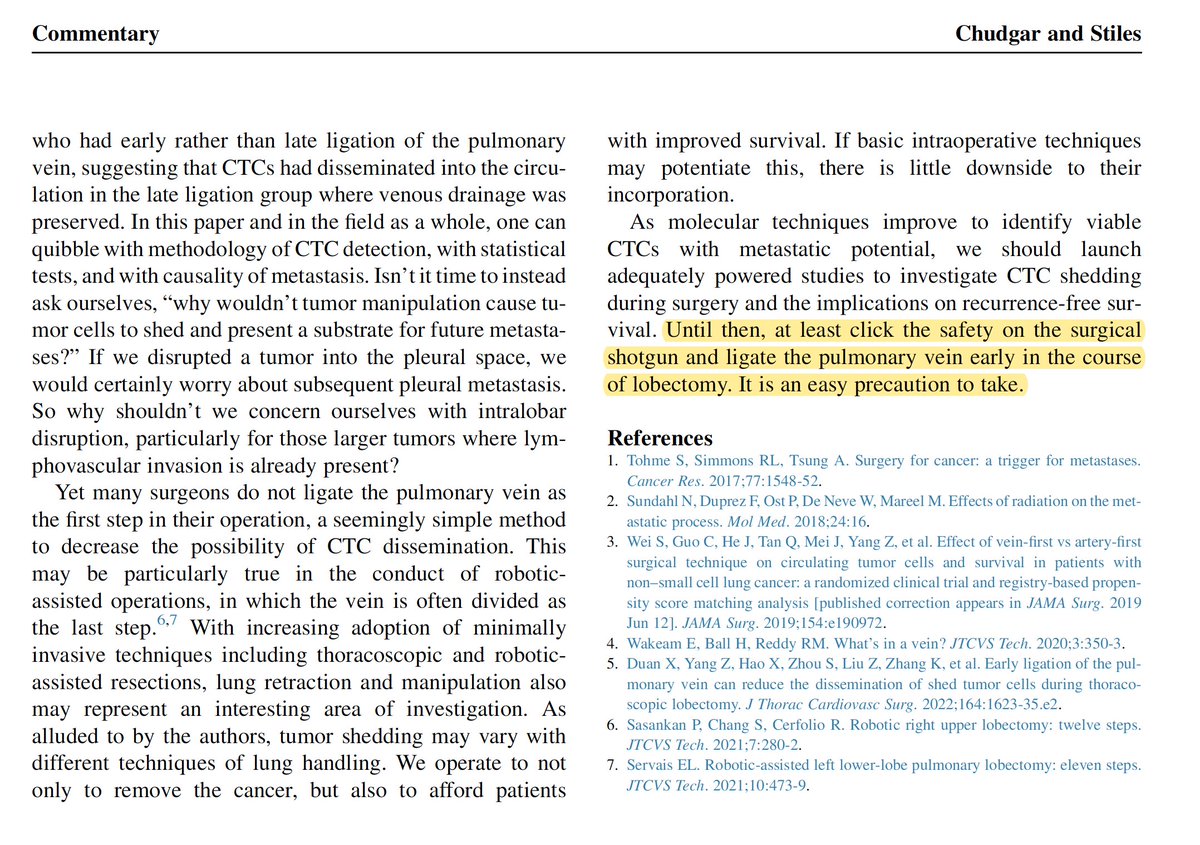
In a thoughtful commentary, @nchudgar and @BrendonStilesMD describe to their colleagues that, for now, there's an easy precaution to at least reduce the risk of tumor cell dissemination whenever surgical resection of lung tumors is performed. jtcvs.org/article/S0022-… 


Meanwhile, ongoing studies are evaluating alternatives to surgery altogether to find a single upfront treatment package that optimizes the likelihood of cure in patients with stage I NSCLC. @PeterGorayski 
Oh, and then there's this study too. vacsp.research.va.gov/CSP_2005/CSP_2… 

What else can we do to crush this disease once and for all? It's simple: demand more research for early-stage lung cancer! #LCAM
• • •
Missing some Tweet in this thread? You can try to
force a refresh







